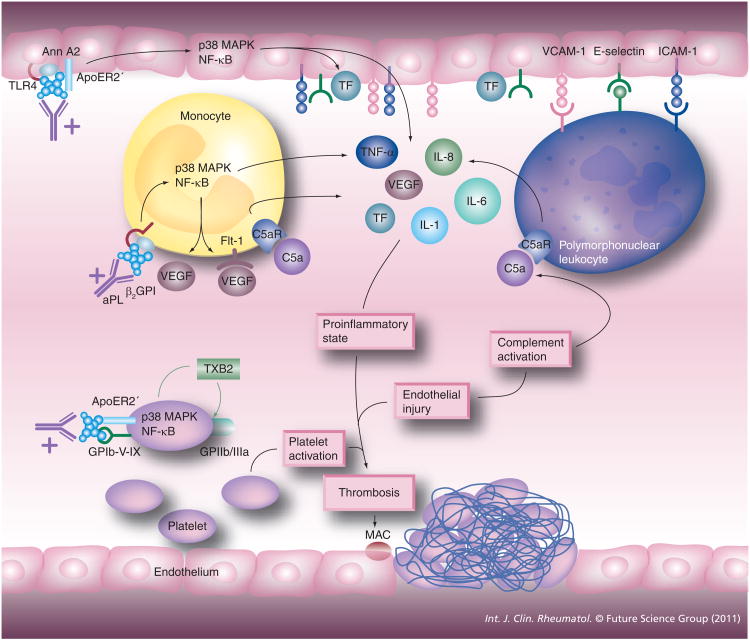
Figure 1. Cell activation in antiphospholipid syndrome.
aPL, including anti-β2GPI– β2GPI complexes, can activate platelets, endothelial cells and monocytes. Endothelial cell activation leads to the release of proinflammatory cytokines and increased leukocyte adhesion, making possible the activation of the polymorphonuclear leukocyte. Monocyte activation leads to the release of proinflammatory cytokines as well including TF, which can potentiate coagulation factor activation and ultimately fibrin production. Platelet activation leads to the release of thromboxane-B2, which potentiates the increased expression of GPIIb/IIIa, a major fibrinogen receptor. The net effect is the induction of a procoagulant state ultimately leading to thrombosis, occurring especially on the background of complement activation and endothelial injury due to infection and trauma.
β2GPI: β2-glycoprotein I; Ann: Annexin; aPL: Antiphospholipid; MAC: Membrane attack complex; NF-κB: Nuclear factor κB; TF: Tissue factor.