Abstract
Background:
We aimed to evaluate the timeliness of reporting of malaria surveillance system and understanding the existing problems.
Methods:
The timeliness of malaria surveillance system of Iran was evaluated in four provinces of Iran including Sistan & Baluchistan, Hormozgan, Kerman (as provinces with local malaria transmission) and Khuzestan (without local malaria transmission). In this descriptive-analytic cross-sectional study two levels of Primary Health Care service providers including first level (Health Houses) and second level (Urban or Rural Health care units) were evaluated with regard to reporting of malaria surveillance system.
Results:
Forms number 1 (87% reported within one day) and number 2 (reporting median: 2 days) are reported from first level to second level, and forms number 4 (median: 4 days), number 3 (median: 6 days), number 7 (median: 9 days), number 5 (median: 11 days) and number 6 (median: 19 days) are reported from second level to the third level respectively in a shorter time. Independent variables such as distance, local malaria transmission level, and case finding type, are the factors affecting the reporting delay.
Conclusion:
Reporting in the first level compared to the second level is done with lower delay. In the areas where there is a deadline set for reporting, reporting is done more timely. Whatever number of malaria cases is decreased, sensitivity and subsequently timeliness reduced. It is recommended that the studies of timeliness be done with sensitivity and usefulness analysis of surveillance system.
Keywords: Timeliness, Malaria, Surveillance system, Iran
Introduction
Timeliness is one of the main and important components of the surveillance systems, which indicates the speed (or time) of the steps, from acquiring information up to the action in a surveillance system. Surveillance consists of the collection, analysis, interpretation and dissemination of systematic information about a health-related event. The information is used in public health efforts aimed at reducing morbidity, mortality and health promotion (1). In fact, the obtained data from a surveillance system in its current information system will be the basis for decision making and the subsequent efforts (1, 2, 3). Now the very important point is that whether the obtained information from the surveillance system, is available in a timeliness manner for the users? This concept is interested in surveillance systems and in published literatures as the reporting timeliness (4–8).
Malaria surveillance system is among the structures that timeliness of information cycle has an extraordinary importance in it. In recent years we have witnessed a decline in malaria cases in Iran. So that, planning to eliminate malaria in the “Horizon Program of 2025” has been located in the agenda of the Iranian Ministry of Health since the beginning of 2010 (9). Entering the phase of pre-elimination, suggests that the burden of death or disease would not be significant in the country. The plan approach will be toward the action by focusing on the malaria foci centers too. Dealing with the epidemics of malaria has a double importance at this stage due to the presence of Iran in the unstable malaria region. In this program, timeliness action should be considered in subsequent events associated with malaria more than ever (9).Thus, the electronic reporting system in Iran has been created from the health centers of the townships to the province’s health centers and then to the center of disease management at national level (parallel to the start of the elimination of malaria). Obviously, the transfer time will be very short by using this electronic system of information transmission. But no action has been taken to collect data from more peripheral levels yet and consequently its performance is also questioned.
The present study has been designed and implemented accordingly to evaluate the timeliness of reporting of malaria surveillance system and understanding the existing problems.
Methods
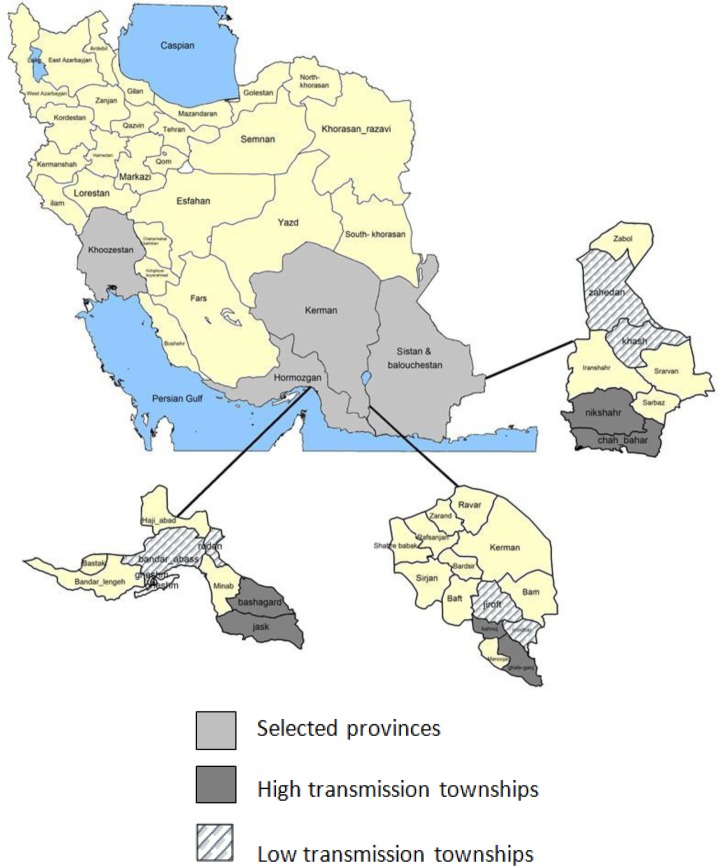
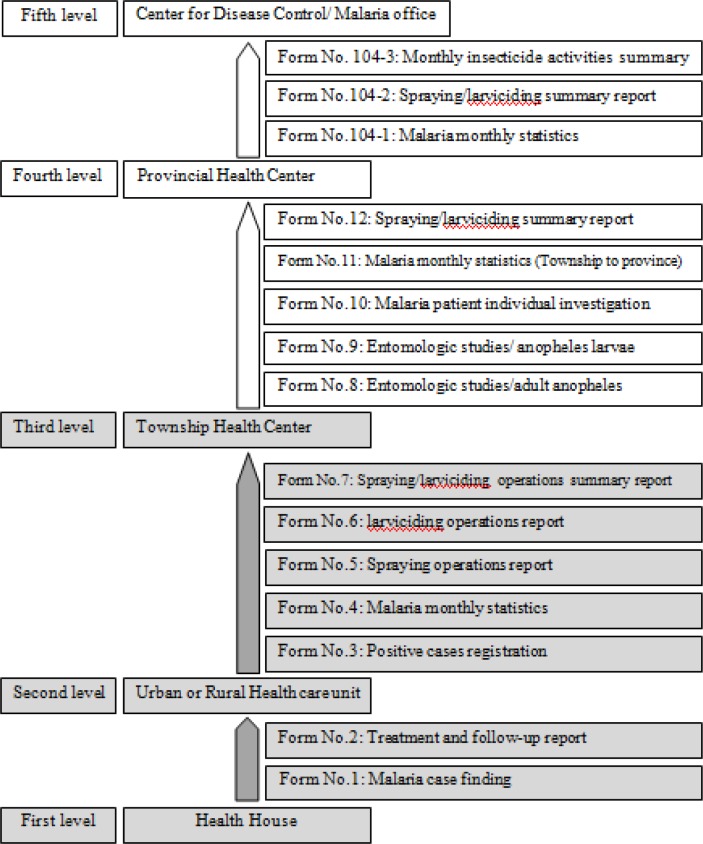
In this cross-sectional study, four provinces were assessed: the provinces of Sistan and Baluchestan, Hormozgan, Kerman (provinces with local malaria transmission) and Khuzestan (the province without local malaria transmission). In each province with local transmission, 4 townships were selected (2 townships with the highest incidence and 2 townships with a low incidence comparing to the townships of the same province). Those townships were selected in the Khuzestan province where they have reported positive cases of malaria during the previous year of conducting the study (Fig. 1). As it has been shown in Figure 2, the levels of delivering services and reporting in Iran health system (and also in the malaria surveillance system) are including in 5 levels.
Fig. 1:
The selected provinces (bigger picture) and the townships (in three smaller pictures) for study of timeliness of Malaria surveillance system
Fig. 2:
Reporting levels of Malaria surveillance system in Iran
Each of these levels has the task of providing services in its covered population, monitoring the performance of lower-level units and reporting to their higher levels. The most peripheral levels of this system are healthcare houses and bases. The places are responsible for providing services in rural and urban areas, respectively, under the supervision of the relevant Health Center. There are 2 forms in malaria surveillance system: the case finding form (Form No. 1) and the form of treatment and follow-up of positive cases (Form No. 2). Both forms, respectively, are completed and reported to higher levels immediately after detection of a positive case and after the end of follow-up and treatment. The second levels which are the urban and rural health centers, report the Forms number 3 – 7 to the township health center. Form No. 3 (registration of cases) will be reported to the township health center after the detection and receiving additional information about a malaria case, mainly at the end of each week. Form No. 4 (monthly statistics) at the end of each month, Form No. 5 (report of spraying operations) after each spraying operation (in areas where spraying operation was done), and Form No. 6 (report of the larviciding) at the end of each larviciding operation (in areas where larviciding operation was done), is completed and submitted. Form No. 7 (summary of spraying operations /larviciding) is sent after spraying and larviciding operations. In this study, the first to the second-level reporting and the second to the third level, have been assessed through the forms (which is displayed with darker color in Fig. 2).
So that all selected areas (in terms of reporting in the last 20 cases), were investigated in forms number 1 to 4 (case finding, treatment and follow-up cases, monthly statistics), and all the forms No. 5, No. 6 and No. 7 (report of spraying operations, the report of larviciding operations, summary of spraying and larviciding) which were reported in the level of townships. In the present study, the timeliness of malaria surveillance system was evaluated in the two reporting levels of the healthcare house / base (first level) to the level of health centers in rural / urban areas and reporting of health care centers (second level) to the township health center (third level) (Fig. 2).
The reason that we did not consider the upper level is that the data transmission from the township to the upper levels is already performed electronically by web. Therefore, the reporting to the upper levels is done (from the township level to the province and from the province health center to the Center for Diseases Management in MOHME) simultaneously and immediately after receiving information from lower levels since the beginning of 2010. Therefore, it was not possible to study the above mentioned levels by using the forms and it has been ignored.
The relationship between the independent variables (such as distance, the coverage of primary healthcare services, the covered population and ...) with the reporting method in Form No. 1 (patient finding) was performed by using the Chi-square and Fischer exact tests. Time of reporting the Forms of No. 2 to No. 7 were also analyzed as well as time to reporting with the survival analysis and Log rank test.
Results
The obtained data from the reviewed forms, were including 198 positive cases, in four provinces of Sistan and Baluchestan (41%, 81 cases), Hormozgan (35.5%, 71), Kerman (17.5%, 35) and Khuzestan (6%, 11). Table 1 indicates the distribution of the studied cases (in terms of the variables reviewed in this study). The results showed that from the total of 80 reported positive cases from the first level of services to the second level in Form No. 1 (case finding), 37 cases (46.2%) have been reported from the urban health bases and 43 cases (53.8%) from the healthcare houses to the related healthcare centers (level second).
Table 1:
Distribution of frequency of the reported cases on the basis of studied variables
| Variable | Categories | Frequency | Percentage |
|---|---|---|---|
| Local malaria transmission† | High | 96 | 48.5 |
| Low | 91 | 46 | |
| Clear | 11 | 5.5 | |
| The detection level of positive case‡ | First | 80 | 40.4 |
| Second | 109 | 55.1 | |
| Third | 9 | 4.5 | |
| Health care unit | Urban | 119 | 61 |
| Rural | 76 | 39 | |
| Case finding type†† | Active | 84 | 42.4 |
| Passive | 114 | 57.6 | |
| PHC coverage ratio (%) | 90=> | 58 | 32.8 |
| 90< | 119 | 67.2 |
The amount of local transmission of malaria in local malaria zones
The level of health services which the positive malaria case has been diagnosed at that level (Figure 2)
Method of diagnosis of positive cases, Active (by the visiting of the health officer), Passive (referring the individual to the health center)
This reporting in 87.5% cases (70 cases) has been carried out during one day and the remaining 12.5% of the cases (10 cases) in more than one day. Table (2) showed the result analysis of the reviewed independent variables relationship with the method of reporting of Forms No. 1 and 2.
Table 2:
Independent variables relationship with the timeliness of reporting from the first level to the second level of health services (house or base health care center to the township center) by using the Chi-square test and the Log Rank
| Variable | Categories | Case finding form (n=80) | Treatment form (n=80) | |||||
|---|---|---|---|---|---|---|---|---|
| Reported within one day (n= 70) | Reported longer than a day (n=10) | Total n =80 | P-Value† | Median | 95% Confidence interval | Statistics‡ | ||
| Total reporting time | - | 70(87.5) | 10 (12.5) | 80 | - | 2 | 1.1 to 2.9 | - |
| Province | Sistan& Balouchestan | 32 (86.5) | 5 (13.5) | 37 | 0.43 | 2 | 1.4 to 2.6 | χ2= 0.62 df= 1 P= 0.43 |
| Hormozgan | 34 (87.2) | 5 (12.8) | 39 | 3 | 2.1 to 3.9 | |||
| Kerman | 4 (100) | 0 (0) | 4 | 8 | - | |||
| Khuzestan | - | - | - | - | - | |||
| Local malaria transmission | High | 50 (87.7) | 7 (12.3) | 57 | 1 | 3 | 2.1 to 3.9 | χ2=0.66 df=1 P=0.42 |
| Low | 20 (87) | 3 (13) | 23 | 1 | 0.2 to 1.8 | |||
| Population covered by first level of health care | 650<= | 33 (84.6) | 6 (15.4) | 39 | 0.74 | 2 | 0.9 to 3.1 | χ2 =3.46 df= 1 P= 0.06 |
| 650> | 33 (89.2) | 4 (10.8) | 37 | 3 | 1.6 to 4.4 | |||
| Distance of first level from the second (Km) | 25<= | 39 (92.9) | 3 (7.1) | 42 | 0.18 | 2 | 0.9 to 3.1 | χ2= 2.87 df= 1 P= 0.09 |
| 25> | 30 (81.1) | 7 (18.9) | 37 | 2 | 0.5 to 3.5 | |||
| Case finding type | Active | 43 (89.6) | 5 (10.4) | 48 | 0.51 | 3 | 1.7 to 4.3 | χ2 = 4.12 df= 1 P= 0.04 |
| Passive | 27 (84.4) | 5 (15.6) | 32 | 2 | 1.4 to 2.6 | |||
| Parasite type | vivax | 67 (87) | 10 (13) | 77 | 1 | 2 | 1.1 to 2.9 | - |
| falciparum | 3 (100) | 0 (0) | 3 | - | - | |||
| PHC coverage ratio (%) | 90<= | 30 (81.1) | 7 (18.9) | 37 | 0.73 | 2 | 0.9 to 3.1 | χ2= 0.34 df= 1 P= 0.56 |
| 90> | 20 (87) | 3 (13) | 23 | 1 | 0.2 to 1.8 | |||
Chi-Square test has been performed/
Log-Rank test has been performed
As it can be seen in this table, none of the reviewed independent variables have shown a significant relationship with the reporting of these forms (Table 2).
Among the 80 patients (stated positively) on the first level (the last 20 cases reported in 2010), 72 cases (90%) were reported with the median time of 2 days (95% CI: 1.1 to 2.9 days) during the treatment form to the higher level (second level). Out of the non-reported 8 cases, 7 cases were still receiving the treatment and 1 case was not reported until the completion of data collection to a higher level (health center). There was a significant relationship in analyzing the relationship between the reviewed independent variables and the only case finding type (active or passive) with the method of reporting of this form. In fact, in those cases where the patients were admitted actively, this form has been completed and sent in longer times than the cases which were discovered passively (Table 2). Among the total of 189 positive cases diagnosed in the first and second level, 165 cases (87.3%) have been reported in the Form No. 3 (case registration form) from the second level to the third level (township health center). In 24 cases, there was no information reported to the township health center. These cases were included: 2 delayed cases in reporting on those townships where they were sent the information during the year (32 and 51 days), and there were also 22 un-reported cases in the townships that no case registration (Form No. 3) was performed during 2010. Indeed they had not reported to the related township health center and excluded the form from their self-reporting system at all. The relationship of independent variables associated with the method of reporting the Forms No. 3 to 7, was shown in Table 3.
Table 3:
Independent variables relationship with the timeliness of reporting from the second to the third level of providing health services (health center to township center)
| Variable | Categories | Positive cases registration form (n= 169) | Monthly statistics form (n= 111) | Spraying operations report form (n= 45) | larviciding operations report form (n= 30) | Spraying/ larviciding operations summary report form (n= 26) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Median | 95% Confidence interval | Statistics | Median | 95% Confidence interval | Statistics | Median | 95% Confidence interval | Statistics | Median | 95% Confidence interval | Statistics | Median | 95% Confidence interval | Statistics | ||
| Total reporting time | - | 6 | 3.8 to 8.2 | - | 4 | 3.6 to 4.4 | - | 11 | 7.7 to 14.3 | - | 19 | 16.3 to 21.7 | - | 9 | 7.1 to 10.9 | - |
| Province | Sistan&balouchestan | 8 | 2.4 to 13.6 | χ2 =1.83 df= 1 P= 0.40 |
5 | 4.4 to 5.6 | χ2 =17.9 df= 2 P< 0.001 |
10 | 7.4 to 12.6 | χ2=9.47 df=1 P= 0.002 |
19 | 17.6 to 20.4 | - | 7 | 6.4 to 7.6 | χ2=2.27 df=2 P= 0.32 |
| Hormozgan | 6 | 4.5 to 7.6 | 3 | 2 to 4.1 | 18 | 10.5 to 25.5 | 21 | - | 9 | 5.8 to 12.2 | ||||||
| Kerman | 0 | - | 2 | 0.5 to 3.5 | 0 | - | 4 | - | 9 | 1.0 to 17.0 | ||||||
| Khuzestan | - | - | 1 | - | - | - | 0 | - | - | - | ||||||
| Health care unit | Urban | 5 | 2.6 to 7.4 | χ2=1.48 df= 1 P= 0.22 |
4 | 3.2 to 4.8 | χ2=0.91 df= 1 P= 0.34 |
10 | 4.1 to 15.9 | χ2= 0.23 df= 1 P= 0.63 |
17 | 2.5 to 31.5 | χ2=2.11 df= 1 P= 0.15 |
9 | 6.1 to 11.9 | χ2=1.75 df=1 P= 0.19 |
| Rural | 10 | 7.7 to 12.3 | 4 | 3.6 to 4.4 | 11 | 7.4 to 14.6 | 20 | 17.5 to 20.5 | 8 | 6.1 to 9.9 | ||||||
| Local malaria transmission | High | 2 | 0.7 to 3.3 | χ2=18.41 df=1 P< 0.001 |
4 | 3.6 to 4.4 | χ2= 3.44 df= 1 P= 0.06 |
† | ||||||||
| Low | 14 | 9.4 to 15.6 | 3 | 2.0 to 4.0 | ||||||||||||
| Clear | - | - | 1 | - | ||||||||||||
| Population covered by second level of health system | 13000<= | 5 | 2.9 to 7.1 | χ2=0.08 df= 1 P= 0.77 |
4 | 3.6 to 4.4 | χ2=3.13 df= 1 P= 0.08 |
11 | 7.9 to 14.1 | χ2=0.006 df= 1 P= 0.94 |
20 | 17.8 to 22.2 | χ2=1.23 df=1 P= 0.27 |
9 | 7.3 to 10.7 | χ2 = 1.83 df= 1 P= 0.03 |
| 13000> | 6 | 0.9 to 11.1 | 3 | 2.0 to 4.0 | 14 | 2.8 to 25.2 | 19 | 3.2 to 34.8 | 27 | 0 to 59.0 | ||||||
| Distance of second level from the third (km) | 60< | 10 | 7.8 to 12.2 | χ2=2.15 df= 1 P= 0.14 |
3 | 2.1 to 3.9 | χ2=7.47 df= 1 P= 0.006 |
12 | 5.4 to 18.6 | χ2=4.37 df= 1 P= 0.04 |
16 | 0 to 48.1 | χ2=5.13 df= 1 P= 0.02 |
9 | 6.9 to 11.1 | χ2=0.52 df= 1 P= 0.471 |
| 60=> | 11 | 8.5 to 13.5 | 4 | 3.6 to 4.4 | 10 | 7.1 to 12.9 | 20 | 18.6 to 21.4 | 9 | 6.9 to 11.1 | ||||||
| Times of (spraying/larviciding) operations | First | ‡ | 11 | 8.5 to 13.5 | χ2=0.006 df= 1 P= 0.94 |
20 | 19.1 to 20.9 | χ2=6.53 df= 1 P= 0.01 |
7 | 1.9 to 12.1 | χ2=2.04 df=1 P= 0.15 |
|||||
| Second | 8 | 3.8 to 12.2 | 14 | 3.6 to 24.4 | 8 | 5.7 to 10.3 | ||||||||||
| Third | - | - | - | - | 15 | - | ||||||||||
| Fourth | - | - | - | - | 9 | - | ||||||||||
The spraying operations / larvicidingsessions were only performed in areas with local malaria transmission. The analysis of local malaria transmission level and reporting the forms of No. 5 to 7, have been ignored
The sessions of spraying and larviciding operations had no relation with the method of reporting the forms No. 3 and No. 4
As it can be seen in this table, the median time for reporting this form has been 6 days (95% CI: 3.8 to 8.2 days) respectively. The relationship is statistically significant in the only variable of the level of local malaria transmission (Table 3). Total of 111 patients were evaluated in reviewing the reporting method of Form No. 4 (monthly statistics), 110 cases (99%) were reported via this form the second level to the township health center (third level). 1 case has not been reported until the end of the study. As it can be seen in Table 3, the median time for reporting the cases was 4 days (95% CI: 3.6 to 4.4 days) from the beginning of each month. There was a significant relationship with the variables of the province and the distance between the township health centers and the health center with the method of reporting of this form (Table 3). The median time reported for 45 spraying operation reports (Form No. 5) was estimated versus 11 days (95% CI: 7.8 to 14.3 days) after the spraying operation. In Sistan-Baluchestan province, the data has been reported in significantly less time than Hormozgan province (P = 0.002). Reporting in the health centers which were in the greater distance from the township health centers had more timeliness (P = 0.04). The median reporting time of 19 days (95% CI: 16.3 to 21.7) was estimated after completing the larviciding operations, respectively, for the 30 numbers of reviewed Form No. 6 (larviciding operation). Thus, the larviciding operations have been reported in less time significantly in the second session than the first time (P = 0.011). The reporting have been done in less time in the closer health centers to the township health center (P = 0.023). The median reporting time of 9 days (95% CI: 7.1 to 10.9) after completing the spraying operations / larviciding was also estimated in the 24 reported forms (Form No. 7) in the studied township health centers, respectively. The health centers with less covered population have reported in less time than the others with larger population (P = 0.028). It should be noted that Table 3 summarized the results of statistical analysis between the independent variables with reporting the Forms No. 3 to 7 (which were reported from the second level to the third level).
Discussion
Timeliness is among the key elements of an efficient surveillance system. Malaria surveillance system has been found a special importance by implementing programs to eliminate malaria in Iran up to 2025. Unfortunately, despite the importance of this topic and the proposed framework for the evaluation of surveillance systems in America (by the Centers for Disease Control and Prevention) which was clearly focused on the issue of timeliness (1).
But the published literatures to assess in the field of timeliness of surveillance systems, and especially malaria, are very little. Most of the published cases have been focused to detect and treat the cases rather than to focus on reporting and circulation of information in surveillance systems (10–14). Moreover, the few published articles due to the differences in reporting their health systems are not easily comparable with the present study. The findings showed that the Form No. 1 (87% reported during the same day), Form No. 2 (median 2 days) from the first to the second level, Form No. 4 (median 4 days), Form No. 3 (median 6 days), Form No. 7 (median 9 days), Form No. 5 (median 11 days) and Form No. 6 (median 19 days) have been reported in less time from the second level to the third level, respectively. As mentioned earlier form No. 1, has been reported in less time than the other forms. Whereas malaria is among the diseases which are subject to immediate reporting (telephone reporting) and regarding to the implementation of elimination program, the sensitivity is high for reporting the cases all around 24 hours. Therefore, such kind of reporting was not unexpected. However, the median time of reporting malaria has been estimated 10 days in the paper reporting system of the Netherlands. This value has been reduced to 2 days after the installation of electronic system. Another study which was conducted in the state of Colorado in the United States of America has been indicated that in the database of Tri-County Health Department (TCHD) 25% and in Colorado 35% of the diseases which are subject to reporting, will be reported within 24 hours (7, 8). There was no significant relationship between the method of reporting this form (form NO.1) and none of the variables investigated in reviewing the possible factors associated in affecting case finding reporting form. This can be affected by the lack of reported cases in more than one day and finally the lack of cases in the layers of independent variables. The study findings showed that in cases where the case finding adopted as an inactive (passive) case, the form of treatment (after the treatment) has been reported much earlier. The observed results can be explained by this fact that those who were discovered as a passive case, mainly referred to the health centers for diagnosis by themselves. They ultimately have been more willing to receive and complete their treatment. Therefore the tracking has been done in a timely manner and the report was also timeliness. In the second level of reviewing the reporting method of health care providers (health centers) to the third level (township health center), this study showed that the forms No. 4, No. 3, No. 7, No. 5 and No. 6 have been reported in less time. Among the important factors in the method of reporting at this level, there was a significant relationship between the time required for reporting the forms No. 4, No. 5 and No. 6 and the distance of the health centers to the township health center. Except for Form No. 5, in the two other cases (No. 4 and No. 6), the farther away centers had been submitted their reports to the township health center in a longer period of time than the closer centers. Another influential factor in the second level of reporting was the effect of the province as it has been mentioned in the results section. Form No. 4, respectively, has been reported more timely in the provinces of Kerman, Hormozgan and Sistan-Baluchestan. As far as Form No. 5 in the province of Sistan-Baluchestan province has been reported in less time than the Hormozgan province. This difference could be due to differences in process and performance of reporting in the provinces. Another reason for timelier reporting of Form No. 4 than the other forms of second level was its regular reporting at the end of each month and up to the fifth day of the next month, which the report has been sent from all of health centers to the township health center. So that it was mentioned in the results section, the reporting of Form No. 3 (case registration) is influenced by the level of local malaria transmission. This form in areas with a high rate of local malaria transmission has been reported in less time than the areas with a low local transmission. Such perceptions can be made that the sensitivity to the timely reporting in areas with local transmission of malaria is less than those areas with high local transmission level. Therefore, the case registration form has been reported in a longer period of time to the township health center too. On the contrary to what it was expected, that Form No. 3 was reported in a less period of time than the monthly statistics report (especially in areas with low local transmission), it has been reported in a non-uniform manner and without any fixed schedule. It has been sent weekly in some townships, monthly in some others and without having any specific process in the others. Some townships did not report it at all. A similar situation also was existed for Form No. 7. In some investigated townships and probably due to the parallel functioning of the Form No. 5 and 6, they have not been reported. The population covered by the health centers and spraying operations / larviciding sessions were the other factors which had a significant relationship with the reporting of forms No. 6 and 7. Form No. 7 in health centers with less covered populations and Form No. 6 in the second session of larviciding operations have been reported in less time. However, it is not possible to realize the establishment of a clear relationship between these variables and forms No. 6 and No. 7, due to the shortage of sample size in the layers of the mentioned independent variables.
Conclusion
Eventually, what it was achieved in the present study suggested that reporting on malaria surveillance system in Iran is done in less time from the first level to the second level of providing the services. The forms have been reported as well as more timely in the regions where the sensitivity for timely reporting of cases and forms by the system were high and reporting deadlines were set for them. Finally, whatever the numbers of malaria cases have been reduced in these areas, the sensitivity (proportion of cases the disease is diagnosed by the health care surveillance system) and subsequently the timeliness of reporting in their surveillance system was reduced. This point coupled with the lack of reporting of health centers that have not had positive cases, are indicating the importance of zero-reporting of the cases in pre-elimination and elimination stages.
Recommendations
According to the study findings, it is suggested to pay more attention to the timeliness of reporting in malaria surveillance system, especially in the second level of providing the healthcare services. A certain deadline should be determined for reporting the forms for each of the first and second levels due to their usages. The electronic reporting system will be developed by creating the necessary infrastructures and can be used at the health centers. The discovery of zero-reporting in all of the involved units and reporting of the malaria cases is important. Due to the importance of awareness about using the gained information in the surveillance system, it is recommended the studies of timeliness assessment will be performed with the analysis of surveillance system usefulness. One of the limitations of this study was the lack of access to the information of those townships which was not possible to review the method of their reporting due to the lack of positive cases and non-reporting of zero cases (zero reporting). According to the observed relationship between timeliness of surveillance system and its sensitivity, it is also recommended to study about the sensitivity of the surveillance system in addition to the study about the timeliness.
Ethical considerations
Ethical issues (Including plagiarism, Informed Consent, misconduct, data fabrication and/or falsification, double publication and/or submission, redundancy, etc) have been completely observed by the authors.
Acknowledgments
Hereby, this is to thank and appreciate the assistance of Ms. Faraji in the Department of Malaria Control and also the efforts of respected colleagues of the Deputy of Health in the provinces of Sistan-Baluchestan, Hormozgan, Kerman and Khuzestan (especially Mr. Mohammad Sakeni, Mr. Asadollah Ahmadi, Dr. Reza Safari, Mr. Gholamreza Momeni and Ms. Bigdeli). Also we are thankful for collaborations of Mr. Sarani for Geographical Information System maps. This study was the master’s thesis of Mr. Hossein Akbari in the School of Public Health at Tehran University of Medical Sciences that has been supported financially for it. The authors declare they do not have any conflict of interest.
References
- 1.Centers for Disease Control and Prevention Updated guidelines for evaluating public health surveillance systems. MMWR. 2001;50:1–35. [PubMed] [Google Scholar]
- 2.Framework for Program Evaluation in Public Health U.S. Department Of Health & Human Services. 1999 Report No.: 48/ No. RR-11. [Google Scholar]
- 3.Framework and Tools for Evaluating Health Surveillance Systems Health Surveillance Coordinating Committee (HSCC), Population and Public Health Branch Health Canada, 2004.
- 4.Jajosky RA, Groseclose SL. Evaluation of reporting timeliness of public health surveillance systems for infectious disease. BMC Public Health. 2004;4(29) doi: 10.1186/1471-2458-4-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Domínguez A, Coll J, Fuentes M, Salleras L. Timeliness of notification in infectious disease cases. Public Health Rep. 1992;107(4):474. [PMC free article] [PubMed] [Google Scholar]
- 6.Klevens RM, Fleming PL, Li J, Gaines CC, Gallagher K, Schwarcz S, Karon JM, Ward JW. The completeness, validity, and timeliness of AIDS surveillance data. Ann Epidemiol. 2001;11(7):443–9. doi: 10.1016/s1047-2797(01)00256-3. [DOI] [PubMed] [Google Scholar]
- 7.Vogt RL, Spittle R, Cronquist A, Patnaik JR. Evaluation of the timeliness and completeness of a Web-based notifiable disease reporting system by local health department. J Public Health Managt Pract. 2006;12(6):540. doi: 10.1097/00124784-200611000-00007. [DOI] [PubMed] [Google Scholar]
- 8.Panackal AA, Múikanatha NM, Tsui FC, McMahon J, Wagner MM, Dixon BW, et al. Automatic electronic laboratory-based reporting of notifiable infectious diseases. Emerg Infect Dis. 2002;8(7):685. doi: 10.3201/eid0807.010493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Malaria elimination in IR Iran (Horizon 1404) 2010. Islamic Republic of Iran, CDC, MOH&ME; (In Farsi)
- 10.Yimer S, Bjune G, Alene G. Diagnostic and treatment delay among pulmonary tuberculosis patients in Ethiopia: a cross sectional study. BMC Infect Dis. 2005;5(1):112. doi: 10.1186/1471-2334-5-112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bassili A, Seita A, Baghdadi S, Al Absi A, Abdilai I, Agboatwalla M, et al. Diagnostic and treatment delay in tuberculosis in 7 countries of the Eastern Mediterranean region. Infect Dis Clin Prac. 2008;16(1):23. [Google Scholar]
- 12.Rajeswari R, Chandrasekaran V, Suhadev M, Sivasubramaniam S, Sudha G, Renu G. Factors associated with patient and health system delays in the diagnosis of tuberculosis in South India. Intl J Tuberc Lung Dis. 2002;6(9):789–95. [PubMed] [Google Scholar]
- 13.Chalumeau M, Holvoet L, Chéron G, et al. Delay in diagnosis of imported Plasmodium falciparum malaria in children. Eur J Clin Microbiol Infect Dis. 2006;25(3):186–9. doi: 10.1007/s10096-006-0105-3. [DOI] [PubMed] [Google Scholar]
- 14.Booth CM, MacLean JD. Knowledge, treatment-seeking, and socioeconomic impact of malaria on the Essequibo Coast of Guyana. MJM. 2001;6(1):17–25. [Google Scholar]