Abstract
The optimal surgical management of patients with concomitant abdominal aortic aneurysm (AAA) and gastrointestinal malignancy remains controversial. A 79 year-old man who presented with hematemesis was found to have advanced gastric cancer concomitant with infrarenal AAA. The patient underwent simultaneous endovascular aneurysm repair (EVAR) and distal gastrectomy. The postoperative course was uneventful. The present case illustrates the clinical utility of EVAR for the high-risk patient with concomitant AAA and gastrointestinal malignancy.
Keywords: abdominal aortic aneurysm; endovascular aneurysm repair; gastric cancer
Introduction
In recent years, the extended average life span has brought a high rate of malignancies associated with cardiovascular diseases. In particular, the incidence of gastrointestinal malignancies concomitant with abdominal aortic aneurysm (AAA) has also increased. Although cancer progression and aneurysmal rupture are both life-threatening events in patients with these clinical entities, current treatment strategy for this condition remains controversial.
We report a successful case of simultaneous endovascular aneurysm repair (EVAR) and distal gastrectomy for AAA and advanced gastric cancer.
Case Report
A 79 year-old man was admitted to a general hospital for the investigation of sudden hematemesis. He was noted to be suffering from general fatigue and appetite loss with 5 kg weight loss in a month. Upper gastrointestinal examination with contrast medium revealed a mass, 55 × 50 mm in size, on the anterior wall of the gastric antrum, and gastrointestinal fiberscopy showed a hemorrhagic tumor compatible with a Bormann type III gastric cancer, and the bleeding was successfully stopped with an endoscopic hemoclip (Fig. 1). He was given a blood transfusion and recovered smoothly. A biopsy specimen demonstrated moderately to poorly differentiated adenocarcinoma.
Fig. 1.
Gastrointestinal fiberscopy revealed a hemorrhagic tumor compatible with a Borrman type III gastric cancer on the anterior wall of the gastric antrum. The bleeding was successfully stopped with an endoscopic hemoclip.
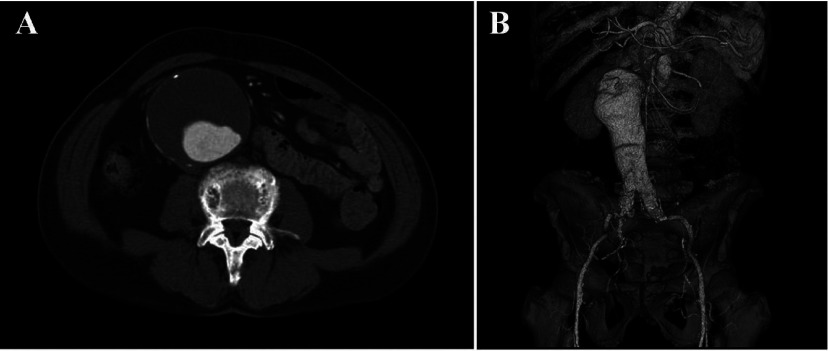
Computed tomography (CT) revealed a massive infrarenal AAA that measured 81 mm in maximum diameter (Fig. 2A). 3-dimensional computed tomography (3D-CT) showed the fusiform AAA with severe angulated proximal neck (Fig. 2B). We diagnosed the disease as advanced gastric cancer concomitant with AAA. Then he was referred to our institution for the operation of both lesions.
Fig. 2.
A: Contrast-enhanced computed tomography (CT) revealed a huge infrarenal abdominal aortic aneurysm (AAA) that measured 81 mm in maximum diameter.
B: 3-dimensional computed tomography (3D-CT) showed the fusiform AAA with a severe angulated proximal neck.
On physical examination, his conjunctivae were pale, but not icteric. A pulsating mass was palpated in his abdomen. Laboratory tests showed renal dysfunction with an elevated serum creatinine level (1.25 mg/dl). After we had discussed the surgical management including one or two-stage operation and open versus endovascular aneurysm repair (EVAR), we decided to perform the simultaneous EVAR and gastrectomy.
Under general anesthesia, bilateral common femoral arteries were exposed through inguinal incisions.A 28 × 12 mm × 18 cm bifurcated Gore-Tex (Excluder) stent graft was chosen. The main body of the system was inserted using through the left common femoral artery into the position just below the left renal artery. After optimal position was confirmed by aortography, the main body was deployed successfully. Then both graft limbs were deployed uneventfully. At the end, aortography confirmed type I endoleak. Therefore, a proximal aortic extension (aortic extender 28 × 30 mm), used to seal the angulated proximal neck, repaired the endoleak. Thereafter a median-laparotomy was performed. The gastric cancer invaded the transverse mesocolon and middle colic artery. A distal gastrectomy with systemic lymph node dissection was performed.
A postoperative 3D-CT on day 7 confirmed a patent endovascular graft in a good position without endoleaks (Fig. 3). The postoperative course was uneventful, and he was discharged on postoperative day 36.
Fig. 3.
Postoperative 3D-CT confirmed a patent endovascular graft in a good position without endoleaks.
Discussion
Although the incidence of patients presenting with concomitant AAA and gastric cancer is low, current treatment strategies in patients with both lesions remains controversial.1–4) The most important and difficult decision to make is whether to operate on the malignant lesion first, the AAA first, or both simultaneously. The decision-making may depend on many variables, including surgeon’s experience and preference, local expertise, aneurysm size, and type and stage of cancer. As Szilagyi stated in 1967,1) it is most important to assess the absolute indications for urgent surgical treatment of each lesion, being a high chance of aneurysm rupture, and such coexistent complications as hemorrhage, obstruction or perforation for the cancer. It is clear that the lesion which has the most dangerous complications should be operated on first.
The use of simultaneous operations for both lesions has several advantages. Risks accompanying total anesthesia, such as pneumonia or drug-induced complications, can be eliminated. Disease progression of the untreated lesion can be prevented. Surgeons have to keep in mind that there is a potential for aneurysm rupture if AAA resection is delayed by staged procedures. Furthermore, the anxiety of patients who are facing two life-threatening lesions is resolved at one time. On the other hand, the major disadvantage of simultaneous operation is the risk of prosthetic graft infection which may result in severe complications. In the present case, we selected the simultaneous operation because of the advanced hemorrhagic cancer and the high possibility of aneurysm rupture. We evaluated that the patient may be unable to tolerate a two-stage operation because of his advanced age and poor general condition.
The evolution of vascular endografts and the reported efficacy of EVAR provide an alternative method for treating complex and high-risk patients with acceptable mortality rate.5–7) EVAR results in early recovery and a shorter convalescence compared with open graft replacement. This modality offers potential treatment benefits in patients with suitable anatomy who have concomitant gastrointestinal malignancy.8–10) Herald et al. first reported the case of synchronous AAA and colorectal cancer treated entirely by minimally invasive surgery without laparotomy.11) Since then, several reports have been described simultaneous EVAR and abdominal cancer resection.12–14) However, almost all of those reports were undergoing a resection for colorectal cancer. While our present case was a high-risk gastric cancer patient complicated with AAA, so simultaneous EVAR and distal gastrectomy were performed, and a satisfactory outcome was obtained. EVAR should be considered the treatment of choice in high-risk patients, taking into account, however, that this treatment is not always feasible in all cases and that in patients with a normal life-expectancy it may not always be the right choice. Thus, a preoperative evaluation including a psychiatric assessment, especially in aged patients, should be carefully conducted when selecting the appropriate surgical procedure.
In conclusion, we successfully performed simultaneous EVAR and distal gastrectomy in a patient with concomitant AAA and advanced gastric cancer. EVAR is a safe and effective treatment for high-risk patients with a relatively low procedure-related morbidity and no mortality.
Disclosure Statement
The authors declare that they have no competing interests.
References
References
- 1.Szilagyi DE, Elliott JP, Berguer R. Coincidental malignancy and abdominal aortic aneurysm. Problems of management. Arch Surg 1967; 95: 402-12 10.1001/archsurg.1967.01330150078012 [DOI] [PubMed] [Google Scholar]
- 2.Komori K, Okadome K, Funahashi S.Surgical strategy of concomitant abdominal aortic aneurysm and gastric cancer. J Vasc Surg 1994; 19: 573-6 [DOI] [PubMed] [Google Scholar]
- 3.Morris HL, da Silva AF. Co-existing abdominal aortic aneurysm and intra-abdominal malignancy: reflections on the order of treatment. Br J Surg 1998; 85: 1185-90 10.1046/j.1365-2168.1998.00852.x [DOI] [PubMed] [Google Scholar]
- 4.Matsumoto K, Nakamaru M, Obara H.Surgical strategy for abdominal aortic aneurysm with concurrent symptomatic malignancy. World J Surg 1999; 23: 248-51 10.1007/PL00013189 [DOI] [PubMed] [Google Scholar]
- 5.EVAR trial participants. Endovascular aneurysm repair versus open repair in patients with abdominal aortic aneurysm (EVAR trial 1): randomised controlled trial. Lancet 2005; 365: 2179-86 10.1016/S0140-6736(05)66627-5 [DOI] [PubMed] [Google Scholar]
- 6.Lederle FA, Freischlag JA, Kyriakides TC.Outcomes following endovascular vs open repair of abdominal aortic aneurysm: a randomized trial. JAMA 2009; 302: 1535-42 10.1001/jama.2009.1426 [DOI] [PubMed] [Google Scholar]
- 7.United Kingdom EVAR Trial Investigators, Greenhalgh RM, Brown LC, et al. Endovascular versus open repair of abdominal aortic aneurysm. N Engl J Med 2010; 362: 1863-71. 10.1056/NEJMoa0909305 [DOI] [PubMed] [Google Scholar]
- 8.Lee JT, Donayre CE, Walot I.Endovascular exclusion of abdominal aortic pathology in patients with concomitant malignancy. Ann Vasc Surg 2002; 16: 150-6. 10.1007/s10016-001-0151-3 [DOI] [PubMed] [Google Scholar]
- 9.Prusa AM, Wolff KS, Sahal M.Abdominal aortic aneurysms and concomitant diseases requiring surgical intervention: simultaneous operation vs staged treatment using endoluminal stent grafting. Arch Surg 2005; 140: 686-91 10.1001/archsurg.140.7.686 [DOI] [PubMed] [Google Scholar]
- 10.Porcellini M, Nastro P, Bracale U.Endovascular versus open surgical repair of abdominal aortic aneurysm with concomitant malignancy. J Vasc Surg 2007; 46: 16-23 10.1016/j.jvs.2006.09.070 [DOI] [PubMed] [Google Scholar]
- 11.Herald JA, Young CJ, White GH.Endosurgical treatment of synchronous rectal cancer and abdominal aortic aneurysm, without laparotomy. Surgery 1998; 124: 932-3 10.1016/S0039-6060(98)70021-2 [DOI] [PubMed] [Google Scholar]
- 12.Kiskinis D, Spanos C, Melas N.Priority of resection in concomitant abdominal aortic aneurysm (AAA) and colorectal cancer (CRC): review of the literature and experience of our clinic. Tech Coloproctol 2004; 8: s19-21 10.1007/s10151-004-0101-5 [DOI] [PubMed] [Google Scholar]
- 13.Rivolta N, Piffaretti G, Tozzi M.Management of simultaneous abdominal aortic aneurysm and colorectal cancer: the rationale of mini-invasive approach. Surg Oncol 2007; 16: S165-7. 10.1016/j.suronc.2007.10.011 [DOI] [PubMed] [Google Scholar]
- 14.Bali CD, Harissis H, Matsagas MI. Synchronous abdominal aortic aneurysm and colorectal cancer. The therapeutic dilemma in the era of endovascular aortic aneurysm repair. J Cardiovasc Surg (Torino) 2009; 50: 373-9. [PubMed] [Google Scholar]