Abstract
Background
Social support may be associated with HF self-care; however, the mechanisms are not well understood. We examine the association between perceived support and self-care behaviors and whether self-care confidence mediates these relationships.
Methods
Cross-sectional survey of HF patients seen in outpatient clinic settings. Our outcome (HF self-care maintenance and self-care management) and mediator (HF self-care confidence) variables were assessed using the Self-Care of Heart Failure Index. Perceived emotional/informational support assessed using the Medical Outcomes Study social support survey. We performed regression analyses to examine associations between perceived support and HF self-care behaviors. Mediation analysis was performed according to Baron & Kenny method.
Results
We surveyed 150 HF patients (mean age 61 yrs; 51% female; 43% African Americans). More emotional/informational support was associated with better self-care maintenance (β=0.13, p=0.04). More emotional/information support was associated with better self-care management (β= 0.23, p=0.04) in unadjusted, but not adjusted analysis (β= 0.20, p=0.10). Self-care confidence mediates the association between perceived support and self-care maintenance (percent change in β coefficient was 32%) and management (percent change in β coefficient was 20%).
Conclusion
Perceived emotional/informational support is associated with better self-care maintenance and possibly better self-care management. Greater self-care confidence is one mediating mechanism.
Keywords: Heart Failure, Social Support, Self-care behaviors
Introduction
HF is a significant public health problem. It is a complex chronic illness that affects nearly 6 million Americans and the prevalence is expected to increase as the population ages.1 HF is the leading cause of preventable hospitalizations in people over the age of 65, with a 19–32% readmission rate within 6 months.2–4 Given the high and rising prevalence, high healthcare utilization costs and poor outcomes, it is considered a high priority condition.5
Poor HF outcomes have been attributed to insufficient HF self-care,6–8 which involves engaging in behaviors to maintain physiologic stability (e.g., adhering to medication and frequent weighing) and decision-making in response to symptoms, (e.g., recognizing signs of fluid overload and taking an extra dose of a diuretic).9 HF self-care is complex and requires both knowledge and skills. HF patients, who are typically older and have multiple morbidities, often have difficulty engaging in self-care and may rely on social support from others for assistance. Yet, data on the association between social support and HF self-care is sparse. Social support is a multidimensional concept which indicates a variety of actual or perceived resources, including emotional support, tangible or instrumental support, or informational support, available to an individual through his/her ties with others.10 Despite the multi-dimensionality of the concept, many studies focus on one type of support- often, emotional or instrumental support- without examining differential effects of other types of perceived support on HF self-care behaviors. Alternatively, other studies conflate perceived support with structural support (e.g., marital status), when in fact the two are conceptually distinct and only moderately correlated.10 This field of research would benefit from a more nuanced and theoretically driven examination of the association between social support and HF self-care.
Social support has been shown to positively influence health outcomes for several chronic illnesses.11–14 However, there is limited and inconsistent evidence to demonstrate whether social support exerts its effect on HF-related outcomes by directly affecting HF self-care. Several studies have shown no independent effect of social support on HF self-care,15–17 while others show that social support is associated with worse self-care.18 The mechanisms by which perceived social support influences self-care are debated.19–21 Confidence in one's ability to control symptoms and adhere to treatment regimens is thought to mediate or moderate the relationship with self-care outcomes.21 Self-care confidence has been associated with better HF self-care behavior22 and therefore may be a mediator of the association between perceived social support and HF self-care behaviors.23
HF self-care interventions have shown variable success at improving outcomes24–26 and the optimal design of such interventions remains unknown. Few HF self-care interventions exist which target the social support networks of HF patients.27,28 It is important to determine the extent to which social support influences HF self-care behaviors in order to guide intervention development and clinical delivery of HF care. Therefore, the aims of this study were to: 1) examine the association between perceived social support and HF self-care behaviors; and 2) determine the extent to which observed associations are mediated by self-care confidence, in a community-dwelling sample of HF patients.
Methods
Design and Sample
We recruited patients with a diagnosis of HF from the general internal medicine or cardiology clinics at one university hospital to complete a cross-sectional survey on perceived social support and HF self-care behaviors. Potentially eligible participants were identified as part of a screening process for study recruitment using the Carolina Data Warehouse for Health (CDW-H). The CDW-H is a central repository containing clinical, research, and administrative data from over 3 million patient records of individuals who have received care in the UNC Health Care System. The CDW-H includes all of the information available in the electronic medical record. Patients were potentially eligible if they were: 21–85 years old, had a clinical diagnosis of systolic or diastolic HF based on ICD-9 codes with confirmatory lab work (e.g., transthoracic and/or transesophageal echocardiogram; cardiac catherization) and/or radiographic testing (e.g., stereo, frontal chest x-ray; sestamibi adenonsine, dobutamine or treadmill; MUGA rest only or stress rest), were symptomatic within past 6 months with a New York Heart Association Class II-IV functional class, were currently prescribed a loop diuretic, and were able to speak English. We excluded patients if they: 1) had significant cognitive impairment; 2) resided in a nursing home or assisted living facility; 3) had a terminal illness with life expectancy of less than 1 year, based on their physician's determination; 4) had a medical or psychiatric condition that may hinder participation; 5) had a clinical diagnosis of dementia or Alzheimer's disease based on ICD-9 codes; and 6) were unable to perform activities of daily living (ADLs), based on participant self-report to a structured question.
Recruitment and Assessment
After initial screening using the CDW-H data, we compiled a list of potentially eligible participants and also reviewed daily clinic schedules and medical records for additional potential participants. After verifying the diagnosis of HF and suitability to participate in the study with the patient's health care provider, 3 trained research assistants (RAs), over the course of the study, directly approached potential participants at the time of a regularly scheduled medical visit to determine their interest in participating. For interested individuals, the RA then verified eligibility and obtained informed consent. RAs administered the questionnaire to participants immediately prior to the visit or via telephone if the participant was unable to complete it before the visit.
Measures
Demographic and Clinical Characteristics
We used information from the CDW-H (i.e. administrative/billing database and electronic medical record) and/or participant report to obtain information on age, race (black vs. white), gender, highest education level, annual household income, marital status, self-rated health, New York Heart Association (NYHA) functional class, ejection fraction (EF), depressive symptoms, and cognitive function. NYHA class was assessed with the question, “which one of the following statements best describes how your heart condition affects you today?” with the 4 response options ranging from “no difficulty with usual physical activity” to “inability to do any physical activity without discomfort.” Depressive symptoms were assessed using the Center for Epidemiologic Studies Depression (CES-D) 10-item measure,29 which assesses the frequency of depressive symptomatology over the past week using a 4-point ordinal scale (ranging from rarely or none of the time to most or all of the time). Possible scores on the CES-D 10-item range from 0–30. We used the Blessed test of Orientation-Memory-Concentration to assess cognitive impairment. The 6-item screening measure is quick, easy to administer and score, and discriminates between mild, moderate, and severe cognitive impairment.30 It has demonstrated reliability and validity when compared to the mini-mental status exam.31 A cut-off of 8 was used because it allowed us to screen out individuals who would not be able to provide informed consent while simultaneously not excluding patients with only mild cognitive impairment, since diminished cognitive function is common in HF patients.32–34
Heart Failure Self-Care Behaviors
We used the 22-item Self-Care of Heart Failure Index (SCHFI) version 6.2 to measure the outcome variables (self-care maintenance and self-care management) and the mediator variable (self-care confidence). The 10-item self-care maintenance scale assesses behaviors used to maintain physiologic stability (e.g., adherence to medications, frequent weighing). The 6-item self-care management scale assesses decision-making in response to symptoms (e.g., recognizing signs of fluid overload and taking an extra dose of a diuretic). Of note, the self-care management questions are answered and scored only if the respondent endorses having experienced dyspnea or ankle swelling within the past month. The 6-item self-care confidence scale assesses one's level of confidence in carrying out self-care maintenance and management behaviors. Each scale score is standardized, with scores ranging from 0–100, where higher scores indicate better self-care. Scores ≥ 70 are reflective of “adequate” self-care. The internal reliability for the scales has previously been reported as 0.55 for maintenance, 0.60 for management, and 0.83 for confidence.9 In the present study, coefficient alpha for maintenance was 0.46, 0.65 for management, and 0.78 for confidence. The SCHFI was written at a sixth grade reading level and takes about 5–10 minutes to complete.
Perceived Social Support
We assessed perceived support using the social support survey developed by Sherbourne & Stewart for the Medical Outcomes Study.35 We selected this measure because it was developed for use in patients with chronic illnesses, is easy to administer, has a sound theoretical basis, and assesses multiple dimensions of social support. This 19-item measure forms 4 subscales, with each assessing the perceived availability of a different aspect of support: emotional/informational, affectionate, tangible, and positive social interaction. For the main analyses reported here, we focus on the 8-item emotional/informational subscale. Each item is scored using 5-point response options, from 0 (none of the time) to 4 (all of the time), with standardized scoring ranging from 0–100 where higher scores indicate greater perceived support. The reliability and validity of this instrument has been documented in other patient populations, including patients with HF.35–37 Internal consistency for the overall scale has been reported as 0.91–0.97 and values for the subscales range from an internal consistency reliability of 0.91–0.96.35–37 In the current study, the Cronbach's alpha internal consistency reliability estimates of the total scale were 0.96 and subscale values were 0.82 to 0.94 (tangible=0.84; affectionate=0.82; social interaction= 0.92; emotional/informational=0.94).
Data Analysis
We performed all analyses using SAS 9.2. (SAS Institute Inc., Cary, North Carolina) We calculated means and frequencies to describe the distribution of the data by categories of perceived emotional/informational support. For normally distributed interval data, we used t-tests. For non-normally distributed data, such as educational level, CES-D, and Blessed test score, we used the Mann Whitney U test. Otherwise, we used chi-square tests to compare frequencies. For the main analysis, we conducted multiple regression analysis to determine the independent effect of perceived emotional/informational support on HF self-care maintenance and self-care management after adjusting for the following potential confounders which have been shown or hypothesized to be related to self-care behaviors and social support: age, race, gender, educational level, annual household income, self-rated health, NYHA class, EF, depressive symptoms, and cognitive impairment. In separate regression analyses we also examined associations between each of the other 4 perceived support subscales separately and HF self-care maintenance and self-care management.
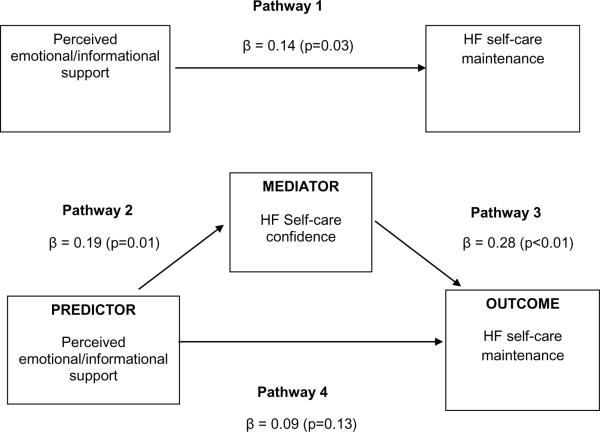
We conducted a mediation analysis using the Baron & Kenny method38 to examine whether self-care confidence mediated the association between perceived social support and HF self-care behaviors (Figure 1). Mediation hypotheses are commonly used in social psychology research and represent the generative mechanism through which the focal independent variable is able to influence the dependent variable of interest.38 In our analysis, self-care confidence was required to meet the following criteria to be considered a mediator: (a) variations in the levels of the predictor variable (perceived social support) significantly accounted for variations in the presumed mediator (self-care confidence); (b) variation in the mediator (self-care confidence) significantly accounted for variations in the dependent variables (HF self-care maintenance or self-care management); and when paths in (a) and (b) are controlled for, a previously significant association between the predictor and dependent variables (c) was no longer significant, with the strongest demonstration of mediation occurring when the path articulated in (c) was zero38 (Figure 1). We used four regression models to estimate the relative effect size needed to satisfy the four mediation criteria. We set statistical significance at p ≤ .05 for all regression models. One approach typically used to assess for mediation is to include the mediator in statistical models with other potential confounders. Therefore, we included all covariates in the mediational models. We determined mediation with statistical significance and changes in the magnitude of unstandardized regression coefficients, β, between Pathways 1 and 4 (Figure 2). We considered a percentage change of ≥15% in β for emotional/informational support when self-care confidence is removed from the model as suggestive of mediation, while a percent change of ≥30% as strongly suggestive of mediation.39
Figure 1.
Baron and Kenny mediational model of the conceptual relationships among perceived emotional/informational support, HF self-care confidence and HF self-care maintenance
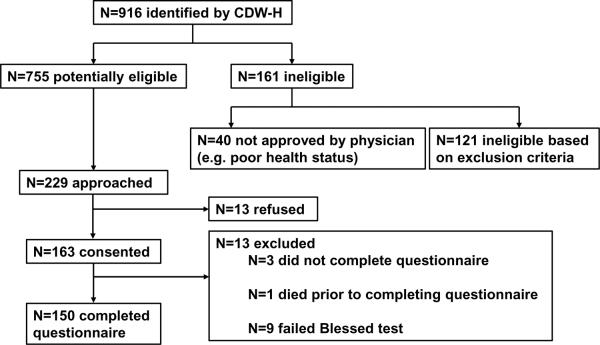
Figure 2.
Mediational model showing the unstandardized multivariate linear regression coefficients (β) for the direct and the mediated pathways by which perceived emotional/informational support influences HF self-care behaviors
Results
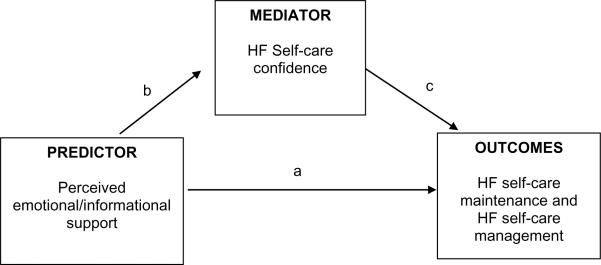
After initial screening of CDW-H data and medical record review, we identified 916 potentially eligible participants (Figure 3). Of the 916, 121 (13.2%) were ineligible based on inclusion/exclusion criteria. An additional 40 (5.3%) participants were not approved by providers. Out of the remaining 755 potential participants, 229 (30.3%) were approached in clinic and 163 (71.1%) agreed to participate. Of the 163 who agreed to participate, 9 (5.5%) failed the Blessed Test; 1 (< 1.0%) died before the questionnaire could be administered and 3 (1.8%) did not complete the questionnaire, leaving 150 (92%) who completed the questionnaire.
Figure 3.
Flow diagram of study recruitment
Demographics
Table 1 lists the overall sample characteristics and characteristics stratified by perceived emotional/informational support. The mean age of patients in our sample was 61 years (range 22–84), 51% were female, 44% were African American, and the mean educational level attained was 13 years (SD 3). Forty-one percent of the sample had an annual household income of less than 15,000 and there were significant differences in annual household income by median social support score. The mean CES-D score was 8.5 and those with below median social support score had significantly higher CES-D scores (i.e. more depressive symptoms).
Table 1.
Characteristics of Study Participants Overall and Stratified by Perceived Emotional/Informational Support dichotomized at the median value of 90.
| Overall Sample (N=148) | Perceived emotional/informational support score below median (N=74) | Perceived emotional/informational support score above median (N=74) | P-value | |
|---|---|---|---|---|
|
| ||||
| Mean Age, yrs (SD) | 61 (12) | 60 (11) | 61 (14) | 0.72 |
|
| ||||
| Female, % | 51 | 53 | 49 | 0.68 |
|
| ||||
| Black, % | 44 | 49 | 39 | 0.22 |
|
| ||||
| Mean highest educational level (SD) | 13 (2.6) | 13 (2.3) | 13 (2.8) | 0.65 |
|
| ||||
| Annual household Income, % | ||||
| <$15,000 | 42 | 53 | 29 | 0.02 |
| $15,000–$24,999 | 22 | 21 | 22 | |
| $25,000–$40,000 | 19 | 14 | 23 | |
| >$40,000 | 19 | 11 | 26 | |
|
| ||||
| Currently Married (vs. Other)*, % | 39 | 34 | 44 | 0.20 |
|
| ||||
| Self-Rated Health, % | ||||
| Excellent/Very good/Good | 37.8 | 28 | 46 | 0.08 |
| Fair | 45 | 52 | 38 | |
| Poor | 17 | 19 | 15 | |
|
| ||||
| Mean CESD score (SD) | 9 (6.4) | 9.9 (6.8) | 7.2 (5.8) | 0.01 |
|
| ||||
| Mean Blessed test score (SD) | 3.3 (2.7) | 3.5 (2.6) | 3.0 (2.8) | 0.17 |
|
| ||||
| Left Ventricular Ejection Fraction | ||||
| ≥55% | 39 | 38 | 41 | 0.92 |
| 40–55% | 24 | 24 | 24 | |
| <40% | 37 | 38 | 35 | |
|
| ||||
| New York Heart Association, % | ||||
| 17 | 14 | 20 | 0.33 | |
| Class I | 54 | 58 | 50 | |
| Class II | 20 | 17 | 24 | |
| Class III | 8 | 11 | 5 | |
| Class IV | ||||
Other refers to divorced/separated, widowed, single or unknown
Perceived social support and HF Self-Care Behaviors
Overall, the mean perceived emotional/informational support score was 83 (SD 19.8, with possible scores ranging from 0–100 where higher scores indicate greater support). Mean scores for self-care maintenance (N=149) were 70 (SD 14; possible scores ranging from 0–100, with higher scores indicating better self-care maintenance), with 52% of the sample having “adequate” self-care maintenance (score ≥ 70). Mean score for self-care management was 57 (SD 24; possible scores ranging from 0–100, with higher scores indicating better self-care management), with 32% of sample with recent symptoms having “adequate” self-care management. The mean score for self-care confidence was 65 (SD 17; possible scores ranging from 0–100, with higher scores indicating better self-care confidence), with 33% of people having “adequate” self-care confidence. Educational level (β = 1.0; p=0.02) and cognitive impairment score (β = −1.1; p<0.01) were significantly associated with self-care maintenance, while age was significantly associated with self-care management (β = −0.66; p<0.01). In unadjusted analysis, perceived emotional/informational support was significantly associated with self-care maintenance (N=148; β =0.17, SE 0.06; p<0.01). After adjusting for age, race, gender, highest educational level, annual income, marital status, self-rated health, NYHA class, EF, depressive symptomatology score, and cognitive impairment score, the association between perceived emotional/informational support and self-care maintenance remained significant (N=122; β =0.14, SE 0.06; p=0.03). Perceived emotional/informational support was significantly associated with self-care management in unadjusted analysis (N=112; β =0.23, SE=0.11; p=0.04), but not in adjusted analysis (N=94; β =0.20, SE=0.12; p=0.10). Of note, none of the other perceived social support scales were statistically significantly associated with HF self-care maintenance or management (data not shown).
Self-care Confidence as a Mediator of Relationship Between Perceived Social Support and Heart Failure Self-care Behaviors
Lastly, we examined whether the multivariate linear association between perceived emotional/informational support and HF self-care maintenance and HF self-care management was mediated through self-care confidence (Figure 2). The β for the adjusted association between perceived emotional/informational support and HF self-care maintenance without the proposed mediator (Pathway 1) was 0.14 (p=0.03). After including the potential mediator, self-care confidence (Pathway 4), the β was 0.09 (p=0.13). Therefore, the percent change in β for perceived emotional/informational support after adjusting for self-care confidence was 32%, which is strongly suggestive of mediation. The β for the adjusted association between perceived emotional/informational support and HF self-care management without the proposed mediator (Pathway 1) was 0.20 (p=0.11). After including the potential mediator- self-care confidence (Pathway 4)- the β was 0.16 (p=0.21). The percent change in β for perceived emotional/informational support after adjusting for self-care confidence was 20%, which is suggestive of mediation.
Discussion
In this cross-sectional single-site study of 150 community dwelling patients with HF, we sought to first examine whether perceived emotional/informational support was associated with HF self-care behaviors (self-care maintenance and management) and then to determine whether any observed associations were mediated through self-care confidence. We found that higher perceived emotional/informational support was positively and significantly associated with better HF self-care maintenance, but not self-care management, in adjusted models. The association between perceived emotional/informational support and HF self-care maintenance appears to be mediated through self-care confidence.
We found that perceived emotional/informational support, but not the other types of perceived support (i.e., affectionate support, tangible support, and positive social interaction) is positively associated with HF self-care maintenance, but not self-care management, in adjusted models. This finding confirms those of other studies,23,40 including a multisite study by Gallagher and colleagues,40 which was conducted in hospitalized HF patients who were generally more symptomatic (92% were NYHA Class III or IV) than our study participants. In a sample with similar NYHA class distribution and socio-demographic characteristics to ours, Salyer et al.23 also examined the association between supportive relationships (using the MOS social support scale) and HF self-care behaviors (using the SCHFI) and tested whether self-care confidence mediated that association. Consistent with our finding that self-care confidence mediates the association between perceived social support and self-care behaviors, they found positive direct and indirect (through self-care confidence) effects of perceived social support on self-care maintenance. They also found a positive indirect effect through self-care confidence, but not a direct effect, on self-care management. Because we simultaneously measured perceived emotional/informational support and self-care confidence, we cannot be certain of the directionality of this association. It is possible that individuals who are more self-confident in their HF abilities perceive more emotional/informational support. Therefore, future studies should examine this question using a longitudinal study design. Despite this limitation, this suggests that efforts to improve HF patients' confidence may influence engagement in self-care maintenance and management behaviors.
Other researchers, on the contrary, have found no significant association between perceived support and HF self-care behaviors.16,18,41 This is likely due to differences in study populations and in conceptualization and measurement of key variables. Rockwell et al.'s study sample consisted of hospitalized HF patients, whereas we sampled community-dwelling HF patients. Social support likely differs between hospitalized and community-dwelling patients with HF, making comparisons between these studies problematic. Rockwell et al. used a single subscale from a different measure of HF self-care which assessed whether patients could recognize the importance of various signs and symptoms of HF, regardless to whether they had actually experienced the signs or symptoms.18 Conceptually, this measure is different from the SCHFI self-care maintenance and management subscales which reflect engagement in self-care behaviors and decision-making. Further, Rockwell et al. used an aggregate measure of social support which combined a structural support item (i.e. marital status- yes/no) with questions assessing both perceived and received support- for which the latter is confounded with need. Inclusion of marital status in the conceptualization of support likely biased these results towards a null finding since previous studies have shown that structural and perceived aspects of support are not highly correlated and crude indicators of marital status do not provide insight into the quality of the marital relationship- which is most influential on HF outcomes, particularly survival.42,43 The lack of precision regarding the assessment of social support and use of a potentially inadequate measure for capturing the multifactorial nature of self-care in the latter study may have resulted in the unexpected negative association between social support and HF self-care. Taken together, these findings suggest that social support may not be as important for amassing knowledge of HF signs and symptoms, but it is important for engaging in self-care behaviors and decision-making in response to symptoms.
Sayers et al.,41 examined cross-sectional associations between perceived emotional or instrumental support from family, friends, or significant others (measured using the Multidimensional Scale of Perceived Social Support) and HF self-care maintenance, self-care management and self-care confidence (also measured with the SCHFI) among 74 participants (97% men) primarily recruited from the Veteran's Administration Medical Center. While they demonstrated a statistically significant association between perceived support and self-care confidence, there was no association with HF self-care maintenance or self-care management. There are several possible reasons why our study yielded different results from this one. First, patterns of self-care and perceptions of social support likely differ between men and women.16 Second, there may be key demographic differences in our study populations (e.g. NYHA class) which may influence HF self-care behaviors. The authors do not provide data on the NYHA classification of their sample. Third, their sample size was smaller than ours, limiting their statistical power to detect significant associations.
Our multivariate analysis shows that perceived emotional/informational support is not statistically significantly associated with HF self-care management, even though the effect size for this outcome is greater than the effect size between perceived emotional/informational support and self-care maintenance. Our smaller sample size of 112 participants with symptoms contributed to less power to demonstrate a statistically significant association between perceived emotional/informational support and self-care management. Because of the large effect size, future studies with larger sample sizes may better elucidate a relationship between perceived social support and self-care management.
To date, it is not clear what type of support is most influential on HF self-care behaviors, especially self-care management. We examined other types of perceived support (tangible, affection, and positive social interaction) and none were significantly associated with self-care management or maintenance. Future studies should examine whether actual received, as opposed to perceived support, matters most for engaging in self-care and decision-making related to HF self-care. Although received support is confounded with need, it may be theoretically more relevant than perceived support when examining factors associated with self-care management, which is only assessed in symptomatic individuals. It would also be important for future studies to use measures of social support which identify who provides the support (and characteristics of those persons) as well as other structural features of the patient's social network to provide a more in depth and nuanced understanding of how social network structure impacts the perception and receipt of social support, which then influences HF self-care behaviors.
Our study has limitations. First, as a cross-sectional study, we were unable to imply causality. Second, our sample of only 150 participants consisted of HF patients from one large academic medical center, therefore generalizability may be limited. Finally, we do not examine associations between perceived social support, self-care behaviors, and more distal HF-related outcomes (e.g., hospitalization or mortality).
Despite these limitations, our study has strengths. It was guided by a clear theoretical conceptualization of HF self-care as a naturalistic decision-making process21 potentially influenced by social support, and we examined associations between several types of perceived support and self-care behaviors. We had a larger sample size than other studies which examined a similar research question23,41 and a larger percentage of blacks and females, which may increase the external validity of our results. Our study was conducted in an outpatient sample, as opposed to hospitalized HF patients. This is important since perceptions of support likely differ between hospitalized and community-dwelling patients with HF and the majority of HF self-care for occurs in the outpatient setting.
Our study has important implications for clinical practice and research. There is convincing evidence that social support influences health for a variety of illnesses.10 Our findings extend our understanding of the association between perceived social support and self-care behaviors and suggest that targeting social support may be a good approach for improving self-care and facilitating the delivery of more patient/family centered care. Given the association between lower levels of social support and worse HF self-care behaviors, clinicians should assess whether and what types of support HF patients perceive and receive from members of their social networks, particularly in patients found to have inadequate self-care. This approach would uncover patients who might benefit from social support interventions. In addition, our findings have implications for how health care providers can support self-care, which is a key component of the Chronic Care Model44 of health care delivery. HF self-care education should target not only the patient with HF, but their supporters as well. Family members often accompany patients into the exam room at medical visits45–47 and therefore providers have a unique opportunity to provide HF self-care education to patient and family supporter simultaneously. Based on these findings, we are currently designing a self-care education and activation intervention for HF patients and their family members who accompany them to medical visits with the goal of improving HF self-care behaviors.
Conclusion
Our work and that of others has shown that perceived social support is influential for engagement in and decision-making related to HF self-management behaviors and that self-care confidence is an important potential mediator of this association. Although one's perception of the availability of various types of support is important, future studies should also seek to understand the dynamics of how perceived support gets translated into situations where support is actually received. This would provide a more nuanced understanding of how support influences engagement in and decision-making related to HF self-care behaviors.
Acknowledgements
We would like to thank the providers and staff in the General Internal Medicine and Cardiology clinics who allowed us to recruit their patients, as well as the patients who willingly agreed to participate in this study.
Grant Support This work was supported by award number KL2RR025746 from the National Center for Research Resources, a component of the National Institutes of Health (NIH) via the Clinical Translational Science Award (CTSA)-K12 Scholars Program and NIH Roadmap for Medical Research, as well as by award number K23HL107614 from the National Heart, Lung, and Blood Institute to Dr. Crystal Cené. The CTSA is a national consortium with the goal of transforming how clinical and translational research is conducted, ultimately enabling researchers to provide new treatments more efficiently and quickly to patients. Salary support to conduct this research was also provided through a Mid-career Investigator Award in Patient-Oriented Research (K24 HL105493) as well as award number UL1RR025747 from the National Center for Research Resources to Dr. Giselle Corbie-Smith. Dr. Pignone's effort was supported by an established investigator award from the National Cancer Institute (5K05CA129166). Dr. Christine Jones is supported by a NIH/HRSA training grant and is a NRSA Primary Care Research Fellow (T32HP14001).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosures Authors have no conflicts of interest to disclose.
References
- 1.Lloyd-Jones D, Adams R, Carnethon M, De Simone G, Ferguson TB, Flegal K, et al. Heart disease and stroke statistics--2009 update: A report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation. 2009 Jan 27;119(3):480–486. doi: 10.1161/CIRCULATIONAHA.108.191259. [DOI] [PubMed] [Google Scholar]
- 2.Ross JS, Chen J, Lin Z, Bueno H, Curtis JP, Keenan PS, et al. Recent national trends in readmission rates after heart failure hospitalization. Circ Heart Fail. 2010 Jan;3(1):97–103. doi: 10.1161/CIRCHEARTFAILURE.109.885210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Joynt KE, Jha AK. Who has higher readmission rates for heart failure, and why? Implications for efforts to improve care using financial incentives. Circ Cardiovasc Qual Outcomes. 2011 Jan 1;4(1):53–59. doi: 10.1161/CIRCOUTCOMES.110.950964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Epstein AM, Jha AK, Orav EJ. The relationship between hospital admission rates and rehospitalizations. N Engl J Med. 2011 Dec 15;365(24):2287–2295. doi: 10.1056/NEJMsa1101942. [DOI] [PubMed] [Google Scholar]
- 5.Centers for Medicare & Medicaid Services [Accessed 07/26/2012];Hospital quality initiative. 2012 Available at: http://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/HospitalQualityInits/index.html.
- 6.Lainščak M, Cleland JGF, Lenzen MJ, Keber I, Goode K, Follath F, et al. Nonpharmacologic Measures and Drug Compliance in Patients with Heart Failure: Data from the EuroHeart Failure Survey. Am J Cardiol. 2007;99(6, Supplement 2):S31–S37. doi: 10.1016/j.amjcard.2006.12.018. [DOI] [PubMed] [Google Scholar]
- 7.Hauptman PJ. Medication adherence in heart failure. Heart Fail Rev. 2008 Feb;13(1):99–106. doi: 10.1007/s10741-007-9020-7. [DOI] [PubMed] [Google Scholar]
- 8.Michalsen A, Konig G, Thimme W. Preventable causative factors leading to hospital admission with decompensated heart failure. Heart. 1998 Nov;80(5):437–441. doi: 10.1136/hrt.80.5.437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Riegel B, Lee CS, Dickson VV, Carlson B. An update on the self-care of heart failure index. J Cardiovasc Nurs. 2009 Nov-Dec;24(6):485–497. doi: 10.1097/JCN.0b013e3181b4baa0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cohen S, Underwood LG, Gottlieb BH, editors. Social support measurement and intervention: A guide for health and social scientists. Oxford University Press; New York, New York: 2000. [Google Scholar]
- 11.Luttik ML, Jaarsma T, Moser D, Sanderman R, van Veldhuisen DJ. The importance and impact of social support on outcomes in patients with heart failure: an overview of the literature. J Cardiovasc Nurs. 2005 May-Jun;20(3):162–169. doi: 10.1097/00005082-200505000-00007. [DOI] [PubMed] [Google Scholar]
- 12.Moser DK, Worster PL. Effect of psychosocial factors on physiologic outcomes in patients with heart failure. J Cardiovasc Nurs. 2000 Jul;14(4):106–115. doi: 10.1097/00005082-200007000-00008. [DOI] [PubMed] [Google Scholar]
- 13.Murberg TA. Long-term effect of social relationships on mortality in patients with congestive heart failure. Int J Psychiatry Med. 2004;34(3):207–217. doi: 10.2190/GKJ2-P8BD-V59X-MJNQ. [DOI] [PubMed] [Google Scholar]
- 14.MacMahon KM, Lip GY. Psychological factors in heart failure: a review of the literature. Arch Intern Med. 2002 Mar 11;162(5):509–516. doi: 10.1001/archinte.162.5.509. [DOI] [PubMed] [Google Scholar]
- 15.Cameron J, Worrall-Carter L, Riegel B, Lo SK, Stewart S. Testing a model of patient characteristics, psychologic status, and cognitive function as predictors of self-care in persons with chronic heart failure. Heart Lung. 2009 Sep-Oct;38(5):410–418. doi: 10.1016/j.hrtlng.2008.11.004. [DOI] [PubMed] [Google Scholar]
- 16.Heo S, Moser DK, Lennie TA, Riegel B, Chung ML. Gender differences in and factors related to self-care behaviors: a cross-sectional, correlational study of patients with heart failure. Int J Nurs Stud. 2008 Dec;45(12):1807–1815. doi: 10.1016/j.ijnurstu.2008.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kato N, Kinugawa K, Ito N, Yao A, Watanabe M, Imai Y, et al. Adherence to self-care behavior and factors related to this behavior among patients with heart failure in Japan. Heart Lung. 2009 Sep-Oct;38(5):398–409. doi: 10.1016/j.hrtlng.2008.11.002. [DOI] [PubMed] [Google Scholar]
- 18.Rockwell JM, Riegel B. Predictors of self-care in persons with heart failure. Heart Lung. 2001 Jan-Feb;30(1):18–25. doi: 10.1067/mhl.2001.112503. [DOI] [PubMed] [Google Scholar]
- 19.Molloy GJ, Johnston DW, Witham MD. Family caregiving and congestive heart failure. Review and analysis. Eur J Heart Fail. 2005 Jun;7(4):592–603. doi: 10.1016/j.ejheart.2004.07.008. [DOI] [PubMed] [Google Scholar]
- 20.Sebern M, Riegel B. Contributions of supportive relationships to heart failure self-care. Eur J Cardiovasc Nurs. 2009 Jun;8(2):97–104. doi: 10.1016/j.ejcnurse.2008.07.004. [DOI] [PubMed] [Google Scholar]
- 21.Riegel B, Dickson VV. A situation-specific theory of heart failure self-care. J Cardiovasc Nurs. 2008 May-Jun;23(3):190–196. doi: 10.1097/01.JCN.0000305091.35259.85. [DOI] [PubMed] [Google Scholar]
- 22.Schnell-Hoehn KN, Naimark BJ, Tate RB. Determinants of self-care behaviors in community-dwelling patients with heart failure. J Cardiovasc Nurs. 2009 Jan-Feb;24(1):40–47. doi: 10.1097/01.JCN.0000317470.58048.7b. [DOI] [PubMed] [Google Scholar]
- 23.Salyer J, Schubert CM, Chiaranai C. Supportive Relationships, Self-care Confidence, and Heart Failure Self-care. J Cardiovasc Nurs. 2011 Nov 1; doi: 10.1097/JCN.0b013e31823228cd. [DOI] [PubMed] [Google Scholar]
- 24.Jovicic A, Holroyd-Leduc JM, Straus SE. Effects of self-management intervention on health outcomes of patients with heart failure: a systematic review of randomized controlled trials. BMC Cardiovasc Disord. 2006 Nov 2;6:43. doi: 10.1186/1471-2261-6-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.McAlister FA, Stewart S, Ferrua S, McMurray JJJV. Multidisciplinary strategies for the management of heart failure patients at high risk for admission: A systematic review of randomized trials. J Am Coll Cardiol. 2004 Aug 18;44(4):810–819. doi: 10.1016/j.jacc.2004.05.055. [DOI] [PubMed] [Google Scholar]
- 26.DeWalt DA, Schillinger D, Ruo B, Bibbins-Domingo K, Baker DW, Holmes GM, et al. A multisite randomized trial of a single- versus multi-session literacy sensitive self-care intervention for patients with heart failure. Circulation. 2012;125:2854–62. doi: 10.1161/CIRCULATIONAHA.111.081745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Dunbar SB, Clark PC, Deaton C, Smith AL, De AK, O'Brien MC. Family education and support interventions in heart failure: a pilot study. Nurs Res. 2005 May-Jun;54(3):158–166. doi: 10.1097/00006199-200505000-00003. [DOI] [PubMed] [Google Scholar]
- 28.Piette JD, Gregor MA, Share D, Heisler M, Bernstein SJ, Koelling T, et al. Improving heart failure self-management support by actively engaging out-of-home caregivers: results of a feasibility study. Congest Heart Fail. 2008 Jan-Feb;14(1):12–18. doi: 10.1111/j.1751-7133.2008.07474.x. [DOI] [PubMed] [Google Scholar]
- 29.Andresen EM, Malmgren JA, Carter WB, Patrick DL. Screening for depression in well older adults: evaluation of a short form of the CES-D (Center for Epidemiologic Studies Depression Scale) Am J Prev Med. 1994 Mar-Apr;10(2):77–84. [PubMed] [Google Scholar]
- 30.Katzman R, Brown T, Fuld P, Peck A, Schechter R, Schimmel H. Validation of a short Orientation-Memory-Concentration Test of cognitive impairment. Am J Psychiatry. 1983 Jun;140(6):734–739. doi: 10.1176/ajp.140.6.734. [DOI] [PubMed] [Google Scholar]
- 31.Goring H, Baldwin R, Marriott A, Pratt H, Roberts C. Validation of short screening tests for depression and cognitive impairment in older medically ill inpatients. Int J Geriatr Psychiatry. 2004 May;19(5):465–471. doi: 10.1002/gps.1115. [DOI] [PubMed] [Google Scholar]
- 32.Bennett SJ, Sauve MJ. Cognitive deficits in patients with heart failure: a review of the literature. J Cardiovasc Nurs. 2003 Jul-Aug;18(3):219–242. doi: 10.1097/00005082-200307000-00007. [DOI] [PubMed] [Google Scholar]
- 33.Pressler SJ. Cognitive functioning and chronic heart failure: a review of the literature (2002-July 2007) J Cardiovasc Nurs. 2008 May-Jun;23(3):239–249. doi: 10.1097/01.JCN.0000305096.09710.ec. [DOI] [PubMed] [Google Scholar]
- 34.Vogels RL, Oosterman JM, van Harten B, Scheltens P, van der Flier WM, Schroeder-Tanka JM, et al. Profile of cognitive impairment in chronic heart failure. J Am Geriatr Soc. 2007 Nov;55(11):1764–1770. doi: 10.1111/j.1532-5415.2007.01395.x. [DOI] [PubMed] [Google Scholar]
- 35.Sherbourne CD, Stewart AL. The MOS social support survey. Soc Sci Med. 1991;32(6):705–714. doi: 10.1016/0277-9536(91)90150-b. [DOI] [PubMed] [Google Scholar]
- 36.Bennett SJ, Baker SL, Huster GA. Quality of life in women with heart failure. Health Care Women Int. 1998 May-Jun;19(3):217–229. doi: 10.1080/073993398246386. [DOI] [PubMed] [Google Scholar]
- 37.Bennett SJ, Pressler ML, Hays L, Firestine LA, Huster GA. Psychosocial variables and hospitalization in persons with chronic heart failure. Prog Cardiovasc Nurs. 1997 Fall;12(4):4–11. [PubMed] [Google Scholar]
- 38.Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986 Dec;51(6):1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- 39.Eriksson H, Caidahl K, Larsson B, Ohlson LO, Welin L, Wilhelmsen L, et al. Cardiac and pulmonary causes of dyspnoea--validation of a scoring test for clinical-epidemiological use: the Study of Men Born in 1913. Eur Heart J. 1987 Sep;8(9):1007–1014. doi: 10.1093/oxfordjournals.eurheartj.a062365. [DOI] [PubMed] [Google Scholar]
- 40.Gallagher R, Luttik ML, Jaarsma T. Social support and self-care in heart failure. J Cardiovasc Nurs. 2011 Nov-Dec;26(6):439–445. doi: 10.1097/JCN.0b013e31820984e1. [DOI] [PubMed] [Google Scholar]
- 41.Sayers SL, Riegel B, Pawlowski S, Coyne JC, Samaha FF. Social support and self-care of patients with heart failure. Ann Behav Med. 2008 Feb;35(1):70–79. doi: 10.1007/s12160-007-9003-x. [DOI] [PubMed] [Google Scholar]
- 42.Rohrbaugh MJ, Shoham V, Coyne JC. Effect of Marital Quality on Eight-Year Survival of Patients With Heart Failure. Am J Cardiol. 2006;98(8):1069–1072. doi: 10.1016/j.amjcard.2006.05.034. [DOI] [PubMed] [Google Scholar]
- 43.Coyne JC, Rohrbaugh MJ, Shoham V, Sonnega JS, Nicklas JM, Cranford JA. Prognostic importance of marital quality for survival of congestive heart failure. Am J Cardiol. 2001;88(5):526–529. doi: 10.1016/s0002-9149(01)01731-3. [DOI] [PubMed] [Google Scholar]
- 44.Glasgow RE, Funnell MM, Bonomi AE, Davis C, Beckham V, Wagner EH. Self-management aspects of the improving chronic illness care breakthrough series: implementation with diabetes and heart failure teams. Ann Behav Med. 2002 Spring;24(2):80–87. doi: 10.1207/S15324796ABM2402_04. [DOI] [PubMed] [Google Scholar]
- 45.Wolff JL, Roter DL. Hidden in plain sight: medical visit companions as a resource for vulnerable older adults. Arch Intern Med. 2008 Jul 14;168(13):1409–1415. doi: 10.1001/archinte.168.13.1409. [DOI] [PubMed] [Google Scholar]
- 46.Sayers SL, White T, Zubritsky C, Oslin DW. Family involvement in the care of healthy medical outpatients. Fam Pract. 2006 Jun;23(3):317–324. doi: 10.1093/fampra/cmi114. [DOI] [PubMed] [Google Scholar]
- 47.Botelho RJ, Lue BH, Fiscella K. Family involvement in routine health care: a survey of patients' behaviors and preferences. J Fam Pract. 1996 Jun;42(6):572–576. [PubMed] [Google Scholar]