Summary
Traumatic pericallosal artery aneurysms are rare complications of blunt head trauma. The pericallosal artery is torn under the sharp edge of the rigid falx. CT shows a typical hematoma in the corpus callosum. Endovascular treatment with occlusion of the aneurysm including the parent vessel with coils or glue is the best treatment option.
Key words: trauma, aneurysm, endovascular treatment, parent vessel occlusion
Introduction
Traumatic intracranial aneurysms are rare complications of closed and penetrating head injuries 1,2. With blunt head trauma, the most common location of a traumatic aneurysm is the internal carotid artery by laceration of the vessel following fracture of the skull base. The pericallosal artery is another common location with laceration of a distal pericallosal artery branch under the sharp edge of the falx cerebri. Traumatic intracranial aneurysms are fragile, prone to rupture, and represent a challenging subset of vascular lesions for either surgery or endovascular therapy. This report presents two patients with blunt head trauma and traumatic pericallosal artery aneurysms treated by endovascular parent vessel occlusion.
Case 1
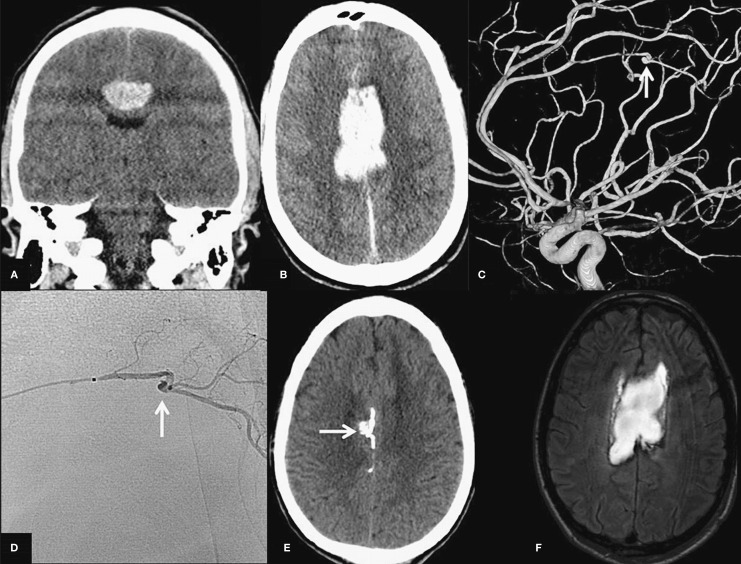
A 28-year-old man hit a deer while driving his car. He was found unresponsive 25 meters away from the damaged car. On admission, next to frontal contusions and subarachnoid blood a brain CT scan showed a large haematoma in the corpus callosum (Figure 1A,B) suspect for a traumatic pericallosal artery aneurysm. In addition, there was a severe lung contusion with rib fractures. After six days his respiratory condition was stabilized and cerebral angiography including 3D rotational angiography was performed. This angiogram showed a tiny (2 mm) aneurysm on a distal right pericallosal artery branch with circumferential involvement of the vessel (Figure 1C). Endovascular parent vessel occlusion or trapping were considered the only possible therapies in this patient in poor clinical condition. A microcatheter (Marathon, ev3, Irvine, CA, USA) was navigated just proximal to the aneurysm (Figure 1D) and a small amount of n-butylcyanoacrylate glue (Histoacryl, Braun, Melsungen, Germany) was injected. The glue first occluded the parent artery distal to the aneurysm and subsequent reflux occluded the aneurysm itself and the proximal parent vessel. A control angiogram confirmed the exclusion of the aneurysm from the circulation. Follow-up CT scan demonstrated the location of the glue inside the aneurysm as well as in the distal and proximal parent vessel (Figure 1E). MRI performed after four weeks showed diffuse axonal injury, there was no infarction in the distal territory of the occluded pericallosal artery (Figure 1F). The patient gradually recovered and was discharged to a rehabilitation centre.
Figure 1.
Coronal (A) and transverse (B) CT scan with hematoma in the corpus callosum. C) Lateral view of right internal carotid 3D angiogram demonstrates a tiny pericallosal artery aneurysm (arrow). D) Lateral view of superselective angiogram shows the microcatheter positioned just proximal to the aneurysm. From this point glue was injected. The arrow points to the aneurysm. E) Native CT scan demonstrates radio-opaque glue in the aneurysm (arrow) and in proximal and distal parent vessels. F) T2-weighted MR after embolization shows hematoma with no infarction in distal anterior cerebral artery territory.
Case 2
A 22-year-old-man driving his scooter was hit by a car and was found unconscious. CT scan on admission showed diffuse brain swelling and bitemporal hemorrhagic contusions with a right frontal skull fracture. Next to the head injuries, there were fractures of the right humerus and femur. Over the following days he gradually regained consciousness and his extremity fractures were treated with osteosynthesis. On the 17th day of admission, he was suddenly found drowsy in bed. CT scan now showed a large hematoma in the corpus callosum with ventricular extension (Figure 2 A,B). Angiography revealed a false aneurysm of a distal right pericallosal artery branch (Figure 2C,D). A microcatheter (Excelsior SL-10, Boston Scientific, Freemont, CA, USA) was navigated just proximal of the aneurysm (Figure 2E) and the afferent artery was occluded with two C-shaped microcoils. Control angiography confirmed exclusion of the aneurysm from the circulation (Figure 2F). Follow-up CT scan after three weeks showed resolution of the hematoma without infarction in the anterior cerebral artery territory. The patient slowly recovered and was discharged to a rehabilitation centre.
Figure 2.
A,B) CT scan 17 days after trauma with frontal skull fracture demonstrates a new hematoma in the corpus callosum with ventricular extension. C,D) Right internal carotid angiogram in lateral (A) and right oblique (B) projections reveals a traumatic aneurysm of a pericallosal artery branch (arrow). F) Superselective angiogram in the same projection as D of the branch harboring the traumatic aneurysm. E) Angiogram after occlusion of the parent artery with 2 microcoils confirms exclusion of the traumatic aneurysm from the circulation.
Discussion
Traumatic pericallosal artery aneurysms are rare complications of blunt head trauma. The mechanism of injury is related to the close anatomical relationship of the vessel with the falx cerebri. With trauma, the artery may suddenly be moved and injured under the sharp edge of the rigid falx 3,4. The vessel wall may be disrupted to a varying extent. Complete disruption usually leads to immediate hemorrhage with formation of a hematoma and development of a false aneurysm (such as in patient 1) while disruption confined to the internal elastic layer and media with intact adventitia leads to the formation of a dissecting aneurysm 1. Such a dissecting aneurysm is prone to rupture and may be responsible for a delayed hemorrhage (such as in patient 2). Time to delayed rupture varies widely with a mean of 21 days and most within a month following trauma 1. Delayed rupture of a traumatic pericallosal aneurysm is associated with a mortality as high as 50%. Diagnosis of traumatic aneurysms before rupture is unlikely since diagnosis involves catheter angiography or CT angiography and these imaging modalities are not routinely performed after severe blunt head trauma. The primary presence of a hematoma in the corpus callosum or the presence of such hematoma after sudden neurological deterioration days or weeks after trauma should raise the suspicion of a traumatic pericallosal aneurysm. To prevent recurrent hemorrhage, treatment should follow. Nowadays, endovascular treatment is preferred over surgery. With modern microcatheter and wire systems, catheterization of distal branches of intracranial vessels is feasible 3-5. In such distal branches, we prefer parent vessel occlusion to selective coiling of the aneurysm. Parent vessel occlusion with glue or coils is simple to perform and definitely excludes the traumatic aneurysm from the circulation. Distal infarction in the territory of the occluded branch usually does not occur because of sufficient leptomeningeal collateral supply. When infarction still occurs, the infarcted brain area is limited and might be damaged previously by the hematoma. In either case, clinical implications probably are minor in the setting of severe head trauma and aneurysmal hemorrhage. For some patients harboring traumatic pericallosal aneurysms with favorable anatomical characteristics, selective coil occlusion sparing the parent artery is technically possible. However, dissecting aneurysms may continue to grow after selective occlusion with coils resulting in reopening and risk of recurrent hemorrhage 5,6. Therefore, endovascular parent vessel occlusion is the preferred definitive therapy, despite the small risk of adding morbidity by distal infarction.
In conclusion, an immediate or delayed corpus callosum hematoma in the setting of blunt head trauma is suspect for a traumatic pericallosal artery aneurysm. Diagnosis is established with angiography. Endovascular parent vessel occlusion definitely excludes the aneurysm from the circulation.
References
- 1.Larson PS, Reisner A, Morassutti DJ, et al. Traumatic intracranial aneurysms. Neurosurg Focus. 2000;8:e4. doi: 10.3171/foc.2000.8.1.1829. [DOI] [PubMed] [Google Scholar]
- 2.Dubey A, Sung WS, Chen YY, et al. Traumatic intracranial aneurysm: a brief review. J Clin Neurosci. 2008;15:609–612. doi: 10.1016/j.jocn.2007.11.006. [DOI] [PubMed] [Google Scholar]
- 3.Cohen JE, Gomori JM, Segal R, et al. Results of endovascular treatment of traumatic intracranial aneurysms. Neurosurgery. 2008;63:476–485. doi: 10.1227/01.NEU.0000324995.57376.79. [DOI] [PubMed] [Google Scholar]
- 4.Cohen JE, Rajz G, Itshayek E, et al. Endovascular management of traumatic and iatrogenic aneurysms of the pericallosal artery. Report of two cases. J Neurosurg. 2005;102:555–557. doi: 10.3171/jns.2005.102.3.0555. [DOI] [PubMed] [Google Scholar]
- 5.Yuen CM, Kuo YL, Ho JT, et al. Rapid regrowth of a successfully coiled traumatic pericallosal aneurysm. J Clin Neurosci. 2007;14:1215–1219. doi: 10.1016/j.jocn.2006.04.013. [DOI] [PubMed] [Google Scholar]
- 6.Ngo DQ, van Rooij WJ, Tijssen CC. Rapidly growing traumatic cerebral aneurysm with early subarachnoid hemorrhage. Neurology. 2008;70:490. doi: 10.1212/01.wnl.0000299089.07740.a8. [DOI] [PubMed] [Google Scholar]