Abstract
We designed and implemented an electronic patient tracking system with improved user authentication and patient selection. We then measured access to clinical information from previous clinical encounters before and after implementation of the system. Clinicians accessed longitudinal information for 16% of patient encounters before, and 40% of patient encounters after the intervention, indicating such a system can improve clinician access to information. We also attempted to evaluate the impact of providing this access on inpatient admissions from the emergency department, by comparing the odds of inpatient admission from an emergency department before and after the improved access was made available. Patients were 24% less likely to be admitted after the implementation of improved access. However, there were many potential confounders, based on the inherent pre-post design of the evaluation. Our experience has strong implications for current health information exchange initiatives.
Keywords: Health information exchange, reduced admissions, electronic health records
1. Background
Efforts are and have been underway at both the national and local levels to share clinical information between clinical settings [1, 2]. Emergency departments (EDs) are a primary setting for many information access and information sharing initiatives [3–7]. Understanding the longitudinal patient health condition (e.g., problems, allergies, medications, diagnoses, recent procedures, recent laboratory tests) is critical in the ED to forming an appropriate plan of care [8, 9]. Since many emergency department visits are unplanned, urgent, and acute, this information is not communicated in advance to emergency physicians, or when the patient presents to the ED. Stiell et al. studied the resultant information deficit, and found information gaps for emergency physicians occurring in a third of patient visits, of which half are considered essential to patient care [10]. The end result is decreased patient care quality [10], as well as inefficiencies in care, in the form of redundant testing [4], care delays [10], and potentially avoidable inpatient admissions [11–13]. The cost savings associated with decreasing avoidable admissions are among the primary contributors to the potential savings from health information access systems [6].
A critical factor in the success of health information systems that share information across patient settings is understanding how longitudinal patient information is accessed by clinicians, and how to improve access. If clinician workflow issues are not understood and addressed, the chances of success are greatly reduced [14, 15].
2. Objectives
In this article, we evaluate access to longitudinal patient information after providing improved access within an electronic health record (EHR) in use at Intermountain Healthcare. We also performed an evaluation the potential impact of providing this access on inpatient admissions from the emergency department. This evaluation attempted to demonstrate the direct impact of this improved access on clinician actions and health care costs.
3. Methods
Intermountain Healthcare is a not-for-profit integrated health care delivery system consisting of 21 hospitals (2200 beds) and more than 90 outpatient clinics in Utah and Idaho. Its facilities range from major adult and pediatric tertiary-level teaching/research facilities to small rural hospital/clinics, and it provides more than 50 percent of all care delivered in the region. Intermountain has extensive clinical information systems, and a history of using those information systems to improve patient care [16–19]. Inpatient and outpatient clinical data is interfaced to a longitudinal patient record and stored in the Clinical Data Repository (CDR), which contains records for 2.5 million patients. Desktop applications allow users in either inpatient or ambulatory settings to view laboratory results, text reports, and radiology images, regardless of where the care was provided. Over 13,000 providers use the clinical information system at Intermountain each month to access the records of 331,000 patients. Because it provides a breadth of services to a large proportion of people within a well-defined area, and has extensive availability of clinical information within those services, Intermountain is a good example of health information integration and exchange across clinical sites and services.
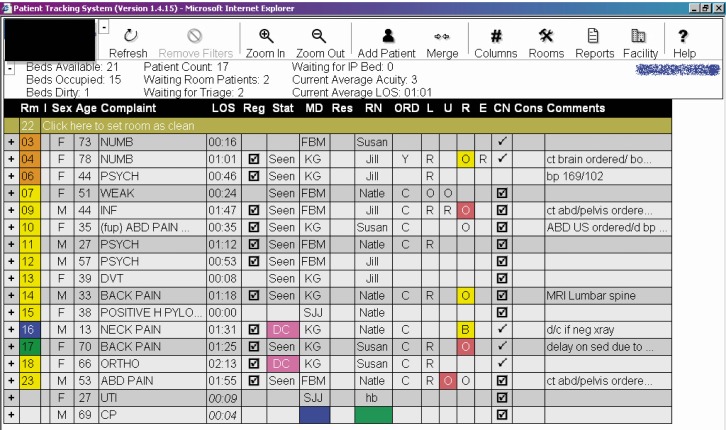
In 2003, Intermountain began development of an emergency department information system, or EDIS, with the goal to integrate it with the existing functionality of the outpatient and inpatient information systems that were already in use. The main component of the EDIS was a patient tracking system to monitor patients’ status and location while in the ED (►Fig. 1). The patient tracking system also monitors the availability of longitudinal patient information in the form of text reports from previous inpatient or outpatient visits in the CDR, and alerts to the availability of that data within HELP-2, Intermountain’s web-based EHR. The first implementation of the patient tracking system was at LDS Hospital, a tertiary care hospital located in Salt Lake City, Utah. The patient tracking system was initially implemented in December 2003, and later updated in May 2004 to provide simplified access to longitudinal data within the CDR applications. This updated system provided simplified access whereby a provider could access a patient record within HELP-2 through the tracking system simply by selecting the patient’s data, and then touching a proximity card to an attached detector. Previously, clinicians were required to manually change to the second application, authenticate, and then navigate to the patient system.
Fig. 1.
Patient tracking system implemented at the emergency department at LDS Hospital in Salt Lake City, Utah. The tracking system is an interactive display, with data indicating patient condition and acuity, assigned clinicians, length of stay, and available information within the longitudinal patient record (CN column).
After successfully implementing the patient tracking system, we retrospectively analyzed the proportion of ED patients for whom longitudinal data was accessed during ED visits at LDS Hospital, with this simplified method of data access. We also analyzed the effect of this access on the ED admission rate, presuming that information about previous encounters could influence the ED disposition decision. We defined the control period as January 1 through April 30, 2004, when the patient tracking system gave notification of the availability of longitudinal patient health information, but required manual authentication and patient selection. To account for seasonal variation between ED patient visit types, we defined the intervention period as one year later, from January 1 through April 30, 2005. During the intervention period, clinicians could access patient records through the simplified process using proximity cards. For each period, we analyzed audit records of patient data access during the time of the ED visit. ED visit times were calculated from patient admission and discharge times as recorded in the patient tracking system, which was in real use during both control and intervention periods. Patients with missing data were excluded from the analysis.
We also analyzed the impact of improved access to longitudinal patient information on the odds of inpatient admission, using the same control and intervention periods. For each patient, we collected patient age, sex, admit and discharge time, triage acuity, number of laboratory orders (a measure of resource consumption, which is related to patient complexity) [20], whether a patient had longitudinal information available in the CDR at the time of the ED visit, whether a clinician accessed the patient’s longitudinal record during the ED visit, disposition (discharge or admit), discharge diagnoses, and inpatient charges. A logistic regression, using covariates of age, sex, acuity, and lab volume, modelled the probability of being admitted in the control and intervention periods, using the control period as a reference.
A third analysis classified patients in the pre-post groups separately according to whether they had an ambulatory-care sensitive (ACS) condition, or whether they had previous longitudinal data available at the point of the ED visit, and evaluated their odds of inpatient admission. This was done to address confounders, by measuring the impact among groups of patients most likely to be influenced by the intervention. ACS conditions were used to identify patients for whom admission decisions would be more likely affected by the understanding of the current outpatient plan of care. We identified ACS conditions within any of the top 4 discharge diagnoses (ED or inpatient) included an ICD-9 code relating to ACS conditions as defined by the Agency for Healthcare Research and Quality [21, 22]. Odds ratios were obtained similarly to the prior analyses, using the same covariates of age, sex, acuity and lab order volume.
4. Results
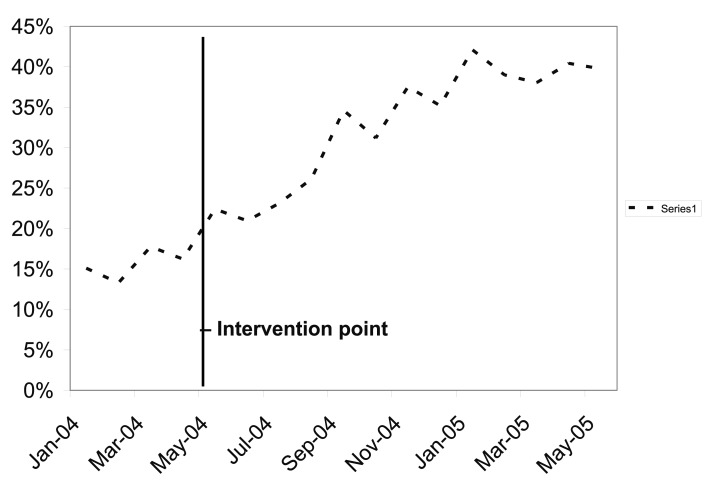
During the control period (1/1/2004–4/30/2004), there were 12,622 patient visits to the Emergency Department at LDS Hospital, and 13,201 patient visits during the intervention period (1/1/2005–4/30/2005). Due to either random system maintenance periods, or patients leaving without treatment, we were missing some data for about 10% of patient visits. After case deletion for missing data, we had 10,928 control and 11,415 intervention patient visits. Longitudinal patient information was accessed for 16% and 40% of ED patients during control and intervention periods, respectively. ►Figure 2 shows the increase in access to patient information during and between the control and intervention periods. Access to patient records was influenced by the patient’s triage acuity; the access increased as the triage acuity increased, except for patients with the highest acuity (resuscitation), where access was lowest (►Table 1).
Fig. 2.
Proportion of ED patients where longitudinal patient information was accessed during the ED visit. This proportion rose from around 15% just after implementation of the use of the patient tracking system, to around 40%. The vertical line indicates the intervention point of the study.
Table 1.
Undjusted odds ratio of longitudinal patient data being accessed during an ED visit, based on triage acuity. Odds ratios are relative to the lowest acuity level, non-urgent. Clinicians were more likely to access patient records as triage acuity increased, except in the highest acuity level (resuscitation), where the odds of access was actually lower.
| Acuity | Odds ratio (95% CI) |
|---|---|
| Non-urgent | Reference |
| Semi-urgent | 1.33 (1.03–1.73) p = 0.0297 |
| Urgent | 1.71 (1.33–2.20) p<0.0001 |
| Emergent | 2.01 (1.503–2.64) p<0.0001 |
| Resuscitation | 0.82 (0.45–1.52) p = 0.53 |
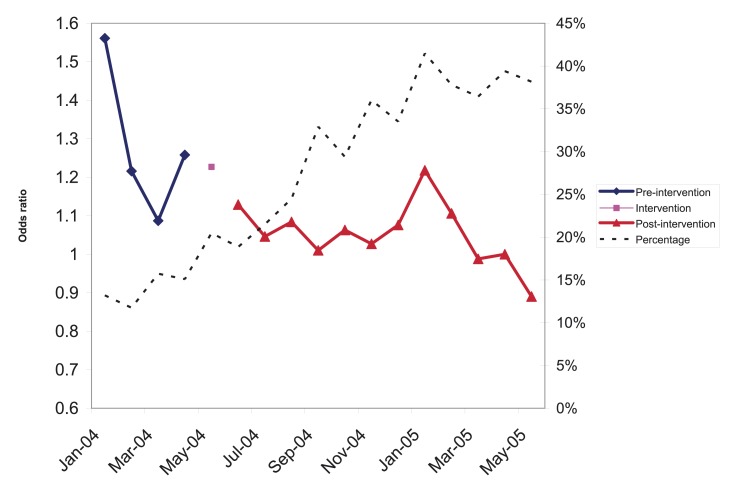
The odds of inpatient admission in the intervention period compared to the control period was 0.761 (95% confidence interval: 0.684–0.846); i.e., there was a 23.9% decrease in the odds of admission concurrent with improved access to longitudinal patient information. ►Figure 3 shows the calculated odds ratio for admission for each month between the control and intervention periods.
Fig. 3.
Odds ratio of inpatient admission before and after implementation of improved longitudinal patient access from the ED, with proportion of ED patients where longitudinal patient information was accessed (see Figure 2). April 2005, the last month in the intervention period, was used as the reference.
►Table 2 shows the control and intervention patients stratified by whether there were previous records available at the ED visit, and whether the patient had an ACS condition. Patients with a previous record available were less likely to be admitted, whether or not they had an ACS condition. Odds of admission were not different for patients without previous records and without ACS conditions, but patients with ACS conditions (and no previous record) were more likely to be admitted.
Table 2.
Odds ratio of inpatient admission from the emergency department for intervention period relative to control period, stratified by whether a previous record was available, and whether the patient was diagnosed with an ACS condition.
| Ambulatory care sensitive diagnosis (ACS) (95% CI) | Not ACS diagnosis (95% CI) | |
|---|---|---|
| Previous record | OR: 0.690 (0.548–0.869) p = 0.0016 n = 3544 |
OR: 0.766 (0.670–0.876) p<0.0001 n = 13224 |
| No previous record | OR: 2.003 (1.012–3.965) p = 0.046 n = 600 |
OR: 0.739 (0.543–1.005) p = 0.0542 n = 3146 |
5. Discussion
This case study indicates important considerations for longitudinal electronic health record initiatives in the emergency department setting. The system provided access to longitudinal patient information, from outpatient visits, inpatient stays, and/or previous emergency department visits. We assessed the proportion of patients for whom clinicians retrieved longitudinal information for different approaches of providing data access. Our implementation of the ED patient tracking system did not provide access to data that was otherwise unavailable – clinicians already had access to the desktop application and longitudinal data within the CDR prior to the tracking system – it simply provided easier access to it. Providing notification of the presence of data led to a modest increase in access to data (January 2004 – April 2004), and the rate of access increased further once the barriers of patient identification and user authentication were removed.
Our study occurred within an integrated delivery system, where health information access is facilitated by shared systems using a centralized data repository. However, most information access and deficits in EDs occurs outside of integrated delivery networks, where information is not as accessible. Health information exchange (HIE) initiatives have attempted to address this challenge, and multiple studies have measured the rate of information access in such settings [4, 23–27]. These rates have varied between <3% and 7%, with estimates of access by physicians as high as 10% [26]. Some of these studies also noted that access was greater for more complex patients [25, 27]. These findings were consistent with our findings, both that the access was more common among patients with higher acuity, and low access levels (access in our system was between 10–15% with notification of available data at the beginning of the study).
The low rate of access in these studies and at the beginning of our study illuminates the significance of the findings of this study. If access to data is sufficiently facilitated, the data will be used. Vest et al. showed that in systems where users were not informed of data availability, their greatest interaction with the information exchange data was searching for whether data were available [28].
Hincapie et al. found that physicians felt use of HIE was inefficient because of significant time spent searching for information that may have been available. Systems that informed the availability of information had higher use than systems that did not, but these were still less than what we observed when the access was simplified further by passing patient, user and data context.
Johnson et al. studied HIE in an ED where clinicians were notified that data were present from different institutions or settings, and found a modest level of usage (6.8% of visits). This lower level of access might be ascribed to two differences in their system: a) it notified of available data during the entry to the patient record, but did not show it in the context of the patient data, and b) it didn’t facilitate direct access to the data.
We had previously studied rates of access at another institution, and found usage close to our rate in the ED (20–50%). This was also in an institution where the data were integrated from different settings, but not necessarily from different institutions (e.g., data access within an integrated delivery system rather than information exchange across organizations [30]. Our access rates of ~40% show that access to HIE could increase substantially if sufficiently facilitated. Our observed decreased admissions, which appear much greater than those observed in a similar study by Overhage et al., might be due to the difference in the use of the data [4]. HIE initiatives that do not notify of the availability of external data, or do not facilitate users accessing that data, should expect lower rates of use for their systems, and a decreased impact as well.
This study also is important because it measures the potential savings of the availability of information access in the emergency department experimentally. Despite the great promises of potential benefit, there is a dearth of studies measuring the actual impact of health information exchange [29]. We observed decreased odds of inpatient admissions coincident with the increased availability of longitudinal patient health information in the emergency department setting. These results support an important assumption related to the use of health information exchange to improve clinical efficiency and decrease costs [12]. HIE benefits in the emergency department are important components of many studies estimating the benefits of HIT. Frisse et al. estimated savings due to reduced admissions from the ED at 20–25% of the total benefit of HIE [6]. Frisse et al. did measure the financial impact of HIE in EDs participating in the MidSouth eHealth Alliance, and found substantial savings. However, rates of access in that study were substantially lower than our rates of access, and may represent just a lower bound of the potential, while these results may reflect what is more possible with facilitated data access [23].
Our results, though, should be interpreted cautiously. There are several weaknesses to this part of the study, mostly related to the pre-post design. The observed decrease in the likelihood of inpatient admission could be part of a historical trend at the specific hospital, among hospitals within the region or Intermountain network, or nationally. Ideally, we would have performed a prospective, randomized controlled trial to reduce these weaknesses. However, such an approach would have been difficult, as the evaluation was not the purpose of the system implementation, nor were we able to a priori direct the implementation plan in a way that we could have performed the study otherwise.
The sponsors of the project were insistent on a rapid implementation period. Even if we able to do a randomly-controlled evaluation, it is unclear whether a difference could be detected. The seasonal variation and differences in admission rates between facilities are both greater than the potential differences due to the intervention. Another approach would have been to compare with other EDs in the Intermountain network; however, the comparable EDs during the intervention period did not have sufficient granularity in the log files to identify what data clinicians used. In addition, we wanted to separate out the indication of available data to facilitated access to that data in the intervention.
We tried to mitigate the risks of confounders by analyzing the specific point of the intervention, and comparing populations where the intervention would most likely have an effect. ►Figures 2 and 3 show that the use of the intervention and the decreased odds of admission were both gradual, so it is difficult to identify a specific point in time where the effect of the intervention can be identified. Month-to-month changes may be more likely due to seasonal changes than to the incremental increase in the use of the intervention. We instead stratified by the availability of patient information, and the conditions that would be most likely to be affected. Since the intervention specifically facilitated access to longitudinal patient records, we expected that the effect of the intervention should be isolated to patients who had such longitudinal patient records available.
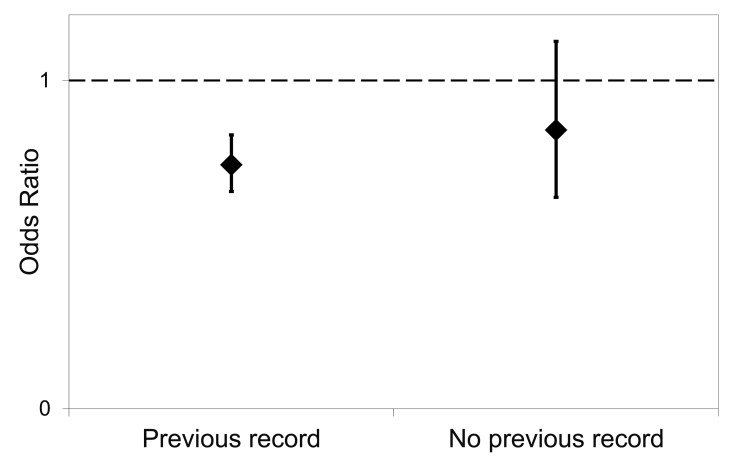
Indeed, as ►Figure 4 shows, the effect is significant with this population, and not significant for patients without previous records available. However, the observed difference between the odds ratios of those with and without records available is not significant, implying either that there was not sufficient power in this study to detect a difference, or that there are other factors contributing to the decreased odds of admission, or both.
Fig. 4.
Odds ratio of inpatient admission from the emergency department for intervention period relative to control, stratified by whether a previous record was available.
We also stratified patients by whether the patient was seen for an ambulatory-care sensitive (ACS) condition, with the assumption that admission decisions for those conditions would be more likely affected by the understanding of the current outpatient plan of care. For patients with ACS conditions, there was a significant difference in the odds ratios for admission between those with and without patient records available. This finding supports an interpretation that the intervention influenced the admission rate, because the observed difference was greatest where we anticipated the intervention would have the biggest effect. However, the nearly-significant decrease among patients without previous records and with non-ACS conditions implies there are some confounding factors that may also be contributing to a decreased odds of admission over time.
6. Conclusion
Ease of access is an important factor in achieving successful health information exchange in the emergency department. Emergency clinicians were more likely to access information when they did not have to manually authenticate and select patients within a different system. We also observed a decrease in the odds of inpatient admission from the emergency department after the implementation of improved access to longitudinal patient health information, but further research is needed to more accurately measure the effect relative to other confounding effects. Our experience, though not conclusive, is promising. Future studies could more conclusively identify the impact of information in ED settings on health care utilization, as well as elucidate the patient factors that may be most associated with information needs from existing patient records.
Clinical Relevance Statement
Health information exchange has been suggested as an important factor in improving quality and decreasing costs of care. In the emergency department, one potential opportunity for influence is the decision to discharge patients to outpatient care or to admit to a hospital, a decision which has marked cost differences in options. We found that by improving ease of access to health information from previous clinical encounters, emergency clinicians were more likely to access information when they did not have to manually authenticate and select patients within a different system, and observed a decrease in the odds of inpatient admission from the emergency department after the implementation of improved access to longitudinal patient health information. While further research is needed to more accurately measure the effect relative to other confounding effects, our experience is promising.
Conflicts of Interest
The authors declare they have no conflicts of interest in the research.
Protection of Human Subjects
This was a retrospective analysis of a non-research implementation of a health information resource. Institutional review board approval was obtained for the study, and the conduct of the study followed the IRB guidelines. The primary risk to subjects was privacy and confidentiality of information, and we followed approved methods for securing any protected health information in the study.
Acknowledgments
Portions of this data regarding the rate of access to longitudinal data were presented at the 2006 AMIA Fall Symposium, as part of the paper “Architectural strategies and issues with health information exchange,” by Wilcox et al. [31].
References
- 1.Bush G.Executive Order: Incentives for the Use of Health Information Technology and Establishing the Position of the National Health Information Technology Coordinator In: Secretary OotP, editor. Washington, DC: 2004. [Google Scholar]
- 2.Marchibroda J, Bordenick JC. Emerging trends and issues in health information exchange: selected findings from eHealth Initiative foundation's second annual survey of state, regional and community-based health information exchange initiatives and organizations. Foundation of eHealth Initiative, Washington, DC, 2005. [Google Scholar]
- 3.Shapiro JS, et al. Regional health information organizations, health information exchange and the impact on emergency medicine. Ann Emerg Med 2006; 48(4): 426–432 [DOI] [PubMed] [Google Scholar]
- 4.Overhage JM, et al. A randomized, controlled trial of clinical information shared from another institution. Ann Emerg Med 2002; 39(1): 14–23 [DOI] [PubMed] [Google Scholar]
- 5.Thompson CA. Regions work to exchange health information. Am J Health Syst Pharm 2005; 62(8): 788, 90,, 92 [DOI] [PubMed] [Google Scholar]
- 6.Middleton B, Frisse M, Kolodner R, Rollow W.Realizing the financial benefits of electronic health records: what do the data show?: American Medical Informatics Association; 2005. [Google Scholar]
- 7.Kuperman GJ, Lipton MS. The New York Clinical Information Exchange (NYCLIX): An Overview. 2006[cited 2006]; Available from: http://www.svcmc.org/documents/for%20our%20physicians/nyclix_101.pdf
- 8.Coleman EA. Falling through the cracks: challenges and opportunities for improving transitional care for persons with continuous complex care needs. J Am Geriatr Soc 2003; 51(4): 549–555 [DOI] [PubMed] [Google Scholar]
- 9.Shablinsky I, Starren J, Friedman C.What do ER physicians really want? A method for elucidating ER information needs. Proc AMIA Symp 1999: 390–394 [PMC free article] [PubMed] [Google Scholar]
- 10.Stiell A, Forster AJ, Stiell IG, van Walraven C.Prevalence of information gaps in the emergency department and the effect on patient outcomes. Cmaj 2003; 169(10): 1023–1028 [PMC free article] [PubMed] [Google Scholar]
- 11.Asplin BR, et al. Insurance status and access to urgent ambulatory care follow-up appointments. Jama 2005; 294(10): 1248–1254 [DOI] [PubMed] [Google Scholar]
- 12.Walker J, et al. The value of health care information exchange and interoperability. Health Aff (Millwood). 2005Jan-Jun; Suppl Web Exclusives:W5–10-W5–8 [DOI] [PubMed] [Google Scholar]
- 13.Frisse M.Technical Discussion: State and Regional Demonstrations in Health Information Technology. Nashville, TN2004 [cited 2006]; Available from: http://www.volunteer-ehealth.org/pdfdocs/AHRQ-10–30–04.pdf
- 14.Kawamoto K, Houlihan CA, Balas EA, Lobach DF. Improving clinical practice using clinical decision support systems: a systematic review of trials to identify features critical to success. BMJ 2005; 330(7494): 765 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Treister NW. Physician acceptance of new medical information systems: the field of dreams. Physician Exec 1998; 24(3): 20–24 [PubMed] [Google Scholar]
- 16.Evans RS, et al. A computer-assisted management program for antibiotics and other antiinfective agents. N Engl J Med 1998; 338(4): 232–238 [DOI] [PubMed] [Google Scholar]
- 17.Clayton PD, et al. Building a comprehensive clinical information system from components. The approach at Intermountain Health Care. Methods Inf Med 2003; 42(1): 1–7 [PubMed] [Google Scholar]
- 18.Haug PJ, et al. Decision support in medicine: examples from the HELP system. Comput Biomed Res 1994; 27(5): 396–418 [DOI] [PubMed] [Google Scholar]
- 19.Kuperman GJ, Maack BB, Bauer K, Gardner RM. Innovations and research review: the impact of the HELP computer system on the LDS Hospital paper medical record. Top Health Rec Manage 1991; 12(2): 76–85 [PubMed] [Google Scholar]
- 20.Eitel DR, et al. The emergency severity index triage algorithm version 2 is reliable and valid. Acad Emerg Med 2003; 10(10): 1070–1080 [DOI] [PubMed] [Google Scholar]
- 21.Kruzikas D, et al. Preventable hospitalizations: A window into primary and preventive Care, 2000. 2004 AHRQ Publication No. 04–0056; [Google Scholar]
- 22.Billings J.Using administrative data to monitor access, identify disparities, and assess performance of the safety net. Tools for Monitoring the Health Care Safety Net. Rockville, MD: Agency for Healthcare Research and Quality, 2003. [Google Scholar]
- 23.Frisse ME, et al. The financial impact of health information exchange on emergency department care. J Am Med Inform Assoc 2012; 19(3): 328–333 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Johnson KB, et al. Health information exchange usage in emergency departments and clinics: the who, what, and why. J Am Med Inform Assoc 2011; 18(5): 690–697 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Vest JR, et al. Factors motivating and affecting health information exchange usage. J Am Med Inform Assoc 2011; 18(2): 14314–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Shapiro JS, Kannry J, Kushniruk AW, Kuperman G.Emergency physicians' perceptions of health information exchange. J Am Med Inform Assoc 2007; 14(6): 700–705 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hincapie AL, et al. Physicians' opinions of a health information exchange. J Am Med Inform Assoc 2011; 18(1): 60–65 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Vest JR, Jasperson JS. How are health professionals using health information exchange systems? Measuring usage for evaluation and system improvement. J Med Syst 2011 Nov 30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hincapie A, Warholak T.The impact of health information exchange on health outcomes. ACI 2011; 2(4): 499–507 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hripcsak G, Sengupta S, Wilcox A, Green RA. Emergency department access to a longitudinal medical record. J Am Med Inform Assoc 2007; 14(2): 235–238 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wilcox A, Kuperman G, Dorr DA, et al. Architectural strategies and issues with health information exchange. AMIA Annu Symp Proc 2006: 814–818 [PMC free article] [PubMed] [Google Scholar]