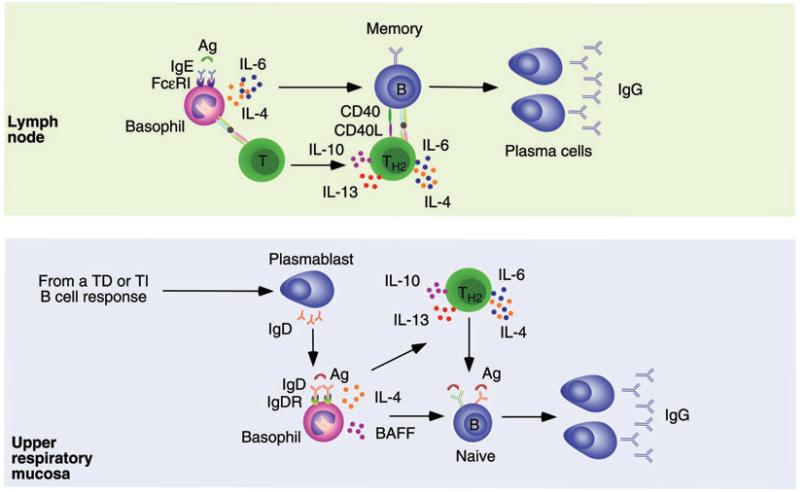
Figure 4.
Basophils provide help to lymph node and mucosal B cells. Upper panel. Basophils bind to IgE generated during a primary immune response through a high-affinity receptor named FcRI. In a secondary immune response, binding of recall antigen to IgE via either conventional or unconventional mechanisms triggers basophil release of IL-4 and IL-6, which enhances the conversion of naïve T cells into TH2 cells secreting IL-4, IL-6, IL-10, and IL-13. Together with CD40L, these cytokines enhance the activation and expansion of IgG-expressing memory B cells in the context of a cognate interaction that leads to the generation of IgG-secreting plasma cells. Basophils may further enhance the activation of memory B cells by delivering helper signals independently of T cells. Bottom panel. B cells from the human upper respiratory mucosa undergo noncanonical CSR from IgM to IgD by following either TD or TI pathways. This process leads to the formation of mucosal and circulating plasmablasts that secrete IgD antibodies reactive against respiratory bacteria. Mucosal IgD would enhance local immunity and homeostasis after translocating across epithelial cells, whereas circulating IgD binds to basophils via an unknown receptor (IgDR). In addition to delivering rapid innate responses and alerting the immune system as to the presence of invading bacteria, basophils exposed to IgD-reactive antigens may enhance immune responses in both systemic and mucosal lymphoid organs. These basophils enhance IgG (but also IgA) CSR and antibody production by activating B cells via BAFF, IL-4, and other B-cell-activating factors, including CD40L and APRIL (not shown). Similar to IgE-stimulated basophils, IgD-stimulated basophils might further enhance the local antibody response by promoting the formation of TH2 cells via IL-4.