Abstract
Introduction: There has been a recent increase in interest in implementing organized geriatric fracture programs for care of older adults with fragility fractures in order to improve both the quality and costs of care. Because such programs are relatively new, there are no standardized methods for implementation and no published descriptions of barriers to implementation. Materials and Methods: An online survey tool was sent to 185 surgeons and physicians practicing in the United States, who are involved with geriatric fracture care. Sixty-eight responses were received and evaluated. Results: Barriers identified included lack of medical and surgical leadership, need for a clinical case manager, lack of anesthesia department support, lack of hospital administration support, operating room time availability, and difficulty with cardiac clearance for surgery. Other issues important to implementation included quality improvement, cost reductions, cost to the hospital, infection prevention, readmission prevention, and dealing with competing interest groups and competing projects mandated by the government. Physicians and surgeons felt that a site visit to a functioning program was most important when considering implementing a hip fracture program. Conclusions: This study provides useful insights into barriers to implementing an organized hip fracture program. The authors offer suggestions on ways to mitigate or overcome these barriers.
Keywords: fragility fractures, systems of care, geriatric fracture program, orthogeriatrics, barriers, implementation science
Introduction
A geriatric fracture program is a model of acute care for older adults with a fragility fracture.1 Such programs include comanaged care with surgeons and medical physicians, early surgical intervention, patient-centered care using standard protocols, and early discharge planning to reduce the length of hospital stay.1–3
There are a number of publications suggesting that an organized model of geriatric fracture care improves quality of care and lowers costs.4,5 There is increasing interest in development and implementation of geriatric fracture programs.6 This seems partially driven by economic concerns and partially driven by quality-of-care concerns. Globally, there are many models of comanaged care that have been described.6 These programs offer various benefits and challenges to the health care system, patients, and physicians.6 This article seeks to determine the barriers to implementation of a geriatric fracture program.
The population is rapidly aging.7 This demographic shift has influenced health care systems, physicians, and governments considerably over the past 5 years. As the population ages, so will the number of older patients sustaining a fragility fracture.8,9 Hip fractures are common and problematic events for older adults. They are also the most costly fractures to care for in a health care system.10–14 Several authors have published reports that an organized geriatric fracture program offers improved care to patients with a hip fracture.1–3,6 These authors cite reduced rates of complications, mortality, and length of stay.6,15 There are at least 2 reports that such programs also reduce costs of care.4,5 In most Western countries today there are great concerns about the costs of care as well as the quality of care.5,11 Better quality of care appears to be linked with lower cost.5 Thus there is increasing interest in pursuit of a better system of care for the hip fracture in older adults. The authors of this article have been involved with implementation of geriatric fracture programs at many other institutions. There appear to be multiple barriers to implementation of such programs at the different institutions; some impediments are similar in nature and others unique to the particular institution. These variations in the barriers to implementation of an organized program have prompted the authors to investigate further.
The authors aim to explore the barriers to establishing an organized hip fracture program and to recommend appropriate countermeasures that can be taken to mitigate or overcome these barriers to implementation.
Materials and Methods
Setting: United States
Surgeons and physicians surveyed
In total, 185 orthopedic surgeons and medical physicians were surveyed for the study. Recipients were selected from professional society e-mail lists and from personal previous contact with the authors. Many of these physicians and surgeons had previously expressed an interest in developing an organized geriatric fracture program at their institution. The responses to the survey were reviewed by the authors and studied for similar patterns of responses.
Survey instrument
The authors created a 10-question online survey through Survey Monkey (California). Survey questions were developed based on experiences and discussions that the authors had during educational events, site visits, and professional meetings. Respondents were asked for information about their site, such as the size of the hospital, level of trauma center, and stage of implementation of a geriatric fracture program. They were asked about barriers and items that would be helpful in starting a program. The survey questions are listed in Table 1. For questions 4 and 5, respondents could choose as many barriers as they felt applicable, and grade their significance from not important to critical. Some of the responses are also presented in graphic format in Figures 1 to 4.
Table 1.
Survey Sent to Physicians and Surgeons
| Questions asked via online survey | |
|---|---|
| 1 | Have you implemented a geriatric fracture center (GFC) program? |
| 2 | Does your hospital collect data on quality and/or cost of care for fragility fractures? |
| 3 | Which time frame is most important to perform hip fracture surgery? |
| 4 | Rate the following as barriers to implementing a fracture program or improving fracture care at your institution:
|
| 5 | When considering a program to implement at your hospital to improve hip fracture care, how important are the following?
|
| 6 | What would be most helpful to you when considering implementing a hip fracture program?
|
| 7 | How well accepted are standardized protocols and orders at your institution? |
| 8 | What level trauma center is your hospital? |
| 9 | Tell us about the size of your hospital/program as best as you know. Approximate numbers are fine. |
| 10 | Please share any thoughts or comments about your program. |
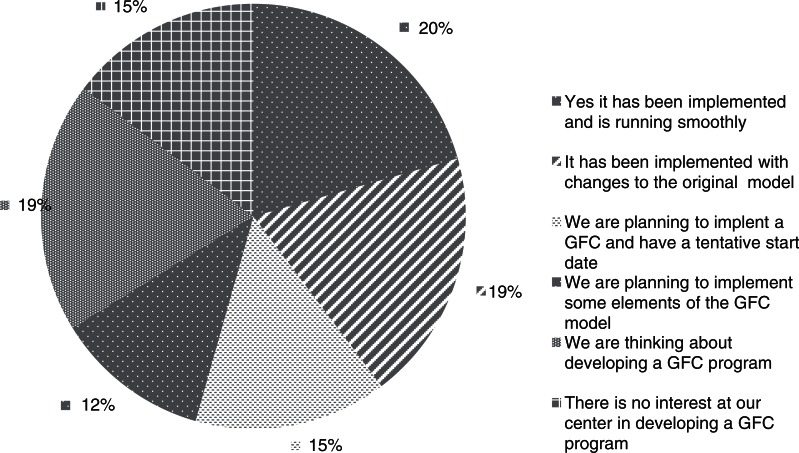
Figure 1.
Have you implemented a geriatric fracture program?
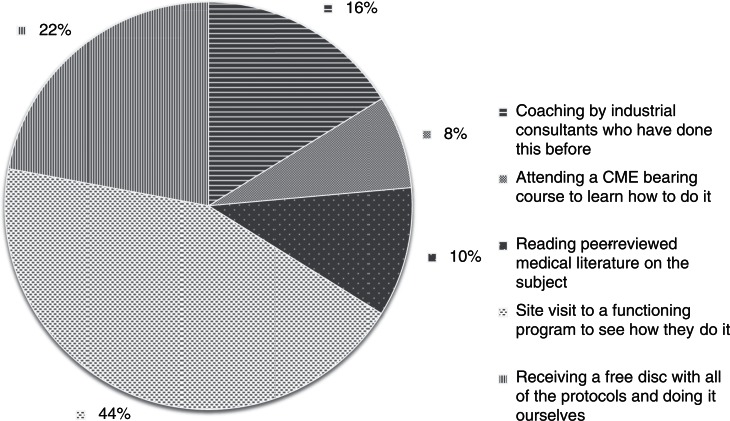
Figure 4.
The most important factors to consider when implementing a hip fracture program.
Once the responses were examined, appropriate countermeasures to these barriers were suggested and are discussed.
Results
Hospital Size
The respondent’s hospital had, on average, a 532-bed capacity with 22 operating rooms. The average number of trauma cases per annum presenting at the respondents’ institutions was 1824. The average hospital represented by the respondents had 16.5 orthopedic surgeons and 9.5 surgeons who shared trauma call, with only 2.3 geriatricians and 14 hospitalists on staff. The average number of fragility fractures treated at the respondent hospitals was 336 per year.
Forty percent of the respondents indicated that they had already implemented a geriatric fracture program. Twenty-six percent of the respondents indicated that they were planning to develop a geriatric fracture program in some form, while 19% were considering implementation. Fifteen percent of the respondents indicated that they were not planning to develop a geriatric fracture program (Figure 1). Forty-seven percent of the respondents indicated that their hospital already collected detailed quality and financial data about their fracture patients. Twelve percent indicated that only quality data were collected, while 3% indicated that the cost of care data was collected. Only 24% indicated that they did not think their hospital actually collected data and nearly 15% were not sure. When asked about the timing of hip fracture surgery, most of the respondents (91%) felt that early surgery (within 48 hours of admission) was best.
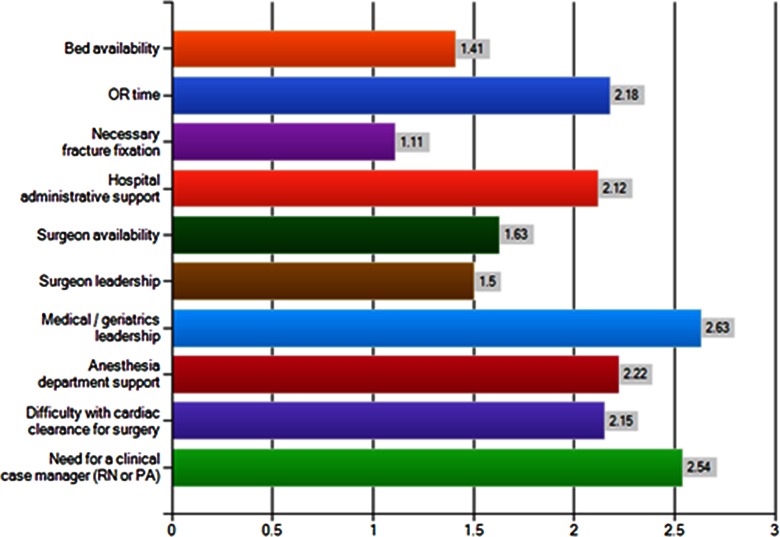
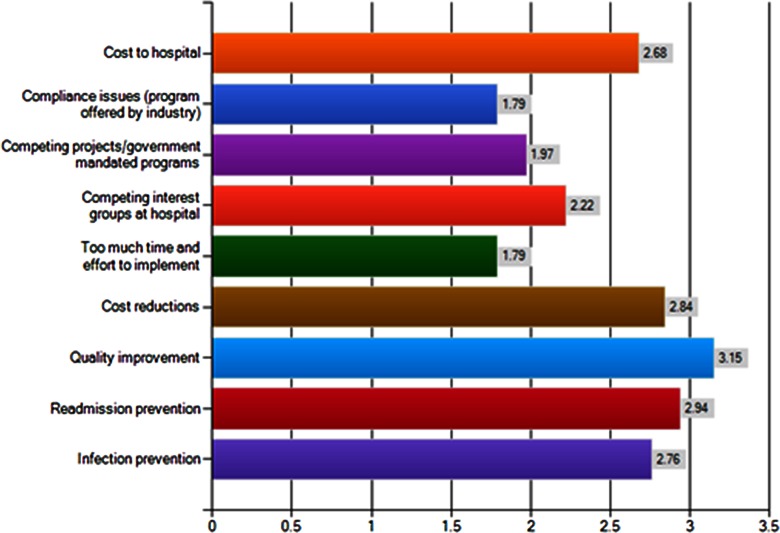
When specific barriers to implementing a fracture program or improving fracture care at their institution were queried, the most frequently cited reasons were a lack of physician leadership (79%), need for a clinical case manager (78%), lack of anesthesia department support (71%), operating room time availability (71%), problems with cardiac clearance (76%), and a lack of hospital administrative support (62%; Figure 2). When physicians were asked how important certain factors were when considering implementing an organized fracture program at their hospital, the following were listed as most important in order: quality improvement, readmission prevention, cost reductions, infection prevention, competing interests at the hospital, and too much time and effort to implement such a program (Figure 3). Of the 40% who had already implemented a program, the “severe barriers” identified were of operating room time access (15%), difficulty with cardiac clearance for surgery (7.4%), the need for a clinical case manager (11%), and the need for medical or geriatric leadership (15%). Interestingly, most of this subgroup did not see surgeon leadership (82%) or hospital administration (56%) as a barrier to implementation of their programs.
Figure 2.
Rate the following as barriers to implementing a fracture program or improving fracture care at your institution. Rating average, where 1 = not a barrier; 2 = minimal barrier; 3 = moderate barrier; and 4 = severe barrier.
Figure 3.
When considering a program to implement at your hospital to improve hip fracture care, how important are the following items: rating average, 1 = not important; 2 = moderately important; 3 = very important; and 4 = critical.
When asked what factors would be most helpful when considering implementing a hip fracture program, 44% believed a site visit to a functioning program in order to observe “how they do it” was most important. Twenty-two percent of the respondents felt that receiving a free disc with all the protocols was extremely important. Sixteen percent felt that coaching by industrial consultants who had done this before was important and 10% felt that reading the peer-reviewed medical literature would be beneficial. Only 7% of the respondents felt that attending a continuing medical education course to learn how to do it was valuable (Figure 4).
When asked how well accepted standardized protocols and orders were at their institution, 78% of the respondents reported that they were either very well accepted or were used in some programs but not for a geriatric fracture program; only 3% used standard protocols for geriatric fracture program; 10% felt that protocols would probably be well accepted but have not been used; and 9% felt it would be very difficult to use standard protocols due to difficulty with provider “buy in.”
Respondents to this survey were predominantly working at a level I or level II trauma center with 62% being from a level I trauma center, 34% level II trauma center, and only 4% respondents working at a level III trauma center. Given the small number of respondents from level III centers, comparisons were only made between level I and II centers. This surprisingly demonstrated the anesthesia department support to be less of a barrier in a level II center than in level I, and medical/geriatric leadership to be more of a barrier in level I centers.
As a final part of the survey, a free text section was provided. Comments included a feeling of hopefulness for starting the program in 2012 and the positive nature of doing a site visit to a successful program. One written comment noted difficulty with “town–gown” (nonacademic vs academic) issues preventing full implementation as well as the need for additional evidence basis for the protocols, the difficulty in obtaining a consensus among private practitioners, and interest in being part of studies on such programs. Other comments offered included a difficulty with “turf wars,” poor leadership, and a lack of wisdom preventing change. Several respondents had complaints about the emergency room at their facility and of difficulties with private practitioners of internal medicine, for example “lack of interest among the community physicians.” Some physicians expressed concerns about political problems at their institution and difficulties with ingrained habits and practice patterns of the surgeons.
Discussion
Although only a small, select sample of surgeons and physicians in the United States were surveyed, the responses and comments made by this group highlight some important barriers to implementation of an organized geriatric fracture program. There is presently no registry or directory of these programs in the United States; there are only reports of the success of individual programs published in the medical literature.1,6,16 This survey studied physicians and surgeons practicing in the United States, regarding their attitudes and interest as well as barriers to implementation of an organized geriatric fracture program. Concerns that will be discussed include leadership, building consensus among physicians, obtaining hospital administration support, costs of implementation, dealing with cardiac clearance and anesthesia issues, operating room data collection, and methods of implementation. These barriers including the countermeasures that can be employed to overcome them will be discussed below. By following these methods listed below in a step-by-step manner, the process of implementing a geriatric fracture program will be greatly simplified.
Leadership has been listed as a great area of concern. It is likely a very important determinant of long-term success. Selection of the proper leaders for implementing a geriatric fracture program is the critical first step in planning.1,17 It is recommended that a committed surgeon “champion” and medicine “champion” be selected at the early development stages of such a program.17 These “champion” physicians should target the need to improve the quality and safety of patient care. The leaders should be in a position to build the required consensus among their colleagues despite competing interests. Only by building a consensus among peers can a program be successful. Building consensus among the surgeons and medical colleagues is another critical early step in program development. Consensus is best achieved by emphasizing the benefits of such a program to them and their patients. Leaders should be accessible, reliable, and credible.
Lack of hospital administration support was also identified as a barrier to implementation of a geriatric fracture program. It is important for the hospital administration to understand the multitude of benefits that can be realized when improving the system of care for older adults.1 These proven benefits include improved quality of care, reduced length of stay, reduced readmission rates, and improved costs of care.3 Improved quality at a better cost represents improved value of care.4 As the US health care system shifts focus toward value-based purchasing, all improvements in value of care will be very important for each hospital to consider.4 When planning to start a program, the support of the hospital administration should be sought early in the process. This will be an essential step. Administration can facilitate access to quality and financial data and assist with preparation of a business plan for the program. It is the administration that will finance the project and help various departments work together cooperatively. Administration will need to support any board approval process that is required.
Hospital administrations are currently occupied with meeting governmental mandates and adjusting to the rapidly shifting “health care reforms” and may not have the capacity to undertake the implementation of a geriatric fracture program. Getting the geriatric fracture program into the queue of projects at a hospital can be a challenge, but it is quite possible with persistent and determined surgeon and physician leadership.
Presently, these programs are implemented differently throughout the United States.1,16,18 No standardized model has been developed and proven to be most effective.6 Many of the current programs have been implemented with the assistance of industrial consultants or in some cases the programs have been implemented with industrial assistance as a “value-added service.” In other cases, the hospital or hospital systems have been charged for the services of the industrial consultants when implementing the program. Cost of implementation was mentioned by many of the responding physicians, as was cost of care a great area of concern. The actual costs of implementing an organized fracture program are quite dependent on existing resources that are already present at the implementing hospital, for example if the hospital already has adequate surgical and medical specialists needed to staff such a program, incremental costs to the hospital will be low. Should the hospital choose to establish a more robust data collection system, an increase in ongoing incremental cost would occur. Additionally, if a case manager was to be hired to oversee the day-to-day activities and in-hospital journey of each patient, this would represent further incremental costs. Many programs have chosen to designate an experienced nurse or mid-level provider to serve in this role rather than hiring new personnel to perform these duties. This is a good strategy in our opinion and keeps the incremental costs low. Seeking the assistance of an experienced industrial consultant can be very helpful and may actually reduce the overall costs of implementation.
It is important to have support from the anesthesia department at the implementing hospital.19 The anesthesiologists must view themselves as partners in the patient journey and should be comfortable in providing the necessary and appropriate anesthesia care for the older adult with a fracture. It is important for the anesthesia specialists to understand the need for urgent surgery to reduce the patient’s perioperative risk. “Timing of surgery” literature should be discussed with the anesthesiologist to help with the acceptance of the need for early surgical intervention of the stable patient.19,20 When the anesthesiologist is integrated into the perioperative care team as a colleague and is comfortable with the preoperative medical consultation provided, the likelihood of case cancellation is dramatically reduced. In cases where there is a significant risk of cancellation, a preoperative team meeting at attending (consultant) level, with the surgeon, medical specialist, and anesthesiologist to discuss the case in a face-to-face manner often avoids case cancellation.
Operating room time availability is a limiting factor at many institutions. There are many and varied surgical cases that compete for emergent or urgent operating room time. An organized program benefits greatly from the availability of designated block time for treatment of geriatric fractures. Such block time allows for earlier surgical intervention and reduced length of stay for older adults with a fracture, to the overall benefit of both the patient and the hospital. Surgical block time also allows for frail, elderly patients to return to their hospital unit when the availability of staff and family is not the lowest of the day. To make this worthwhile for the surgeon and the hospital, it is necessary for the surgeon to be available to use this block time when they are on call. Obviously a satisfactory case volume would be needed to make this useful for the hospital.
Many respondents identified difficulty with cardiac clearance for surgery as an important barrier to implementing a fracture program or improving fracture care at their institution. When instituting a geriatric fracture program, it is important to determine thresholds for requiring cardiac consultation in the preoperative setting,19 and thus adherence to national guidelines such as the American College of Cardiology/ American Hospital Association (ACC/AHA) perioperative guidelines is important to build into an organized program.21 The geriatrician or medical consultant must be comfortable providing preoperative medical consultation in a manner that minimizes the need for preoperative cardiology consultations.19,20 The comfort with preoperative consultations comes with experience in providing the consultations and thus helps to avoid delay due to the perceived need for unnecessary preoperative testing such as preoperative echocardiograms.1,22
One notable finding from question 9 was that there were many more hospitalists at the responding physicians' and surgeons' hospitals than geriatricians. There was an average of 2.3 geriatricians on staff at these centers versus 14.4 hospitalists per center. This suggests that most of these centers implementing a geriatric fracture program would need to use hospitalists as the medical specialists and probable medical champions of the program.
Additional investigation is underway to determine whether the hospitalists given additional training and experience with geriatrics leadership can be used as effectively as geriatricians in an organized fracture program.
Data collection is essential when implementing an organized fracture program. Data about quality measures and about costs of care are both important. When implementing such a program, having baseline data available for analysis will enable both physicians and hospital administration to understand the starting point and will enable a program to be data driven as it progresses. Many of the respondents felt that while data were collected at their hospital, there was uncertainty as to what information was actually collected. This situation can be managed by direct discussions with hospital quality management and finance departments who are typically very willing and eager to work with physicians on quality improvement projects. A commercially available database is available for this purpose or a simple “dashboard or scorecard” can be created at each hospital to manage the results of the program. Metrics followed typically include length of stay, time to surgery, in-hospital complications and mortality, 30-day readmission rate, and infection rates following hip prostheses. This is a useful pursuit that permits short- and intermediate-term assessment of the successes of the program.
When specifically considering what factors would be most helpful to physicians when implementing a geriatric fracture program, the number one response was a site visit to another hospital with a functioning program to serve as a role model, or mentors for hospitals considering implementation of a program. Finding representative hospitals and motivating them to mentor other hospitals remains a challenge. Nearly a quarter of respondents believed that receiving a disk containing the necessary protocols and techniques for implementation of a geriatric fracture program would be most important. Protocols only represent a small portion of the needed effort to implement a fully functional and integrated geriatric fracture program. The authors also acknowledge that use of protocols alone does offer some improvement and advantage to most hospitals simply by standardizing the type of care given and eliminating inappropriate or bad medication usage. The authors believe that there is a need for direct coaching either by colleagues or by consultants on best techniques for implementation of a geriatric fracture program. This avoids the need for each center to reinvent the process to implement a program rather than learning from experience of others who have already done this with success.
A summary of the main barriers as discussed and suggested countermeasures to the identified barriers is provided in Table 2.
Table 2.
Barriers and Countermeasures Suggested by the Authors
| Barrier | Suggested countermeasure |
|---|---|
| Physician leadership | Selection of consensus building leaders3 |
| Need for case manager | Selection of experienced nurse or mid-level provider from the hospital is a good option |
| Anesthesia department support | Need for team building and use of standard accepted guidelines for preoperative consultation19 |
| Operating room time availability | Needs for block time for geriatric fracture cases to permit early surgery20 |
| Administrative support | Best managed with education about the benefits of a program1-4 |
| Difficulty with cardiac clearance | Adherence to national guidelines21 and use of standard medical consultation forms |
| Lack of data | Direct discussions with hospital quality management and finance departments to establish data available and plan for future collection. Administrative support required4 |
Limitations of This Study
The study has many limitations. These include the use of a small sample size of physicians and surgeons responding to this survey. Because no registry of organized geriatric fracture programs exists, it is impossible to truly know how many programs are functioning in the United States today that provide an organized manner of hip fracture care. It is estimated by the authors, based on correspondence and discussion at meetings, that approximately 100 or so programs are fully implemented in the United States today and perhaps another 200 institutions are considering implementing such a program. The survey had 68 respondents. We suspect that we have captured from our responses some of the known programs running in the United States today. This however is a very small sample size, so the reader must evaluate data obtained from it cautiously.
Another limitation is the sampling bias toward level I and level II trauma hospitals. This bias has occurred by selection of the surgeons invited to respond to the survey and by those surgeons and physicians who elected to reply. Level I trauma centers are more likely to be academic medical centers, and it is possible that the academic physicians are more motivated and likely to respond to an academic survey such as this. It is suspected that this bias toward level I and level II trauma centers does not fully represent barriers that may be encountered in level III hospitals. Additional study of such hospitals would be required to obtain meaningful information, yet we suspect that the barriers would be relatively similar at different types of hospitals.
Finally a limitation of this article is the lack of conclusive proof that organized fracture programs will reliably provide better care when implemented at different types of hospitals in different geographic locations.6 Published reports to date have described successful outcomes at isolated academic centers,1,16 yet we recognize that there are no randomized controlled trials or large multicenter trials to confirm the efficacy of this model of care.6 The authors do believe based on their personal experiences and multiple published reports that an organized system of hip fracture care is optimal for the patient and the hospital. This however remains to be shown with larger multicenter trials or randomized controlled trials.
Additional studies are needed to resolve many of these limitations.
Conclusion
A survey was conducted of physicians and surgeons in the United States, regarding barriers to implementing an organized geriatric fracture program. The most concerning/significant barriers described include those of lack of appropriate leadership, team building with colleagues, costs of implementation, the need for coaching and role modeling and difficulties with competing interests among colleagues and with hospital administration. Many techniques are proposed to overcome some of these barriers to implementation of an organized geriatric fracture program, for example appointing “champion leaders.” Additional study on the subject will be useful and will only be possible as more programs are established to permit appropriate study of such programs.
Footnotes
Declaration of Conflicting Interests: The authors' institution receives research support form Synthes, USA not related to this manuscript.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Friedman SM, Mendelson DA, Kates SL, McCann RM. Geriatric co-management of proximal femur fractures: total quality management and protocol-driven care result in better outcomes for a frail patient population. J Am Geriatr Soc. 2008;56(7):1349–1356 [DOI] [PubMed] [Google Scholar]
- 2. Friedman SM, Mendelson DA, Bingham KW, Kates SL. Impact of a comanaged Geriatric Fracture Center on short-term hip fracture outcomes. Arch Intern Med. 2009;169(18):1712–1717 [DOI] [PubMed] [Google Scholar]
- 3. Kates SL, Mendelson DA, Friedman SM. Co-managed care for fragility hip fractures (Rochester model). Osteoporos Int. 2010;21(suppl 4):S621–625 [DOI] [PubMed] [Google Scholar]
- 4. Kates SL, Mendelson DA, Friedman SM. The value of an organized fracture program for the elderly: early results. J Orthop Trauma. 2011;25(4):233–237 [DOI] [PubMed] [Google Scholar]
- 5. Kates SL, Blake D, Bingham K, Kates O, Mendelson DM, Friedman SM. Comparison of an Organized Geriatric Fracture Program to United States Government Data. Geriatr Orthop Surg Rehabil.2010;1(1):15–21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Giusti A, Barone A, Razzano M, Pizzonia M, Pioli G. Optimal setting and care organization in the management of older adults with hip fracture. Eur J Phys Rehabil Med. 2011;47(2):281–296 [PubMed] [Google Scholar]
- 7. Cummings SR, Rubin SM, Black D. The future of hip fractures in the United States. Numbers, costs, and potential effects of postmenopausal estrogen. Clin Orthop Relat Res. 1990(252):163–166 [PubMed] [Google Scholar]
- 8. Kates SL, Kates OS, Mendelson DA. Advances in the medical management of osteoporosis. Injury. 2007;38(suppl 3):S17–S23 [DOI] [PubMed] [Google Scholar]
- 9. Morris AH, Zuckerman JD. National Consensus Conference on Improving the Continuum of Care for Patients with Hip Fracture. J Bone Joint Surg Am. 2002;84-A(4):670–674 [DOI] [PubMed] [Google Scholar]
- 10. Youm T, Koval KJ, Zuckerman JD. The economic impact of geriatric hip fractures. Am J Orthop. 1999;28(7):423–428 [PubMed] [Google Scholar]
- 11. Braithwaite RS, Col NF, Wong JB. Estimating hip fracture morbidity, mortality and costs. J Am Geriatr Soc. 2003;51(3):364–370 [DOI] [PubMed] [Google Scholar]
- 12. Khasraghi FA, Lee EJ, Christmas C, Wenz JF. The economic impact of medical complications in geriatric patients with hip fracture. Orthopedics. 2003;26(1):49–53; discussion 53 [DOI] [PubMed] [Google Scholar]
- 13. Titler M, Dochterman J, Kim T, et al. Cost of care for seniors hospitalized for hip fracture and related procedures. Nurs Outlook. 2007;55(1):5–14 [DOI] [PubMed] [Google Scholar]
- 14. Johnell O. The socioeconomic burden of fractures: today and in the 21st century. Am J Med. 1997;103(2A):20S–25S; discussion 25S-26S [DOI] [PubMed] [Google Scholar]
- 15. Schnell SFS, Mendelson DA, Bingham KW, Kates SL. The 1-year mortality of patients treated in a hip fracture program for elders. Geriatr Orthop Surg. 2010;1(1):6–14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Batsis JA, Phy MP, Melton LJ, 3rd, et al. Effects of a hospitalist care model on mortality of elderly patients with hip fractures. J Hosp Med. 2007;2(4):219–225 [DOI] [PubMed] [Google Scholar]
- 17. Kempe H, Kates SA, Kempe M. Nanomedicine’s promising therapy: magnetic drug targeting. Expert Rev Med Devices. 2011;8(3):291–294 [DOI] [PubMed] [Google Scholar]
- 18. Zuckerman JD, Sakales SR, Fabian DR, Frankel VH. Hip fractures in geriatric patients. Results of an interdisciplinary hospital care program. Clin Orthop Relat Res. 1992(274):213–225 [PubMed] [Google Scholar]
- 19. Marsland D, Colvin PL, Mears SC, Kates SL. How to optimize patients for geriatric fracture surgery. Osteoporos Int. 2010;21(suppl 4):S535–S546 [DOI] [PubMed] [Google Scholar]
- 20. Leung F, Lau TW, Kwan K, Chow SP, Kung AW. Does timing of surgery matter in fragility hip fractures? Osteoporos Int. 2010;21(suppl 4):S529–S534 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Fleisher LA, Beckman JA, Brown KA, et al. ACC/AHA 2007 guidelines on perioperative cardiovascular evaluation and care for noncardiac surgery: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 2002 Guidelines on Perioperative Cardiovascular Evaluation for Noncardiac Surgery). Anesth Analg. 2008;106(3):685–712 [DOI] [PubMed] [Google Scholar]
- 22. Heireamhoin SO, Beyer T, Ahmed M, Mulhall KJ. The role of preoperative cardiac investigation in emergency hip surgery. J Trauma. 2011;71(5):1345–1347 [DOI] [PubMed] [Google Scholar]