Summary
This report describes a rare occurrence of spontaneous closure of direct bilateral carotid cavernous fistula in a 62-year-old woman who had head injury.
This was confirmed by clinical examination and subsequent angiogram. Partial thrombosis of bilateral superior ophthalmic veins was observed in the initial arteriography.
This finding may be useful in prediction of spontaneous cure of carotid cavernous fistulas.
Key words: bilateral carotid cavernous fistula, spontaneous occlusion
Introduction
A post traumatic carotid cavernous fistula (CCF) is direct communication between the internal carotid artery and the cavernous sinus which is usually high flow and most often develop as a consequence of head trauma1-7. Particularly in Thailand, it almost always results from a motor vehicle accident1.
The symptoms depend on venous drainage patterns whose classical ocular presentation involves pulsatile exophthalmos, bruit, chemosis and visual disturbances1,2,3,8.
In recent years, transarterial embolization by detachable balloons has proved the best option for initial treatment of a direct CCF1-3,7-9.
However, the rare occurrence of spontaneous fistula closure has been reported3,5,6,7,10,11,12. This case report illustrates a bilateral post traumatic CCF undergoing spontaneous occlusion simultaneously in spite of no treatment attempt.
Case Report
A 62-year-old woman was referred to our hospital because of head injury. She was knock down by a motorcycle while walking. On admission she was unconscious and had left hemiparesis with a Glasgow Coma Scale score of 7.
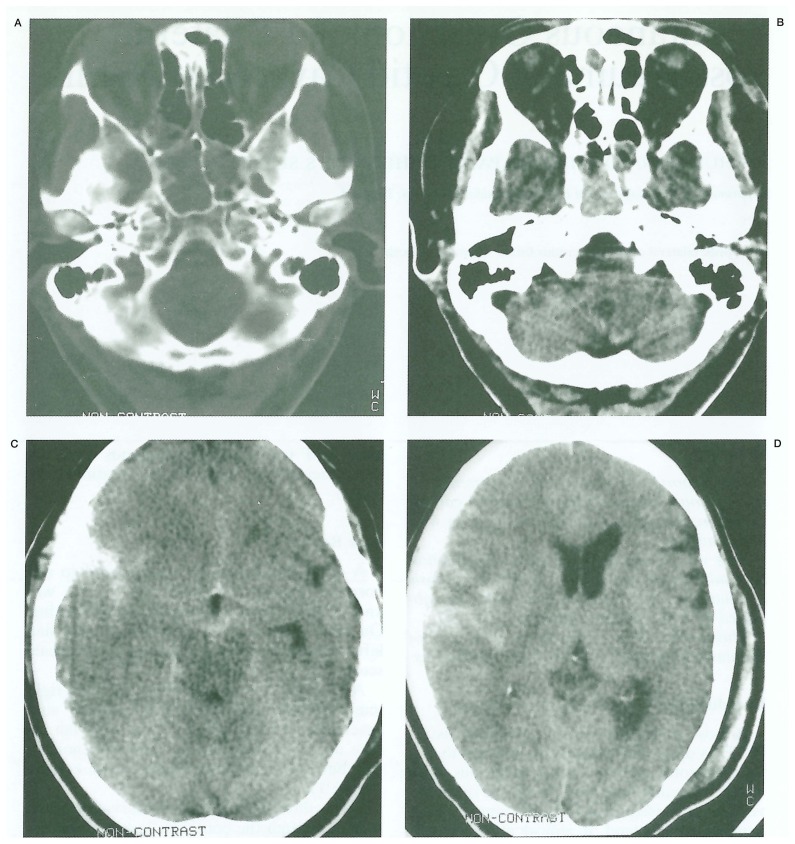
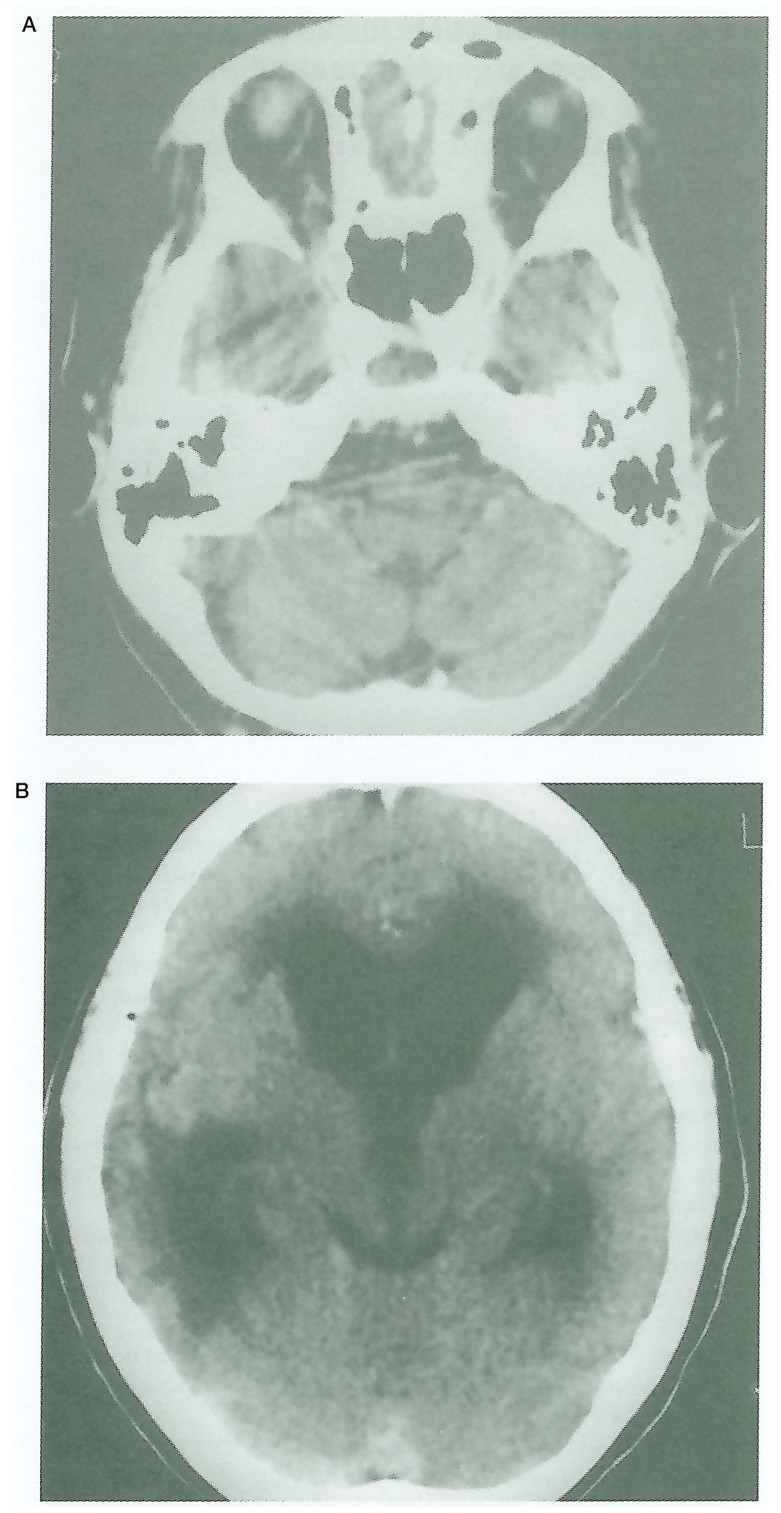
A cranial CT at this time revealed right temporal lobe contusion with profuse subarachnoid hemorrhage in the right sylvian fissure, as well as hemorrhage in the sphenoid sinus but no skull base fracture was evident (figure 1).
Figure 1.
Initial cranial CT scan without contrast study. A,B) Axial scan showing hemorrhage in the sphenoid sinus without demonstrable fracture of the skull base. Also note mild prominent bilateral superior ophthalmic veins. C,D), Axial scan at higher levels reveal subarachnoid hemorrhage in the right sylvian fissure with cortical contusion.
Three days later during conservative treatment, although the conscious level and neurological signs were unchanged, bilateral exophthalmos with chemosis and subconjunctival hemorrhage were observed.
A bruit synchronizing with the pulse was heard on auscultation over bilateral orbital regions.
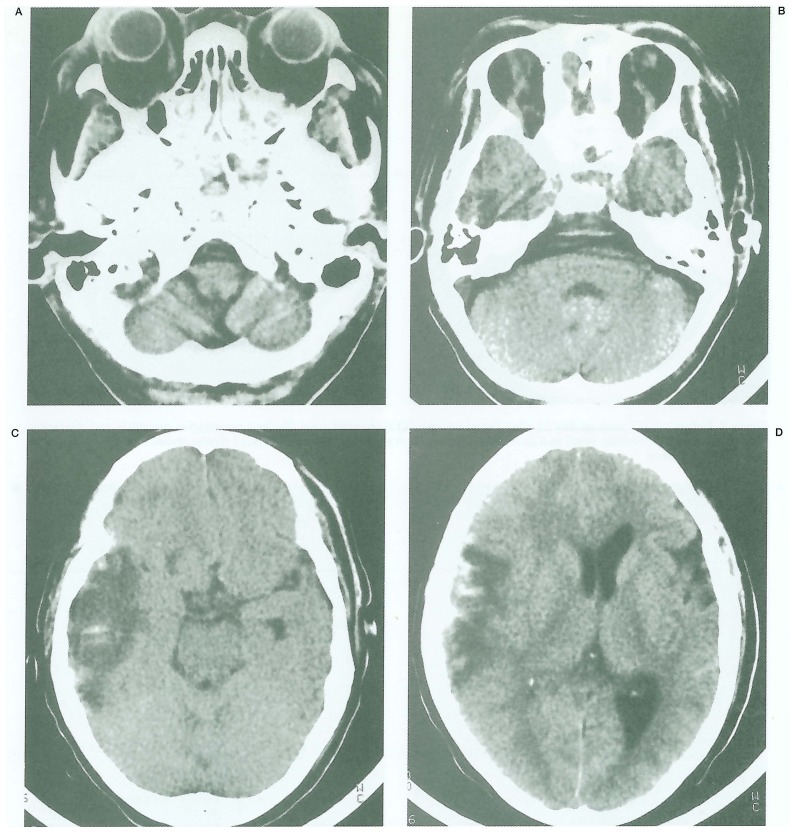
A repeated CT scan of head, on the sixth day of trauma, revealed further dilatation of bilateral superior ophthalmic veins and progressive edema of the right contused temporal lobe (figure 2).
Figure 2.
Follow-up CT scan on day 6 after trauma. A,B) Axial scans at skull base region reveal significant bilateral proptosis and further dilatation of superior ophthalmic veins with enlarged cavernous sinuses C,D) Axial scans at same level as in figure 1C and 1D show progressive of edema of right temporal contusion.
Over the subsequent two weeks, a follow-up CT scan was performed showing bilateral proptosis with persistent dilated ophthalmic veins and significantly enlarged cavernous sinuses (figure 3A).
Figure 3.
Follow-up CT scan on day 21 after initial trauma. A) Enhanced scans disclose progressive proptosis and dilatation of both superior ophthalmic veins and cavernous sinuses. B) Axial scan at level of sylvian fissure shows resolving of hemorrhage and contusion.
The parenchymal injury and subarachnoid hemorrhage had resolved (figure 3B).
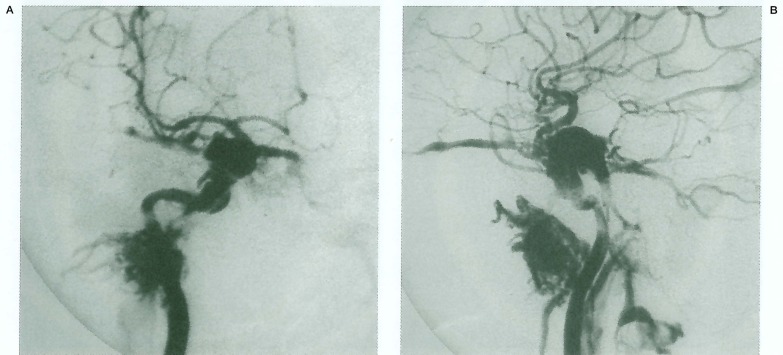
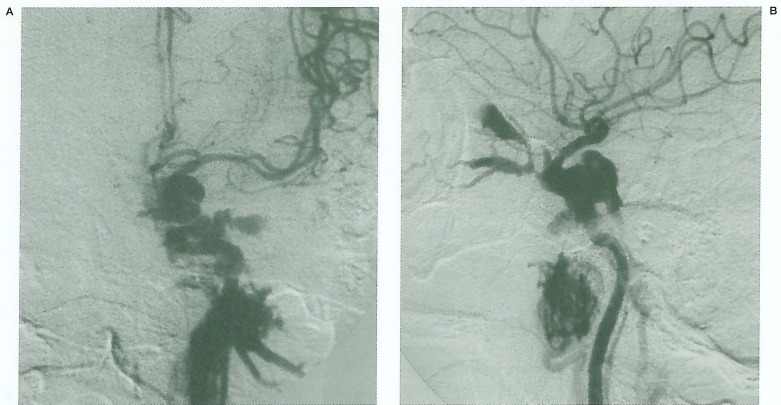
Cerebral angiogram was then requested to confirm the diagnosis of a CCF and for possible embolization. Bilateral CCFs were then disclosed (figure 4, 5).
Figure 4.
Right internal carotid angiography. A) Frontal and B) lateral projections demonstrate a high flow CCF with venous drainage into the superior ophthalmic vein, superior and inferior petrosal sinuses and pterygoid sinus with minimal pial reflux. Note partial thrombosis of the ophthalmic vein and good filling of the supraclinoid ICA and its branches.
Figure 5.
Left internal carotid angiography. A) Frontal and B) lateral projection reveal left CCF with evidence of superior ophthalmic vein thrombosis. No steal phenomenon is demonstrated.
The venous drainage of the right CCF was into superior ophthalmic vein, pterygoid plexus, superior and inferior petrosal sinuses with minimal pial reflux, whereas that of the left one was through ophthalmic veins, pterygoid plexus and inferior petrosal sinus. No steal phenomenon was demonstrated.
Partial thrombosis of bilateral ophthalmic veins was also noted. Because of bilateral CCFs and her associated neurological lesions, the risk of detachable balloon treatment in acute phase and risk of possible sacrifice on one side of the parent artery were weighed against the risk of complications of CCF itself. So, a decision regarding immediate treatment of the CCF was deferred. An elective endovascular treatment was planned in the following month.
Surprisingly, both ocular symptoms gradually improved over two weeks following initial an-giogram, which was more rapid in the left eye.
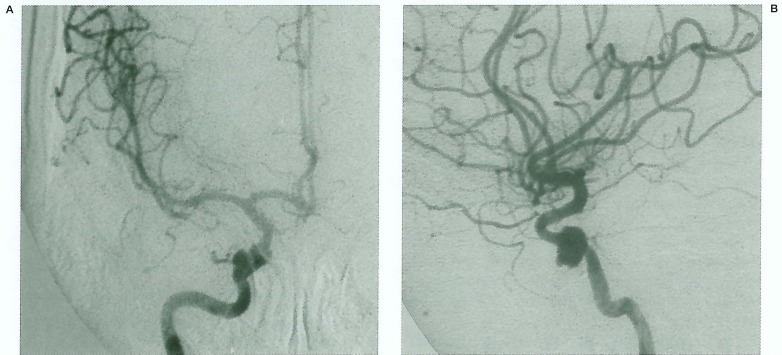
A follow-up angiogram six weeks later exhibited complete closure of the CCFs leaving a residual venous pouch on each side, symmetrically (figure 6, 7).
Figure 6.
Follow-up right internal carotid angiogram in the subsequent 6 weeks. A) Frontal and B) lateral views reveal complete occlusion of the right CCF with leaving a small venous pouch, otherwise is normal.
Figure 7.
Follow-up left internal carotid injection, same setting as in figure 6. A) Frontal and B) lateral projections reveal symmetrical closure of the left CCF and residual venous pouch as in the right side (compared to figure 6).
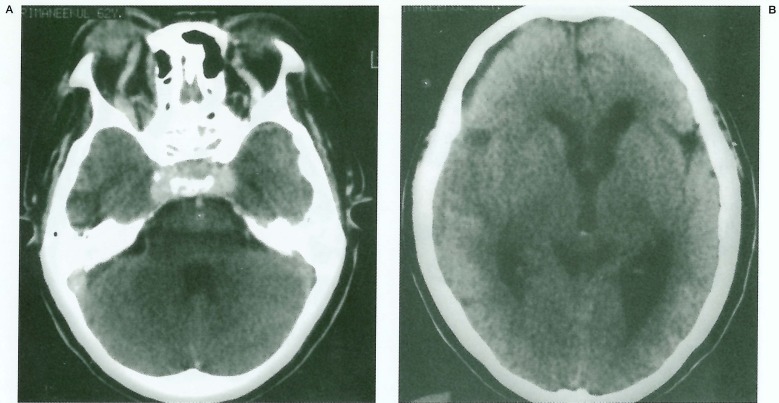
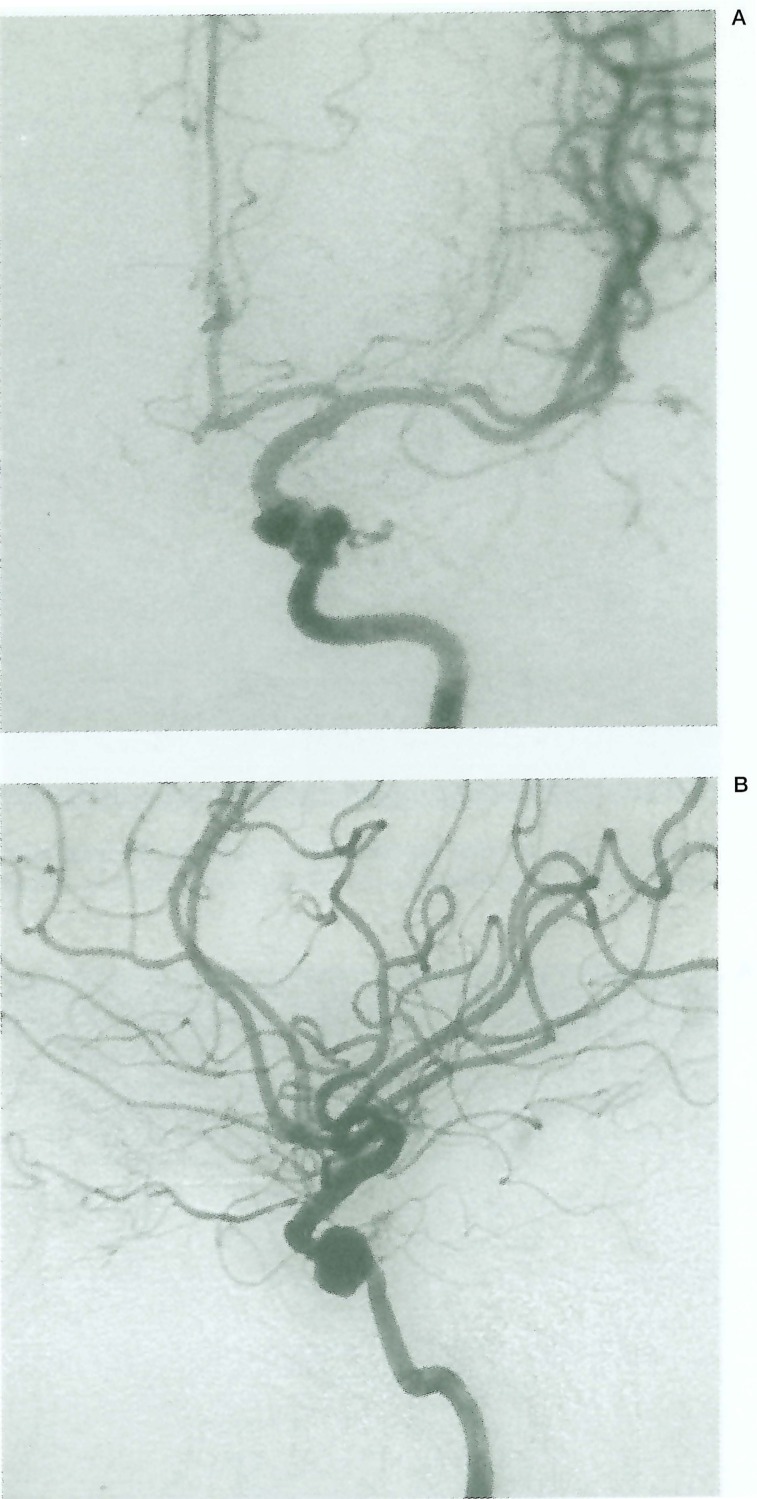
At this time she was somnolent and not respond to verbal commands. However, the proptosis, chemosis and audible bruit disappeared. Because her consciousness was not regained, a follow-up CT scan was again obtained. It revealed no dilatation of the superior ophthalmic veins as expected but progressive communicating hydrocephalus (figure 8).
Figure 8.
Cranial CT scan performed on the day after the second angiogram. A) Axial scan at base skull region shows disappearance of dilated superior ophthalmic veins. B) Contrast image exhibits progressive communicating hydrocephalus significantly as compared to the initial study.
Therefore, a subsequent ventriculoperitoneal shunting was performed. The patient was discharged on the 104th day of admission with residual neurological deficits but no subsequent recurrence of ocular symptoms.
Discussion
A post traumatic CCF occurs secondary to laceration of the internal carotid siphon or from rupture of its intracavernous branches, with or without skull base fracture2.
There are many explanations of the etiologic mechanism responsible for traumatic CCF.
It may be due to the effect of the shear force, penetrating injury by bony spike or sudden critical increase in the intraluminal pressure of the internal carotid artery2,3,4,8.
Bilateral traumatic CCF has been found in approximately 1-2% of patients with CCF3,13.
The aim of treatment of the CCF is complete occlusion of the fistula while maintaining patency of the parent artery.
Therefore, the challenge is greater in management of a bilateral CCF. Currently, the initial treatment of choice is transarterial detachable balloon embolization2,3,7,8,9,14.
Most cases are embolized on an elective basis, but an urgent treatment is needed in those high risk patients who have progressive visual loss, epistaxis, sphenoid sinus aneurysm, cavernous sinus varix or increase intracranial pressure2,5.
Spontaneous closure of a symptomatic post traumatic CCF is quite rare because the shunt has a high rate of blood flow2,3,5,7. This event is far more common in an indirect CCF or dural type2,3,15,16,17.
There have been a few reports in the literature regarding the spontaneous healing of direct CCF3,10,11,12,18,19. Seeger et al reported nine cases of spontaneously thrombosed CCF, but only two of them were direct type18.
Nishijima et al summarized six cases of spontaneous occlusion of traumatic CCF, one of them after orbital venography11.
Castillo et al reported a spontaneous thrombosis which was confirmed by Gd-DTPA enhanced MR12.
Tomsick mentioned of his four symptomatic traumatic CCFs without any attempt at treatment and another three closures following unsuccessful attempts at balloon occlusion, a phenomenon also reported by Berthelsen and Wilm3.
Spontaneous occlusion of bilateral CCF, to our knowledge, was reported in only one caseby Voigt et al in 197110, however, this case was a spontaneous dural CCF type B according to Barrow classification15.
In our case, bilateral CCF was disclosed clinically in a few days following head trauma.
Despite no recommendation in the literature regarding the proper timing for endovascular treatment of the acute CCF, we are reluctant to perform balloon embolization in such instance.
In our opinion, it may be a risk if we distend cavernous sinus by balloon in the acute stage of injury.
We usually delay definite therapy for at least six weeks after initial trauma, if there is no indication for emergency treatment.
Meanwhile, observation for the progressive eye symptoms and monitoring intraocular pressure are suggested.
Fortunately, this case had spontaneous healing in this period which was proved by serial angiography.
The mechanism of spontaneous cure is uncertain.
Various postulations have been advanced in the literature.
An explanation is suggested from the effect of iodinated contrast media which exaggerates leukocytic accumulation, promotes RBC aggregation and has a direct effect on the vascular endothelium leading to thrombosis 11,12.
Another possibility is that spontaneous thrombosis may be provoked by venostasis following alteration in the presssure gradient during angiography or due to decrease in blood flow passing through the fistula secondary to hypotension during anesthesia10,11,12.
This phenomenon is, however, usually reported with spontaneous dural CCF rather than direct high flow type3,10,15,16,20.
Considering the mechanism of spontaneous closure in our case, there are two interesting situations; the patient had an accompanied increase in intracranial pressure caused by primary brain injury and had evidence of thrombosis of the bilateral ophthalmic veins.
We speculate that an increased intracranial pressure may cause venostasis in the cavernous sinus, subsequently leading to ophthalmic vein thrombosis and inducing spontaneous closure of the fistula.
This can happen simultaneously in bilateral lesions.
Conclusion
This case illustrates a very rare occurrence of spontaneous regression of bilateral high flow traumatic CCF.
It is important to demonstrate and analyzecarefully the angioarchitecture of the lesion before therapeutic planning regarding the timing and method of treatment.
Evidence of thrombosis of the ophthalmic veins may be a predictive sign of spontaneous closure. In such instance, with no indications for urgency treatment, patients should be managed conservatively before the decision to institute any aggressive forms of treatment.
References
- 1.Suthiponchai S, Pongpech S, et al. Interventional neuroradiology in Thailand: 1989-1997. Interventional Neuroradiology. 1997;3:185–198. doi: 10.1177/159101999700300301. [DOI] [PubMed] [Google Scholar]
- 2.Lasjaunias P, Berenstein A. In: Surgical Neuro-angiography: Endovascular treatment of craniofacial lesions. Vol. 2. Berlin: Springer-Verlag; 1987. Arteriovenous fistulas; pp. 175–211. [Google Scholar]
- 3.Tomsick TA. Carotid Cavernous Fistula. Digital educational publishing, INC; 1997. TypeA (direct) CCF: etiology, prevalence, and natural history; pp. 33–58. [Google Scholar]
- 4.Helmke K, Kruger O, Lass R. The direct carotid cavernous fistula: a clinical, pathoanatomical, and physical study. Acta Neurochir. 1994;127:1–5. doi: 10.1007/BF01808537. [DOI] [PubMed] [Google Scholar]
- 5.Halbach V, Hieshima G, et al. Carotid cavernous fistulae: indications for urgent treatment. Am J Radiol. 1987;149:587–593. doi: 10.2214/ajr.149.3.587. [DOI] [PubMed] [Google Scholar]
- 6.Graves V, Strother C, et al. Giant intracavernous carotid aneurysm after spontaneous thrombosis of a carotid cavernous sinus fistula. Am J Neuroradiol. 1988;9:595–597. [PMC free article] [PubMed] [Google Scholar]
- 7.Carter LP, Spetzler RF, Hamilton MG. Neurovascular surgery. McGraw-Hill, INC; 1995. Carotid-cavernous fistulae: Part 1: presentation and features; pp. 1056–1057. [Google Scholar]
- 8.Fabian TS, Woody JD, et al. Posttraumatic carotid cavernous fistula: frequency analysis of signs, symptoms, and disability outcomes after angiographic embolization. Journal of Trauma-Injury Infection and Critical Care. 1999;47(2):275–281. doi: 10.1097/00005373-199908000-00009. [DOI] [PubMed] [Google Scholar]
- 9.Lewis Al, Tomsick TA, et al. Long-term results in direct carotid-cavernous fistulas after treatment with detachable balloons. J Neurosurg. 1996;84:400–404. doi: 10.3171/jns.1996.84.3.0400. [DOI] [PubMed] [Google Scholar]
- 10.Voigt K, Sauer M, Dichgans J. Spontaneous occlusion of a bilateral caroticocavernous fistula studied by serial angiography. Neuroradiology. 1971;2:207–211. doi: 10.1007/BF00337568. [DOI] [PubMed] [Google Scholar]
- 11.Nishijima M, Iwai R, et al. Spontaneous occlusion of traumatic carotid cavernous fistula after orbital venography. Surg Neurol. 1985;23:489–492. doi: 10.1016/0090-3019(85)90244-7. [DOI] [PubMed] [Google Scholar]
- 12.Castillo M, Silverstein M, et al. Spontaneous thrombosis of a direct carotid cavernous sinus fistula: confirmation by Gd-DTPA-enhanced MR. Am J Neuroradiol. 1989;10:S75–S76. [PMC free article] [PubMed] [Google Scholar]
- 13.Lewia Al, Tomsick TA, Tew JM. Management of 100 consecutive carotid-cavernous fistulas: results of treatment using detachable balloons. Neurosurgery. 1995;36:239–244. doi: 10.1227/00006123-199502000-00001. [DOI] [PubMed] [Google Scholar]
- 14.Mullan S. Carotid-cavernous fistulas and intracavernous aneurysms. In: Wilkins R, Rengachary SS, editors. Neurosurgery. St Louis: Mcgraw-Hill; 1988. p. 1488. [Google Scholar]
- 15.Barrow DL, Spxector RH, et al. Classification and treatment of spontaneous carotid-cavernous sinus fistulas. J Neurosurg. 1985;62:248–256. doi: 10.3171/jns.1985.62.2.0248. [DOI] [PubMed] [Google Scholar]
- 16.Sasaki H, Nukui H, et al. Long-term observations in cases with spontaneous carotid-cavernous fistulas. Acta Neurochir. 1988;90:117–120. doi: 10.1007/BF01560564. [DOI] [PubMed] [Google Scholar]
- 17.Komiyama M, Nakajima H, et al. Traumatic carotid cavernous sinus fistula: serial angiographic studies from the day of trauma. Am J Neuroradiol. 1998;19:1641–1644. [PMC free article] [PubMed] [Google Scholar]
- 18.Seeger JF, Gabrielsen TO, et al. Carotid cavernous sinus fistulae and venous thrombosis. Am J Neuroradiol. 1980;1:141–148. [PMC free article] [PubMed] [Google Scholar]
- 19.Calon B, Freys G, et al. Early discovery of a traumatic carotid-cavernous sinus fistula by jugular venous oxygen saturation monitoring. J Neurosurg. 1995;83:910–911. doi: 10.3171/jns.1995.83.5.0910. [DOI] [PubMed] [Google Scholar]
- 20.Yamamoto T, Asai K, et al. Spontaneous resolution of symptoms in an infant with a congenital dural caroticocavernous fistula. Neuroradiology. 1995;37:247–249. doi: 10.1007/BF01578267. [DOI] [PubMed] [Google Scholar]