Abstract
Introduction:
The Food and Drug Administration is in the process of reviewing evidence of the impact of mentholated cigarettes on smoking behaviors and smoking cessation in order to determine if these products should be removed from the market. More empirical research is needed to inform those decisions. The goal of this study was to examine associations of menthol cigarette use with biochemically verified continuous short-term smoking abstinence, and potential moderation by race, among adult current smokers enrolled in a cohort study (N = 183; 57.4% female; 48.1% non-Hispanic Black, 51.9% non-Hispanic White).
Methods:
Continuation ratio logit models, adjusted for age, race, gender, total annual household income, educational level, employment status, and partner status, were used to examine associations of menthol use with smoking abstinence with and without an interaction term for race.
Results:
Menthol cigarette use was not significantly associated with smoking abstinence in the sample as a whole; however, there was a significant interaction of menthol use with race (p = .03). Follow-up analyses stratified by race indicated that among White participants, menthol users had significantly lower odds of maintaining continuous abstinence than nonmenthol users (p = .05). Exploratory analyses suggested that tobacco dependence may lie along the causal pathway and partially explain this effect.
Conclusions:
White menthol smokers in this sample were at increased risk of smoking relapse relative to White nonmenthol smokers, at least partially due to greater tobacco dependence. Results should be replicated among other treatment-seeking samples with a greater representation of White menthol and Black nonmenthol smokers.
INTRODUCTION
Menthol cigarettes are heavily marketed to racial/ethnic minority groups (Anderson, 2011; Gardiner, 2004; Sutton & Robinson, 2004; Yerger, Przewoznik, & Malone, 2007), and are used at higher rates among racial/ethnic minority smokers relative to non-Hispanic White smokers (Gardiner, 2004; Giovino et al., 2004; Gundersen, Delnevo, & Wackowski, 2009; Kabat, Morabia, & Wynder, 1991; Lawrence et al., 2010). It has been suspected that the higher prevalence of menthol cigarette use among racial/ethnic minority smokers may be a contributor to smoking-related health disparities, as the presence of menthol in cigarettes may make smoking more attractive, easier to tolerate, or more reinforcing (Ahijevych & Garrett, 2004, 2010; Clark, Gardiner, Djordjevic, Leischow, & Robinson, 2004; Okuyemi et al., 2003; Williams et al., 2007). However, results of both treatment-oriented and population-based studies investigating relations of menthol use status and smoking cessation have been mixed, with some studies supporting relations between menthol use and lower cessation rates (Delnevo, Gundersen, Hrywna, Echeverria, & Steinberg, 2011; Levy et al., 2011; Okuyemi et al., 2003; Okuyemi, Faseru, Sanderson Cox, Bronars, & Ahluwalia, 2007; Trinidad, Perez-Stable, Messer, White, & Pierce, 2010) and others citing null results (Alexander, Crawford, & Mendiondo, 2010; Fu et al., 2008; Hyland, Garten, Giovino, & Cummings, 2002; Muscat, Richie, & Stellman, 2002; Pletcher et al., 2006). Given the conflicting results in the literature, additional research on the relation of menthol use status and cessation are needed. Such research is particularly timely, given that menthol has been excluded from a ban on cigarette flavorings pursuant to the Family Smoking Prevention Tobacco Control Act pending additional research.
Although the literature on the relation between menthol use and cessation is mixed overall, several studies suggest the importance of examining the moderating role of race in these relations. Most of these studies support a significant disadvantage among Black or other racial/ethnic minority menthol users with regard to smoking cessation (see Foulds, Hooper, Pletcher, & Okuyemi, 2010 for a review). For example, at least four recent studies have found that Black, Hispanic, and/or Black and Hispanic menthol users are less likely to have successfully quit smoking as compared with their nonmenthol using counterparts (Delnevo et al., 2011; Gandhi, Foulds, Steinberg, Lu, & Williams, 2009; Gundersen et al., 2009; Stahre, Okuyemi, Joseph, & Fu, 2010). However, at least two studies have supported that even non-Hispanic White menthol users are at a disadvantage relative to non-Hispanic White nonmenthol users when it comes to quitting smoking (Delnevo et al., 2011) or avoiding smoking relapse after a period of abstinence (in this case, among a postpartum sample; Reitzel et al., 2011). Moreover, one recent study found that White menthol users were less likely to even make a quit attempt relative to Black menthol users, as well as relative to White nonmenthol users (Kahende, Malarcher, Teplinskaya, & Asman, 2011). Again, more research is needed to better understand how the relation of menthol use status and cessation might differ by race/ethnicity, as well as the mechanisms that might underlie these differences.
It has been previously speculated that tobacco dependence might account for significant inverse relations between menthol use and smoking cessation, irrespective of the smoker’s racial background. Internal tobacco industry documents, for example, support that the menthol content of cigarettes has been specifically manipulated to facilitate tobacco dependence among long-term smokers (Kreslake, Wayne, Alpert, Koh, & Connolly, 2008). However, empirical results in this area have been mixed, with some studies supporting relations between menthol use and greater dependence (Fagan et al., 2010), and others supporting the opposite pattern (Hyland et al., 2002) or a mixed picture based on how tobacco dependence is conceptualized (Muscat et al., 2009). Smoking behaviors and tobacco dependence, however, are known to differ by race/ethnicity (Foulds et al., 2010; Muscat et al., 2002), and perhaps may also differ by menthol use status within racial/ethnic groups. For example, one previous study found a stronger inverse association of menthol use with heaviness of smoking (in particular) among Black than among White smokers (Muscat et al., 2009). However, no previous studies that we are aware of have examined the potential indirect effects of menthol use status on smoking cessation through tobacco dependence by race.
The purpose of the current study was to examine the associations of menthol use status with biochemically verified short-term smoking abstinence among a treatment-seeking sample of non-Hispanic Black and non-Hispanic White daily smokers, and to examine whether associations were moderated by race, in analyses adjusted for age, gender, income, education, employment status, and partner status. A secondary aim was to identify the potential role of tobacco dependence as a mediator underlying significant relations.
METHODS
Participants and Procedures
Data were collected as part of a longitudinal study examining changes in risk perceptions over time among community smokers attempting to quit smoking. Inclusion criteria were as follows: English-speaking current smokers aged 18–65 who endorse smoking ≥5 cigarettes/day for ≥12 months, willingness to quit smoking within the next week, functioning telephone number and a permanent home address, and sixth grade literacy level. Exclusion criteria were as follows: regular use of tobacco products other than cigarettes, the use of pharmacological smoking cessation treatments at enrollment, reported medical contraindications to the nicotine patch, pregnancy or lactation, other household members enrolled in the study, participation in a smoking cessation program in the last 3 months, or active substance use or dependence (other than tobacco).
Participants in the parent study were 200 smokers from Houston, TX, who were enrolled in 2006–2007; however, due to the inadequate representation of some racial and ethnic groups in the sample, the current study was limited to the non-Hispanic White and non-Hispanic Black participants in the parent project (n = 183). Data were collected during a phone screening for eligibility and five in-person clinic visits. These visits occurred 1 week prior to the participants’ quit date (baseline), on the quit date (week 0), and weeks 1, 2, and 3 following the quit date (week 1, week 2, and week 3). All participants in the parent protocol had access to four brief cessation counseling sessions and 4 weeks of nicotine replacement therapy (the patch), and were compensated for their time and effort with a $25 department store gift card at each in-person clinic visit they attended. The University of Texas MD Anderson Cancer Center Institutional Review Board approved this study. Written informed consent was obtained before data collection.
Measures
Sociodemographics
Sociodemographics collected during the phone screen included age, race, gender, total annual household income, educational level, employment status, and partner status.
Menthol Use Status
Menthol use was assessed during the phone screen by a single item assessing if participant’s usual brand of cigarettes was menthol or nonmenthol. Results yielded a binary predictor variable (nonmenthol vs. menthol; reference group = nonmenthol).
Continuous Short-Term Smoking Abstinence
Smoking status was assessed at postquit weeks 1, 2, and 3. Continuous abstinence from smoking was defined as a self-report of no cigarettes smoked since the quit date (not even a puff) and an expired carbon monoxide level of <10 ppm at each assessment. Relapse at any assessment resulted in classification as relapsed from that point forward. Data were available to determine abstinence status for 90.2% of participants at week 1 and 91.3% of participants at weeks 2 and 3. When data were unavailable for determining abstinence, participants were coded as relapsed.
Tobacco Dependence
Tobacco dependence was assessed using the Heaviness of Smoking Index (HSI), which was calculated from the number of cigarettes smoked per day and the time to the first cigarette of the day (Borland, Yong, O’Connor, Hyland, & Thompson, 2010; Heatherton, Kozlowski, Frecker, Rickert, & Robinson, 1989). Scores on the HSI could range from 0 to 6. The HSI was handled as continuous variable in analyses (see Fagerström, Russ, Yu, Yunis, & Foulds, 2012 for precedent).
Data Analyses
Preliminary analyses explored differences in participant characteristics by menthol use status using chi-square tests for categorical variables and t tests for continuous variables. Main analyses examined the effect of menthol use on short-term smoking abstinence in SAS v. 9.1 (SAS Institute) using continuation ratio (CR) logit models (PROC GENMOD). CR logit modeling is appropriate when ordered categories (i.e., relapsed at week 1, abstinent at week 1 but relapsed at week 2, and abstinent through week 3) represent a progression through “stages” (Agresti, 2002; Bender & Benner, 2000; McGowan, 2000; Singer & Willett, 1993; Willett & Singer, 1993). The CR logit models operate by modeling the conditional probability of being abstinent at the current assessment point given that a participant has been abstinent through the most recent assessment point. Analyses controlled for age, race, gender, total annual household income, educational level, employment status, partner status, and stage. Following this, the interaction of race and menthol use status on smoking abstinence was tested by including the interaction term in the adjusted model. Significant results were further examined in analyses stratified by race.
Following the completion of the main analyses, exploratory analyses were conducted to examine the resiliency of significant findings to two alternative conceptualizations of abstinence: continuous short-term smoking abstinence including “completers-only” and 7-day point prevalence abstinence. Completers-only continuous short-term smoking abstinence was defined the same way as the main abstinence outcome except that missing abstinence data were maintained as missing in the dataset. Seven-day point prevalence abstinence was defined as a self-report of no smoking (not even a puff) during the 7 days prior to the assessment and an expired carbon monoxide level of <10 ppm. Unlike continuous smoking abstinence, 7-day point prevalence abstinence status could vary from week to week (e.g., abstinent during week 1, relapsed during week 2, and abstinent during week 3). CR logit modeling was used to assess outcomes using completers-only continuous short-term smoking abstinence, and generalized linear mixed model regression (SAS PROC GLIMMIX) was used to assess outcomes using 7-day point prevalence abstinence.
Finally, we were interested in the possibility that tobacco dependence (i.e., the HSI) might lie along the causal pathway and at least partially account for any significant relations of menthol use status and smoking abstinence. To address this possibility, we used a nonparametric bootstrapping procedure to estimate the significance of an indirect effect in single mediation models with 5,000 resamples with replacement from the dataset (MacKinnon, 2008). Continuous abstinence was treated as an ordinal variable with one observation (i.e., abstinent through which postquit week) for every participant. Therefore, the bootstrapping was performed by resampling individual ordinal outcomes from the dataset. Because the CR logit model operates through a logistic regression approach for a binary smoking abstinence variable, with observations conditional on being continuously abstinent through each time point (thus, each individual contributes a varied number of binary observations), the corresponding estimates of the coefficients were standardized in calculating the indirect effect and the proportion of total effect that was mediated [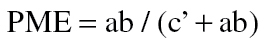 ] (MacKinnon, Lockwood, Brown, Wang, & Hoffman, 2007). These analyses were conducted using R version 2.13.0 (R Core Team, 2012) and were adjusted for age, gender, total annual household income, educational level, employment status, partner status, and stage.
] (MacKinnon, Lockwood, Brown, Wang, & Hoffman, 2007). These analyses were conducted using R version 2.13.0 (R Core Team, 2012) and were adjusted for age, gender, total annual household income, educational level, employment status, partner status, and stage.
RESULTS
Participant Characteristics
Participants (N = 183; 95 non-Hispanic White and 88 non-Hispanic Black smokers) were 45.9 years of age (±10.31) on average. In the overall sample, continuous abstinence rates were 25.7% at week 1, 19.1% at week 2, and 15.9% at week 3. There were fewer menthol than nonmenthol using participants (83 menthol users vs. 100 nonmenthol users). Among menthol users, continuous short-term smoking abstinence rates were 19.3% at week 1, 14.5% at week 2, and 12.1% at week 3. Among nonmenthol users, continuous short-term smoking abstinence rates were 31.0% at week 1, 23.0% at week 2, and 19.0% at week 3. Among White participants, 18.9% (n = 18) endorsed current menthol cigarette use, whereas 73.9% (n = 65) of Black participants endorsed current menthol cigarette use. White menthol smokers had higher HSI scores (4.28±1.53) as compared with Black menthol (3.42±1.27) smokers (t = −2.43, p = .02). Likewise, White menthol smokers had higher HSI scores than White nonmenthol smokers (3.75±1.30), although this difference was not statistically significant (p = .14). Participant characteristics by menthol use status are in Table 1.
Table 1.
Participant Characteristics by Menthol Use Status
| Menthol user | Nonmenthol user | p value | Total sample | |||||
|---|---|---|---|---|---|---|---|---|
| n = 83 | n = 100 | N = 183 | ||||||
| n/Mean | %/SD | n/Mean | %/SD | N/Mean | %/SD | |||
| Age | 45.90 | 10.31 | 46.81 | 9.23 | .5312 | 46.4 | 9.71 | |
| Missing | 0 | 0 | 0 | |||||
| Race | ||||||||
| Non-Hispanic Black | 65 | 78.31 | 23 | 23.00 | <.0001 | 88 | 48.09 | |
| Non-Hispanic White | 18 | 21.69 | 77 | 77.00 | 95 | 51.91 | ||
| Missing | 0 | 0 | 0 | |||||
| Gender | .1064 | |||||||
| Male | 30 | 36.14 | 48 | 48.00 | 78 | 42.62 | ||
| Female | 53 | 63.86 | 52 | 52.00 | 105 | 57.38 | ||
| Missing | 0 | 0 | 0 | |||||
| Annual household income | .1392 | |||||||
| <$20,000 | 42 | 52.50 | 41 | 41.41 | 83 | 46.37 | ||
| ≥$20,000 | 38 | 47.50 | 58 | 58.59 | 96 | 53.63 | ||
| Missing | 3 | 1 | 4 | |||||
| Education | .0672 | |||||||
| ≤High school diploma | 33 | 39.76 | 27 | 27.00 | 60 | 32.79 | ||
| >High school diploma | 50 | 60.24 | 73 | 73.00 | 123 | 67.21 | ||
| Missing | 0 | 0 | 0 | |||||
| Employment status | .0487 | |||||||
| Employed | 36 | 43.37 | 58 | 58 | 94 | 51.37 | ||
| Unemployed | 47 | 56.63 | 42 | 42 | 89 | 48.63 | ||
| Missing | 0 | 0 | 0 | |||||
| Partner status | .1092 | |||||||
| Married/living with partner | 20 | 24.10 | 35 | 35.00 | 55 | 30.05 | ||
| Single/widowed/divorced | 63 | 75.90 | 65 | 65.00 | 128 | 69.95 | ||
| Missing | 0 | 0 | 0 | |||||
| HSI | 3.60 | 1.37 | 3.73 | 1.23 | .5079 | 3.67 | 1.29 | |
| Missing | 0 | 0 | 0 | |||||
Note. t tests or chi-square tests were used to evaluate significant differences between menthol and nonmenthol users. Missing data were maintained in analyses. HSI = Heaviness of Smoking Index; SD = standard deviation.
Preliminary Analyses
Preliminary analyses indicated significant differences between menthol and nonmenthol users by race and employment status. Specifically, most menthol users were Black, whereas most nonmenthol users were White participants. Also, more menthol users were unemployed, whereas more nonmenthol users were employed. Similar findings have been reported previously (Lawrence et al., 2010). See Table 1.
Main Analyses
The main effects of menthol use status on continuous short-term smoking abstinence were not significant (β = −0.31, SE = 0.40; χ2(1) = 0.60; p = .44; n [hereafter, number of observations used in analysis] = 257). An additional model tested the interaction of menthol use and stage. This interaction term was not significant (p = .78), indicating no significant variation of the effect of menthol status on abstinence by data stage. Race, however, was a significant moderator of relations between menthol use status and smoking abstinence (p = .03). Follow-up analyses stratified the sample by race and examined covariate-adjusted relations between menthol use status and smoking abstinence. Menthol use was significantly associated with short-term continuous smoking abstinence among White participants (β = −1.56, SE = 0.79; χ2(1) = 3.96; p = .05; n = 142), but not among Black participants (β = 0.54, SE = 0.55; χ2(1) = 0.95; p = .33; n = 115). The direction of relations was such that White menthol users were about 5 times less likely to maintain continuous smoking abstinence than White nonmenthol users (odds ratio = 0.21, 95% CI = 0.05–0.98).
Exploratory Analyses
Initial exploratory analyses were conducted with two alternative conceptualizations of abstinence: completers-only continuous smoking abstinence and 7-day point prevalence abstinence. For analyses focused on completers-only continuous smoking abstinence, there was a significant interaction of menthol use status and race (p = .03; n = 238). As with the main analyses, follow-up analyses that were stratified by race found a significant association of menthol use with continuous smoking abstinence among White participants (β = −1.60, SE = 0.79; χ2(1) = 4.06; p = .04; n = 132), but not among Black participants (β = 0.50, SE = 0.56; χ2(1) = 0.80; p = .37; n = 106). Likewise, there was a significant interaction of menthol use status and race in analyses predicting 7-day point prevalence abstinence over time (p < .01; n = 537). Racially stratified analyses again supported a significant association of menthol use with point prevalence smoking abstinence through postquit week 3 among White participants (β = −1.90, SE = 0.82; F(1,85) = 5.41; p = .02; n = 279), but not among Black participants (β = 1.00, SE = 0.67; F(1,78) = 2.69; p = .11; n = 258).
The final exploratory analyses examined the indirect effect of menthol use on continuous short-term smoking abstinence through the HSI within the White and Black participant samples separately. Results indicated a significant indirect effect of HSI on the relation between menthol use and smoking abstinence among White (standardized indirect effect = −0.07, bias-corrected 95% bootstrap CI = −0.01 to −0.38, p ≤ .05), but not Black (p > .05), participants. Among the White subsample, menthol use was positively related to dependence, and dependence was inversely related to abstinence. The proportion of the mediated effect among the White subsample was 9.6%.
DISCUSSION
The current study examined the effect of menthol use on biochemically verified, continuous short-term smoking abstinence among a treatment-seeking sample of adult daily smokers from Houston, TX. Results from this well-controlled study failed to support a main effect of menthol use on cessation. These results are similar to a number of previous studies in the field focused on both treatment-seeking and population-based samples of smokers (Alexander et al., 2010; Fu et al., 2008; Hyland et al., 2002; Muscat et al., 2002; Pletcher et al., 2006). However, results indicated a significant racial interaction effect whereby White menthol smokers were about 5 times more likely to relapse than White nonmenthol smokers. This pattern of results was consistent across three different conceptualizations of abstinence (e.g., intent-to-treat continuous smoking abstinence, completers-only continuous smoking abstinence, and 7-day point prevalence abstinence). The significant relationship between menthol use and smoking cessation among White smokers was somewhat unexpected, given that previous studies tend to support significant relations among minority smokers (see Foulds et al., 2010). However, results are consistent with a previous study focused on relapse prevention conducted among treatment-seeking postpartum women, which found that White nonmenthol users had 4 times higher abstinence rates than White menthol users (Reitzel et al., 2011). Results also complement other studies suggesting that White menthol smokers experience more difficulty quitting than White nonmenthol smokers (Delnevo et al., 2011; Kahende et al., 2011). The lack of effects of menthol use on cessation among the Black smokers in the sample may reflect unique sample characteristics, as this study was comprised treatment-seeking smokers who were willing to participate in a clinical trial. As minority participation in clinical trials is generally low, the participants in this study may not be representative of the larger Black population of smokers in some important way. Likewise, the other study finding a similar pattern of results (e.g., menthol effects for Whites but not Blacks; Reitzel et al., 2011) was also a clinical trial. Nevertheless, it is important to examine the effects of menthol use on cessation in various populations and settings to fully understand extant relations, although ideally such studies should be designed with this purpose in mind.
A potentially important finding in the present study was that greater tobacco dependence, as indicated by higher scores on the HSI, partially accounted for the effects of menthol use on reduced odds of smoking cessation among White smokers in this sample. Tobacco dependence is most commonly treated as a covariate in analyses predicting smoking cessation due to its known relations with quitting behaviors (Borland et al., 2010). It was not included as a covariate in the current study, however, due to its conceptualization as a potential mediator of relations. Although the proportion of the total effect accounted for by the HSI was relatively small (9.6%), results suggest that tobacco dependence might lie along the causal pathway between menthol use and smoking cessation, at least among White smokers. This is important because few, if any, previous studies in this area have formally examined variables that might mediate relations between menthol use and smoking cessation. These results, however, are considered preliminary in nature and should be interpreted with caution given the limited number of White menthol users in this sample. Additional research in this area will help to clarify if tobacco dependence is truly a mechanism underlying the effects of menthol use on cessation, or if it is best conceptualized as a confounding variable. It is worth noting that, in this study, additionally controlling for the HSI in our main and exploratory (nonmediation focused) analyses did not change the pattern of results.
Understanding more about the mechanisms that underlie relations between menthol use and reduced odds of cessation can help to inform interventions. In this case, results suggest that White menthol smokers may benefit from additional or more intense cessation interventions than the standard cessation intervention made available in the parent study, and that a particular focus on coping with smoking urges may be indicated. Additionally, these results suggest that future studies in this area might examine whether tobacco dependence is a mediator of associations between menthol use and cessation within racial subgroups, in order to clarify if and how these relations might differ by race. Likewise, a focus on other mechanisms that account for relations between menthol use and cessation is needed, and should be a goal of future studies in this area.
The Food and Drug Administration is in the process of reviewing evidence of the impact of mentholated cigarettes on smoking behaviors and smoking cessation in order to determine if these products should be removed from the market. Empirical findings suggesting that certain racial groups may be more likely to smoke mentholated cigarettes and/or less likely to quit smoking bring issues of social justice to bear on the Food and Drug Administration’s deliberation (Gardiner & Clark, 2010; Healton et al., 2010). Results of the present study add to a growing body of empirical literature that supports associations between menthol cigarette use and smoking relapse among a particular group of smokers (in this case, non-Hispanic White smokers), and suggest the potential utility of removing menthol flavorings from the market to facilitate smoking cessation. However, given the small proportion of White menthol smokers (22%) and Black nonmenthol smokers (23%) in this study, it is also important to acknowledge that these results should be replicated among other treatment-seeking samples with greater representation of smokers in these categories. Because the current study represented a secondary data analysis of existing data, it was necessarily restricted in this regard.
Limitations of the current study include that it was focused on a select group of treatment-seeking smokers from a large metropolitan area in the southwest. Therefore, results may not generalize to nontreatment-seeking smokers, smokers from rural areas, or smokers from other areas of the country, inasmuch as these smokers may differ from the ones included in this study. Nontreatment-seeking smokers (self-quitters), for example, may be less dependent on tobacco than treatment-seeking smokers, and so forth. It is important to examine relations between menthol use and cessation among self-quitters, as well as among smokers of different racial/ethnic groups, in order to better understand the broader impact of menthol use on smoking and quitting behaviors. In addition, although we adjusted analyses for many covariates that were known to potentially affect the relations of interest, it is possible that some relevant covariates were omitted. For example, information on compliance with the nicotine replacement therapy provided in this study was not collected and could not be included in analyses. Another limitation of the current study was the limited focus on short-term smoking abstinence. The results of the current study may not generalize to long-term smoking abstinence. Future studies should address this important area of research. Finally, our exploratory analyses focused on one conceptualization of tobacco dependence, the HSI. Future studies might use multiple measures of tobacco dependence to examine for consistency of associations across measures both within and between racial groups.
In conclusion, the current study adds to the extant literature on relations between menthol cigarette use and smoking cessation, and suggests that menthol use is related to increased difficulty in successfully quitting smoking among treatment-seeking White smokers. These results, coupled with other research citing similar effects among White (Delnevo et al., 2011; Kahende et al., 2011; Reitzel et al., 2011) and Black smokers (Foulds et al., 2010), can inform the future actions taken by the Food and Drug Administration with regard to the banning of mentholated flavorings in cigarettes.
FUNDING
This work was supported by grants from the Centers for Disease Control and Prevention (K01DP000086 to JIV), and the National Institutes of Health through MD Anderson’s Cancer Center Support Grant (CA016672), as well as by start-up funds (to LRR) as provided by The University of Texas MD Anderson Cancer Center. The contents of this work are solely the responsibility of the authors and do not necessarily represent the official views of the project supporters.
DECLARATION OF INTERESTS
None declared.
ACKNOWLEDGMENTS
We would like to acknowledge the research staff at The University of Texas MD Anderson Cancer Center who assisted with implementation of the original project. We would also like to thank Ms. Nga Nguyen of the University of Texas MD Anderson Cancer Center for her expert assistance with statistical programming.
REFERENCES
- Agresti A. (2002). Categorical data analysis (2nd ed.). Hoboken, NJ: John Wiley & Sons; doi:10.2307/1269816 [Google Scholar]
- Ahijevych K., Garrett B. E. (2004). Menthol pharmacology and its potential impact on cigarette smoking behavior. Nicotine & Tobacco Research, 6(Suppl. 1), S17–S28 doi:10.1080/14622200310001649469 [DOI] [PubMed] [Google Scholar]
- Ahijevych K., Garrett B. E. (2010). The role of menthol in cigarettes as a reinforcer of smoking behavior. Nicotine & Tobacco Research, 12(Suppl. 2), S110–S116 doi:10.1093/ntr/ntq203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alexander L. A., Crawford T., Mendiondo M. S. (2010). Occupational status, work-site cessation programs and policies and menthol smoking on quitting behaviors of US smokers. Addiction, 105(Suppl. 1), 95–104 doi:10.1111/j.1360-0443. 2010.03227.x [DOI] [PubMed] [Google Scholar]
- Anderson S. J. (2011). Marketing of menthol cigarettes and consumer perceptions: A review of tobacco industry documents. Tobacco Control, 20(Suppl. 2), ii20–ii28 doi:10.1136/tc.2010.041939 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bender R., Benner A. (2000). Calculating ordinal regression models in SAS and S-Plus. Biometrical Journal, 42, 677–699 doi:10.1002/1521-4036(200010)42:6<677::AID-BIMJ677> 3.3.CO;2-F [Google Scholar]
- Borland R., Yong H. H., O’Connor R. J., Hyland A., Thompson M. E. (2010). The reliability and predictive validity of the Heaviness of Smoking Index and its two components: Findings from the International Tobacco Control Four Country study. Nicotine & Tobacco Research, 12(Suppl.), S45–S50 doi:10.1093/ntr/ntq038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark P. I., Gardiner P. S., Djordjevic M. V., Leischow S. J., Robinson R. G. (2004). Menthol cigarettes: Setting the research agenda. Nicotine & Tobacco Research, 6(Suppl. 1), S5–S9 doi:10.1080/14622200310001649441 [DOI] [PubMed] [Google Scholar]
- Delnevo C. D., Gundersen D. A., Hrywna M., Echeverria S. E., Steinberg M. B. (2011). Smoking-cessation prevalence among U.S. smokers of menthol versus non-menthol cigarettes. American Journal of Preventive Medicine, 41, 357–365 doi:10.1016/j.amepre.2011.06.039 [DOI] [PubMed] [Google Scholar]
- Fagan P., Moolchan E. T., Hart A., Jr., Rose A., Lawrence D., Shavers V. L., Gibson J. T. (2010). Nicotine dependence and quitting behaviors among menthol and non-menthol smokers with similar consumptive patterns. Addiction, 105(Suppl. 1), 55–74 doi:10.1111/j.1360-0443.2010.03190.x [DOI] [PubMed] [Google Scholar]
- Fagerström K., Russ C., Yu C.-R., Yunis C., Foulds J. (2012). The Fagerstrom Test for Nicotine Dependence as a predictor of smoking abstinence: A pooled analysis of varenicline clinical trial data. Nicotine & Tobacco Research [Epub ahead of print]. doi:10.1093/ntr/nts018 [DOI] [PubMed] [Google Scholar]
- Foulds J., Hooper M. W., Pletcher M. J., Okuyemi K. S. (2010). Do smokers of menthol cigarettes find it harder to quit smoking? Nicotine & Tobacco Research, 12(Suppl. 2), S102–S109 doi:10.1093/ntr/ntq166 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fu S. S., Okuyemi K. S., Partin M. R., Ahluwalia J. S., Nelson D. B., Clothier B. A., Joseph A. M. (2008). Menthol cigarettes and smoking cessation during an aided quit attempt. Nicotine & Tobacco Research, 10, 457–462 doi:10.1080/14622200801901914 [DOI] [PubMed] [Google Scholar]
- Gandhi K. K., Foulds J., Steinberg M. B., Lu S. E., Williams J. M. (2009). Lower quit rates among African American and Latino menthol cigarette smokers at a tobacco treatment clinic. International Journal of Clinical Practice, 63, 360–367 doi:10.1111/j.1742-1241.2008.01969.x [DOI] [PubMed] [Google Scholar]
- Gardiner P. S. (2004). The African Americanization of menthol cigarette use in the United States. Nicotine & Tobacco Research, 6(Suppl. 1), S55–S65 doi:10.1080/14622200310001649478 [DOI] [PubMed] [Google Scholar]
- Gardiner P., Clark P. I. (2010). Menthol cigarettes: Moving toward a broader definition of harm. Nicotine & Tobacco Research, 12(Suppl. 2), S85–S93 doi:10.1093/ntr/ ntq176 [DOI] [PubMed] [Google Scholar]
- Giovino G. A., Sidney S., Gfroerer J. C., O’Malley P. M., Allen J. A., Richter P. A., Cummings K. M. (2004). Epidemiology of menthol cigarette use. Nicotine & Tobacco Research, 6(Suppl. 1), S67–S81 doi:10.1080/14622203710001649696 [DOI] [PubMed] [Google Scholar]
- Gundersen D. A., Delnevo C. D., Wackowski O. (2009). Exploring the relationship between race/ethnicity, menthol smoking, and cessation, in a nationally representative sample of adults. Preventive Medicine, 49, 553–557 doi:10.1016/ j.ypmed.2009.10.003 [DOI] [PubMed] [Google Scholar]
- Healton C. G., Bullock A. T., Robinson W. S., Beck S. E., Cartwright J., Eubanks S. Y. (2010). Why we should make menthol cigarettes history. Nicotine & Tobacco Research, 12(Suppl. 2), S94–S97 doi:10.1093/ntr/ntq177 [DOI] [PubMed] [Google Scholar]
- Heatherton T. F., Kozlowski L. T., Frecker R. C., Rickert W., Robinson J. (1989). Measuring the heaviness of smoking: Using self-reported time to the first cigarette of the day and number of cigarettes smoked per day. British Journal of Addiction, 84, 791–799 doi:10.1111/j.1360-0443.1989.tb03059.x [DOI] [PubMed] [Google Scholar]
- Hyland A., Garten S., Giovino G. A., Cummings K. M. (2002). Mentholated cigarettes and smoking cessation: Findings from COMMIT. Community Intervention Trial for Smoking Cessation. Tobacco Control, 11, 135–139 doi:10.1136/tc.11.2.135 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kabat G. C., Morabia A., Wynder E. L. (1991). Comparison of smoking habits of blacks and whites in a case-control study. American Journal of Public Health, 81, 1483–1486 doi:10.2105/AJPH.81.11.1483 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kahende J. W., Malarcher A. M., Teplinskaya A., Asman K. J. (2011). Quit attempt correlates among smokers by race/ethnicity. International Journal of Environmental Research and Public Health, 8, 3871–3888 doi:10.3390/ijerph8103871 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kreslake J. M., Wayne G. F., Alpert H. R., Koh H. K., Connolly G. N. (2008). Tobacco industry control of menthol in cigarettes and targeting of adolescents and young adults. American Journal of Public Health, 98, 1685–1692 doi:10.2105/AJPH.2007.125542 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lawrence D., Rose A., Fagan P., Moolchan E. T., Gibson J. T., Backinger C. L. (2010). National patterns and correlates of mentholated cigarette use in the United States. Addiction, 105(Suppl. 1), 13–31 doi:10.1111/j.1360-0443.2010.03203.x [DOI] [PubMed] [Google Scholar]
- Levy D. T., Blackman K., Tauras J., Chaloupka F. J., Villanti A. C., Niaura R. S.… Abrams D. B. (2011). Quit attempts and quit rates among menthol and nonmenthol smokers in the United States. American Journal of Public Health, 101, 1241–1247 doi:10.2105/AJPH.2011.300178 [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKinnon D. (2008). Introduction to statistical mediation analysis New York, NY: Taylor and Francis Group; [Google Scholar]
- MacKinnon D. P., Lockwood C. M., Brown C. H., Wang W., Hoffman J. M. (2007). The intermediate endpoint effect in logistic and probit regression. Clinical Trials, 4, 499–513 doi:10.1177/1740774507083434 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGowan M. J. (2000). Ordinal outcomes with the continuation ratio model. Paper presented at the Proceedings of the Northeast SAS Users Group Conference, Philadelphia, PA [Google Scholar]
- Muscat J. E., Chen G., Knipe A., Stellman S. D., Lazarus P., Richie J. P., Jr. (2009). Effects of menthol on tobacco smoke exposure, nicotine dependence, and NNAL glucuronidation. Cancer Epidemiology Biomarkers & Prevention, 18, 35–41 doi:10.1158/1055-9965.EPI-08-0744 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muscat J. E., Richie J. P., Jr., Stellman S. D. (2002). Mentholated cigarettes and smoking habits in whites and blacks. Tobacco Control, 11, 368–371 doi:10.1136/tc.11.4.368 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Okuyemi K. S., Ahluwalia J. S., Ebersole-Robinson M., Catley D., Mayo M. S., Resnicow K. (2003). Does menthol attenuate the effect of bupropion among African American smokers? Addiction, 98, 1387–1393 doi:10.1046/j.1360-0443. 2003.00443.x [DOI] [PubMed] [Google Scholar]
- Okuyemi K. S., Faseru B., Sanderson Cox L., Bronars C. A., Ahluwalia J. S. (2007). Relationship between menthol cigarettes and smoking cessation among African American light smokers. Addiction, 102, 1979–1986 doi:10.1111/j.1360- 0443.2007.02010.x [DOI] [PubMed] [Google Scholar]
- Pletcher M. J., Hulley B. J., Houston T., Kiefe C. I., Benowitz N., Sidney S. (2006). Menthol cigarettes, smoking cessation, atherosclerosis, and pulmonary function: The Coronary Artery Risk Development in Young Adults (CARDIA) Study. Archives of Internal Medicine, 166, 1915–1922 doi:10.1001/archinte.166.17.1915 [DOI] [PubMed] [Google Scholar]
- R Core Team (2012). R: A language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing; Retrieved from http://www.R-project.org/ [Google Scholar]
- Reitzel L. R., Nguyen N., Cao Y., Vidrine J. I., Daza P., Mullen P. D. … Wetter D. W. (2011). Race/ethnicity moderates the effect of prepartum menthol cigarette use on postpartum smoking abstinence. Nicotine & Tobacco Research, 13, 1305–1310 doi:10.1093/ntr/ntr095 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singer J. D., Willett J. B. (1993). It’s about time: Using discrete-time survival analysis to study duration and the timing of events. Journal of Educational Statistics, 18, 155–195 doi:10.2307/1165085 [Google Scholar]
- Stahre M., Okuyemi K. S., Joseph A. M., Fu S. S. (2010). Racial/ethnic differences in menthol cigarette smoking, population quit ratios and utilization of evidence-based tobacco cessation treatments. Addiction, 105(Suppl. 1), 75–83 doi:10.1111/j.1360-0443.2010.03200.x [DOI] [PubMed] [Google Scholar]
- Sutton C. D., Robinson R. G. (2004). The marketing of menthol cigarettes in the United States: Populations, messages, and channels. Nicotine & Tobacco Research, 6(Suppl. 1), S83–S91 doi:10.1080/14622203310001649504 [DOI] [PubMed] [Google Scholar]
- Trinidad D. R., Perez-Stable E. J., Messer K., White M. M., Pierce J. P. (2010). Menthol cigarettes and smoking cessation among racial/ethnic groups in the United States. Addiction, 105(Suppl. 1), 84–94 doi:10.1111/j.1360-0443. 2010.03187.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Willett J. B., Singer J. D. (1993). Investigating onset, cessation, relapse, and recovery: Why you should, and how you can, use discrete-time survival analysis to examine event occurrence. Journal of Consulting and Clinical Psychology, 61, 952–965 doi:10.1037//0022-006X.61.6.952 [DOI] [PubMed] [Google Scholar]
- Williams J. M., Gandhi K. K., Steinberg M. L., Foulds J., Ziedonis D. M., Benowitz N. L. (2007). Higher nicotine and carbon monoxide levels in menthol cigarette smokers with and without schizophrenia. Nicotine & Tobacco Research, 9, 873–881 doi:10.1080/14622200701484995 [DOI] [PubMed] [Google Scholar]
- Yerger V. B., Przewoznik J., Malone R. E. (2007). Racialized geography, corporate activity, and health disparities: Tobacco industry targeting of inner cities. Journal of Health Care for the Poor and Underserved, 18(4 Suppl.), 10–38 doi:10.1353/hpu.2007.0120 [DOI] [PubMed] [Google Scholar]


