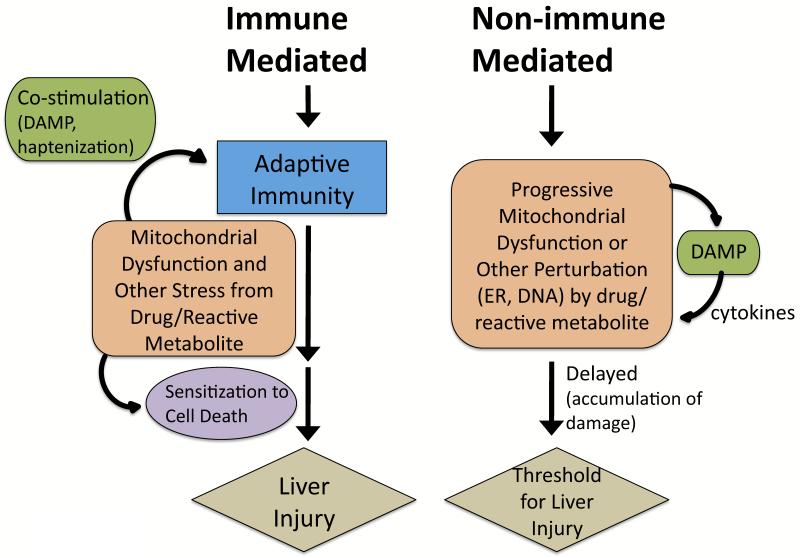
Figure 1. Immune-mediated and non-immune-mediated idiosyncratic DILI.
Many drugs cause idiosyncratic DILI via an adaptive immune system mediated process and have strong associations with certain HLA haplotypes, even though they do not display classic characteristics of systemic immune hypersensitivity (i.e. fever, rash, eosinophilia, rapid positive rechallenge). Drugs/reactive metabolites may stress hepatocytes to stimulate the adaptive immune system. Excessive reactive metabolites bind to proteins (haptenization), and peptide-haptens exposed in the binding grove of HLA molecules then stimulate T-cells. Hepatocytes may become injured and release contents, such as mtDNA, that act as danger associated molecular pattern (DAMP) molecules that co-activate the immune system (sterile inflammation) [97]. Extensive drug-induced stress in hepatocytes may alter signaling pathways to sensitize hepatocytes to the adaptive immune system. Non-allergic DILI is believed to be mediated by biochemical injury, often involving mitochondria. The drug/reactive metabolite stress and injury to hepatocytes may need to accumulate (long latency) before manifestations of DILI are observed. DAMP molecules may also be released in this process and activate cytokines that may mediate injury. Mitochondria have a reserve respiratory capacity and significant inhibition of complexes is needed before bioenergetic capacity is impaired. Thus, drugs/reactive metabolites can damage mitochondria gradually, with no observable effects on mitochondrial respiration until a critical threshold is reached. How often non-immune idiosyncratic DILI occurs is unknown but remains plausible.