Figure 2. SCHEMATIC MODEL OF CHRONIC DESTRESS AND PERPETUATION OF PSYCHIATRIC SYMPTOMS AND DRUG USE IN INDIVIDUALS WITH COMORBID DISORDERS5.
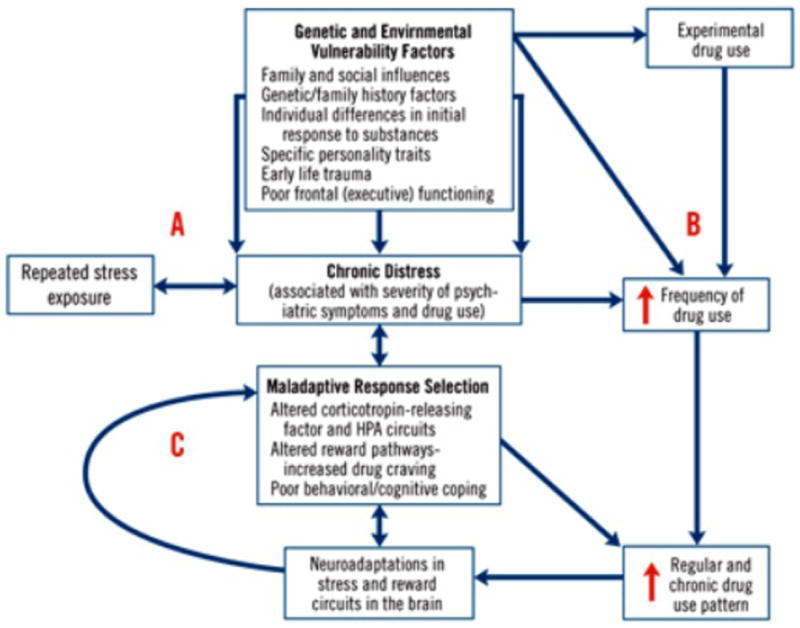
Various genetic and environmental vulnerability factors contribute to the development of psychiatric/emotional distress (A) and to drug abuse (B). Chronic distress is a common construct underlying both the disabling psychiatric symptoms associated with specific psychiatric disorders and the increasing distress associated with severity of substance use disorder. Chronic distress states are associated with selection of maladaptive responses, such as drug use, in order to attain desired goals or homeostasis. Maladaptive response selection mechanisms are associated with alterations in various neurotransmitter systems (including corticotropin-releasing factor and hypothalamic-pituitary-adrenal circuits), increased levels of stress-inducing drug craving, and poor adaptive coping, representing neuroadaptations in the stress and reward circuits (C). This mechanism contributes to the escalation of drug use to the chronic levels characteristic of dependence, supporting a feed-reward loop that leads to greater alterations in stress and reward systems. These alterations perpetuate chronic distress and susceptability to repeated stress exposures, thereby promoting a cycle of distress and drug use in individuals with comorbid disorders.
Brady KT, Sinha R. Co-occurring mental and substance use disorders: the neurobiological effects of chronic stress. Am J Psychiatry. 2005; 162(8): l483-1493. Reprinted with permission from the American Psychiatric Association. Copyright 2005.
HPA=hypothalamic-pituitary-adrenal
