Abstract
Background
Homeless youth are at high risk for HIV infection as a consequence of risky sexual behavior. Interventions in homeless youth are challenging. Assessment of the effectiveness of interventions to modify sexual risk behaviours for preventing HIV in homeless youth is needed.
Objectives
To evaluate and summarize the effectiveness of interventions for modifying sexual risk behaviours and preventing transmission of HIV among homeless youth.
Search methods
We searched electronic databases (CENTRAL, Medline, EMBASE, AIDSearch, Gateway, PsycInfo, LILACS), reference lists of eligible articles, international health agency publication lists, and clinical trial registries. The search was updated January 2010. We contacted authors of published reports and other key role players.
Selection criteria
Randomized studies of interventions to modify sexual risk behavior (biological, self-report sexual-risk behavior or health seeking behavior) in homeless youth (12–24 years).
Data collection and analysis
Data from eligible studies were extracted by two reviewers. We assessed risk of bias per the Cochrane Collaborations tool. None of the eligible studies reported any primary biological outcomes for this review and the reporting of self-report sexual risk behavior outcomes was highly variable across studies precluding calculation of summary measures of effect; we present the outcomes descriptively for each study. We contacted authors for missing or ambiguous data.
Results
We identified three eligible studies after screening a total of 255 unique records. All three were performed in the United States of America and recruited substance-abusing male and female adolescents (total N=615) through homeless shelters into randomised controlled trials of independent and non-overlapping behavioural interventions. The three trials differed in theoretical background, delivery method, dosage (number of sessions,) content and outcome assessments. Overall, the variability in delivery and outcomes precluded estimation of summary of effect measures. We assessed the risk of bias to be high for each of the studies. Whilst some effect of the interventions on outcome measures were reported, heterogeneity and lack of robustness in these studies necessitate caution in interpreting the effectiveness of these interventions.
Authors’ conclusions
The body of evidence does not permit conclusions on the impact of interventions to modify sexual risk behaviour in homeless youth. More research is required. While the psychosocial and contextual factors that fuel sexual risk behaviours among homeless youth challenge stringent methodologies of RCT’s, novel ways for program delivery and trial retention are in need of development. Future trials should endeavour to comply with rigorous methodology in design, delivery, outcome measurement and reporting.
Plain language summary
Ways to reduce risky sexual behavior in homeless youth to prevent HIV
There have been a limited number of rigorously conducted interventions to modify the sexual behavior of homeless youth 12–24 years of age to prevent them acquiring HIV. More research is required to identify effective strategies for this population. In this review we systematically searched published and unpublished accounts of interventions that had been rigorously tested. We found three eligible independently conducted randomised controlled trials testing three different interventions, all conducted in the United States, amongst a total of 615 homeless, male and female youth that tested three different interventions. Due to the variability in fidelity of delivery of interventions and in outcome measurement and reporting, we were unable to aggregate outcomes to estimate summary of effect measures. The significant risk of bias associated with the three included studies and their heterogeneity necessitate caution in interpreting the effectiveness of interventions to modify sexual risk behavior for preventing HIV in homeless youth. While studies along homeless youth are highly challenging, future trials should endeavour to comply with rigorous methodology in design, delivery, outcome measurement and reporting and consider the changing face of homeless youth and HIV prevention tools.
Background
Although youth is generally considered the healthiest phase of life, it is also a time of exploration and experimentation, with sexual identity and sexual practices and behaviours being major areas of development and change. Youth (aged 15–24 years) comprise about 18% (1.2 billion) of the global population of around 6.7 billion people (United Nations 2007). The unique biopsychosocial changes associated with this age group result in disproportionate risk of HIV infection. Youth, therefore, are at the centre of the human immunodeficiency virus (HIV) pandemic (Ross 2006, Doyle AM 2010), but while estimates of the HIV burden of disease in adults (15–49 years) are routinely made, it is more difficult to gauge trends in the HIV disease burden amongst youth due to legal, ethical and moral constraints.
One of the most vulnerable groups is homeless youth, many of whom are forced by circumstance to engage in a variety of risky behaviours and who often are least likely to seek and/or have access to HIV prevention counselling, testing, and care. Unique strategies and interventions to reduce HIV acquisition sexually and through recreational drug use in this vulnerable group therefore may be necessary.
The focus of this review is to evaluate and summarize the effectiveness of interventions for preventing HIV by modifying sexual risk behaviours in homeless youth.
Definition of terms
The terms “youth,” “adolescent/teenager,” and “young adult” are often used interchangeably but at the same time are context and culture specific. Since 1985 (International Youth year), the United Nations has referred to people between the ages of 13 and 19 as teenagers and between the ages of 20 and 24 years as young adults; youth are defined as being between 15 and 24 years of age. It is estimated that in 2004, half of all HIV infections occurred in youth, and about 98% of the 10 million youth living with HIV/AIDS worldwide were in middle-or low-income countries (UNAIDS 2004). For the purposes of this review we adopted a definition of youth being between the ages 12 and 24 years (inclusive).
The term “homeless youth” refers to a wide variety of young people (i.e. runaway, throwaway, unaccompanied, street, and systems youth). Various countries have developed their own definitions of “homelessness” among youth. These are often linked to the reason for their homelessness, with youth often emphasizing the throwaway and parents the runaway justification (Hammer 2002). A runaway is a youth who is away from home without the permission of parents or guardians; a throwaway is a young person who was asked to leave home by either parents/guardians or adults in the household (Hammer 2002). Girls seem more likely to be runaways (Hammer 2002) because of sexual abuse (Cauce 2000) while boys are more likely to be throwaways, possibly because of a greater likelihood of deviant behaviour (Moore 2006).
The term “street youth” can refer to homeless youth who live in high-risk, non-traditional places, such as under bridges, in abandoned buildings, and on the street, or to those whose lives are focused on the street (i.e., youth spending most of their time on the street and fending for themselves) but return to their homes on a regular basis. It should be noted that reference to the word “street” when discussing homeless youth is considered derogative by some investigators (Panter-Brick 2002). Street youth can be defined further in terms of context:
Street-living - youth who ran away from their families and live alone on the streets
Street-working youth who spend most of their time on the streets and fend for themselves but return home on a regular basis
Street-family - youth who live on the streets with other (unrelated) street youth as a group.
In addition, many street youth may be youth who have no family as a result of AIDS related deaths in parents and other family members. This population of street youth is of growing importance in areas of high HIV prevalence.
Systems youth on the other hand are considered to be linked to government systems, such as juvenile justice or foster care, and are homeless due to abuse, neglect, or family incarceration or homelessness (Moore 2006). When a systems youth become homeless it is often because they have run away from a home placement or because the placement failed to provide a stable living environment (Moore 2006). In addition, a common reason for a youth becoming homeless in the USA is ageing out of the youth foster care system. Against this background, it is clear that homeless youth are a heterogenous group with unique contexts and needs. The hidden and transient nature of homeless youth make it difficult to estimate their numbers (Raleigh-DuRoff 2004), primarily, among other reasons because service providers and concerned adults attempt to “protect” youth from police and social services (Kidd 2004; Taylor 2004). UNICEF (2004) estimates that there are about 100 million children who live on the street either all or part of the year. In the United States it is estimated that about 1.5 to 2 million youths per year are homeless or run away from home (Moore 2006). These estimates likely underestimate the number of youth who are homeless in a broader definition inclusive of orphans and vulnerable children (OVC) in contexts of poverty, war, famine, and HIV/AIDS. Crucially, there is a new and large cohort of homeless children and youth that have emerged as a result of premature death of parents, aunts, uncles due to AIDS. This growing population is, by definition, coincident with the greatest population-level HIV risk in sub-Saharan Africa, Eastern Europe and South-East Asia. In 2008, roughly 18 million children (aged less than 18 years) had been orphaned by AIDS in Sub-Saharan Africa alone (UNAIDS 2009), but what proportion end up on the streets is not known. Homeless youth in general, urgently and desperately need interventions not only targeting HIV risk reduction but also addressing gaps in social safety nets.
Why it is important that interventions in this population be reviewed?
Homeless youth are highly vulnerable to HIV acquisition and transmission regardless of whether they live in a country with a focussed or a generalized epidemic, as they live lives of heightened personal and social risk often marked by violence, victimisation and human rights abuses (Boivin 2005; Greene 1997; MacLean 1999; Ramphele MA 1997; Ribeiro 2001). As a group, they lack the economic, social, and emotional resources to provide for their basic needs, such as adequate sleep, clothing, shelter, and nutrition, which has dire consequences for their physical and emotional health (Van Wormer 2003). Studies have indicated that homeless youth have significant health risks related to sexual behaviour and substance use and linked to increased risk for HIV/AIDS and other STIs (Anarfi 1997; Baybuga 2004; de Carvalho 2006; Richter 1995; Walters 1999). In a review of 52 studies of the health of street youth in industrialized countries, these youth had higher rates of hepatitis B, C, and HIV than their non-street peers (Boivin 2005). Homeless youth, therefore, are of particular importance as a population at high risk for acquiring HIV infection.
The behaviours of youth are influenced by a range of factors including individual knowledge and attitudes; relationships with parents, caregivers, and peers; academic/school performance; socioeconomic and environmental contexts; and access to health services. It is generally understood that the majority of youth are sexually active, do not have monogamous sexual relationships, and do not use condoms consistently, as is reflected in the increasing prevalence of HIV among youth worldwide (United Nations 2007). Risk behaviours among youth are often understood in terms of risk clustering, as different risk behaviours occur simultaneously, such as substance use and unprotected sex and sometimes delinquency. These behaviours also seem to have common determinants, meaning that they are affected by the same risk and protective factors (UNAIDS 2004).
Knowledge of sexuality (Gatu 2000; Richter 1995) and HIV/AIDS among homeless youth is generally inadequate and not translated into preventive behaviours (Baybuga 2004; Bernier 1995; Gatu 2000; Robinson 2001; Snell 2002). Homeless youth are highly vulnerable to engaging in unprotected survival sex to meet their basic needs and/or feed a drug habit (Bernier 1995; Walters 1999) and are subject to rape (Swart-Kruger 1997). Because of their psychosocial and contextual environments, they also are highly likely to have multiple sexual partners (de Carvalho 2006; Haley 2004; Poulin 2001; Richter 1995; Roy 2000; Swart-Kruger 1997; van den Hoek 1997). Most are poorly equipped to combat sexual threats, as reported in an ongoing study of Montreal street youth, where only 13.2% of participants reported always using condoms during vaginal intercourse, and only 32.4% reported always using condoms during anal intercourse (Roy 2000). Homeless youth are more likely to engage in self-destructive behaviours, including suicide attempts, substance abuse (especially alcohol) and injecting drug use, than are other youth (Rew 2001; Ringwalt 1998; Roy 2004). Suicide and drug overdose were reported to be two primary observed causes of mortality among homeless youth in a Canadian study (Roy 2004). The engagement in self-destructive behaviours is linked to psychological triggers, such as post-traumatic stress disorder (Cauce 2000), low self-esteem, and feelings of loneliness and hopelessness (Boivin 2005). These factors in turn accelerate and perpetuate the cycle of HIV vulnerability. In addition to traditional risk factors for HIV acquisition such as injection drug use, sharing needles, sexually transmistted infections or lack of condom use, having no place to live or being an orphan are independently associated with higher HIV prevalence in street youth (Kissin 2007, Robbins 2010).
Because they are marginalized and underserved, homeless youth do not have adequate access to social and health services, including health education (Baybuga 2004; Snell 2002). Their HIV risk thus not only is related to their sexual practices, but also are linked to various predisposing and enabling factors that emerge from their psychosocial and contextual vulnerabilities (Lambert 2005).
In response to the need to address HIV/AIDS prevention worldwide, most countries have embarked on intensive mass media-, community-, and group-level interventions and the introduction of widespread antiretroviral treatment programmes (UNAIDS December 2007, 2007). Randomised controlled trials undertaken in various countries have shown a reduction of high-risk sexual practices by youth who have taken part in behavioural interventions (DiClemente 1995; Kegeles 1996; Ross 2006; Underhill 2008).
Interventions directed specifically at modifying the sexual risk behaviours of homeless youth have unique challenges. Implementing workable and practical programmes for heterogeneous mobile populations in non-health care settings are difficult. Furthermore, for members of a group in which social and economic indigence may make it difficult to assert their sexual rights, HIV-prevention messages could be viewed as irrelevant. Peer education and community-based interventions have been implemented to reduce HIV risk among homeless youth. (Rotheram-Borus 1993; Rotheram-Borus 1997; Rotheram-Borus 1999). It has been argued that the ability of the programme to respond to the needs of youth stems from creative service approaches in which youth are involved in program design and in delivering the programme near where youths gather (Tenner 1998). Participatory and tailored interventions seem to be effective in meeting the diverse needs of marginalized youth (Tenner 1998).
This review will identify and allow lessons learned from effective interventions to guide the development and implementation of future HIV-risk reduction, behavioural modification interventions for homeless youth.
Objectives
To evaluate and summarize the effectiveness of interventions for modifying sexual risk behaviours and preventing transmission of HIV/AIDS among homeless youth
Methods
Criteria for considering studies for this review
Types of studies
Randomised controlled trials that have evaluated the behavioural effects and, where possible, the biological outcomes (e.g., STIs and HIV infection) of interventions for HIV prevention in homeless youth were included.
Types of participants
For the purposes of this review we included all homeless persons between the ages of 12–24 years (inclusive) regardless of HIV status, location, reason for homelessness, or gender. This definition is inclusive of homeless young people/adults, adolescents/teenagers and youth. A homeless youth is a person who lacks a fixed, regular, and adequate nighttime residence; and is an individual who has a primary nighttime residence that is:
a supervised publicly or privately operated shelter designed to provide temporary living accommodations (including welfare hotels, congregate shelters, and transitional housing for the mentally ill);
an institution that provides a temporary residence for individuals intended to be institutionalised; or
a public or private place not designed for, or ordinarily used as, a regular sleeping accommodation for human beings (US Code Title 42).
Interventions amongst systems and street youth (see Background) were encompassed by the terms “homeless”, “runaway” or “throwaway” and were potentially eligible for review.
Types of interventions
Any type of intervention including behavioral, social, policy, structural, or other interventions explicitly aimed at reducing sexual risk behavior in homeless youth was included. Interventions delivered to individuals, small groups, or entire communities were eligible. Mantell has described the components an intervention should have to be termed a behavioural, social, policy, or structural intervention (Mantell 1997).
An intervention has a behavioral component if it aims to change individual behavior without an explicit attempt to change peer or social norms that may influence a person’s behavior. It tends to emphasize individual and small-group approaches and includes psychosocial/cognitive interventions. Examples include one-on-one interventions (e.g., HIV counselling and testing, notification assistance, support, peer interventions, role plays, tabling, AIDS hotline, HIV prevention technology); single event interventions (e.g., theatre, drama, video presentation, home risk-reduction parties), and multi-session interventions (e.g., skills-building and problem-solving workshops, training programs).
An intervention has a social component if it aims to change individual behavior by explicitly attempting to change peer or social norms that may influence a person’s behavior. Examples include outreach interventions, engaging opinion leaders as educators, community mobilization, ethnographic interventions, small media-based interventions (e.g., using videos, brochures, pamphlets, newsletters, posters, and other print material), mass media-based interventions (e.g., using television, radio, films, talk-shows, news casts, soaps, videos, music, posters, billboards, and public service announcements), community-based interventions using existing family networks/creating new social networks.
An intervention has a policy component if it aims to change individual behavior or peer/social norms or structures that may influence a person’s behavior through administrative or legal decisions. Examples include mandatory HIV/AIDS education in all schools within a district.
An intervention has a structural component if it aims to change individual behavior by making changes in people’s environment. Examples include providing condom dispensers in bars and accompanying girls home from school to ensure their safety.
Interventions may contain any or a combination of these components. These mixed interventions will be reported as such.
Types of outcome measures
Outcome measures based on the indicators for monitoring and evaluating national HIV/AIDS prevention programmes for young people (WHO 2004) were used.
Primary outcomes: HIV infection, STI infection or pregnancy
Secondary outcomes: self-reported abstinence or intentions regarding abstinence, condom use, unprotected intercourse, refusal of intercourse with no condom, frequency of consensual intercourse, frequency of non-consensual intercourse, type of intercourse (i.e., oral, vaginal, insertive-anal, receptive-anal), type of partner (i.e., same-gender, different gender), number of partners, mutual monogamy, intercourse while intoxicated
Tertiary outcomes: visiting STI clinic, receiving pre-test counselling, taking an HIV test, receiving post-test counselling
We also included composite outcomes that included any of the above.
Search methods for identification of studies
Electronic searches
The following electronic databases were searched for RCTs for the period 1981 to December 2010 in two phases (Initial search: 1 August 2008, updated on 13 January 2010): Medline (Appendix 5); EMBASE(Appendix 3); AIDSearch(Appendix 1); PsycInfo (Appendix 6) and LILACS (Appendix 7). The Cochrane Database of Systematic Reviews, Database of Abstracts of Reviews of Effectiveness and the Cochrane Central Register of Controlled Trials (CENTRAL, Appendix 2) in The Cochrane Library were also searched through January 2010. We formulated comprehensive and exhaustive search strategies (Appendices) in an attempt to identify all relevant studies regardless of language or publication status (i.e., published, unpublished, in press, and in progress). Full details of the Cochrane HIV/AIDS Review Group methods and the journals hand searched are published on Collaborative Review Groups in the Cochrane Library. We used the RCT search strategy developed by The Cochrane Collaboration and detailed in the Cochrane Reviewers’ handbook in combination with terms specific to “sexual risk” AND “behaviour” AND “homeless” AND “HIV” AND “youth”; the full search strategies are shown in Appendices.
Other
Grey Literature
The abstracts of relevant conferences, including the International Conferences on AIDS and the Conference on Retroviruses and Opportunistic Infections, as indexed by AIDSearch and/or Gateway, were reviewed. The publication websites of the World Health Organization, UNAIDS, CDC, and UNICEF were checked for references to technical reports or similar items that may relate to this topic and the reference lists of technical reports from UNAIDS were also searched.
Reference Lists
The search strategy was iterative, in that references of eligible studies were searched for additional references. Existing meta-analyses were reviewed and the reference lists checked for further articles. The reference lists of all review and primary publications identified were searched.
Correspondence
Researchers involved in HIV prevention were contacted for published and unpublished data and relevant information. Authors of potentially eligible trials were contacted for additional information, as appropriate.
Clinical Trial Registries
The following clinical trial registries were searched using terms describing homeless, HIV/AIDS, sexual behavior: clinicaltrials.gov and WHO International Clinical Trials Registry Platform. We also searched clinical trial registries using the author names of each potentially eligible study to identify additional studies they may have been, or may currently be actively involved in.
Data collection and analysis
Selection of studies
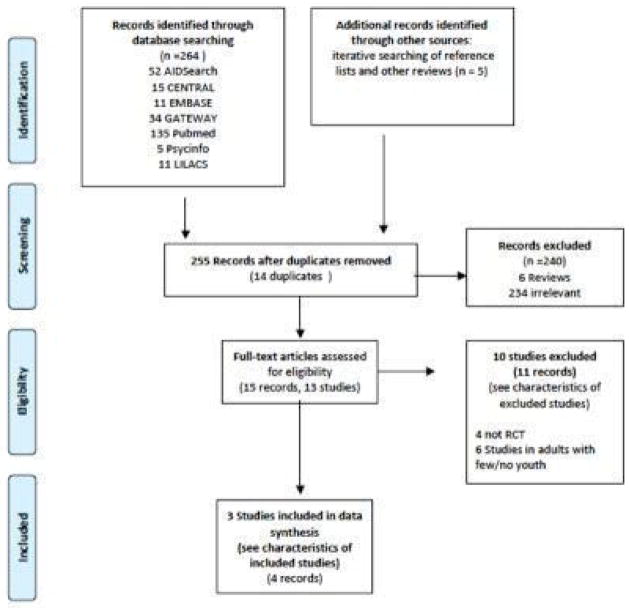
See also Figure 1.
Figure 1.
PRISMA Diagram showing identification, screening, eligibility and inclusion of studies in this review.
The titles and abstracts of all studies identified by electronic searches were screened by two independent authors (VN and AM) to shortlist studies for possible inclusion in the review. Full manuscripts of short listed studies were obtained and scrutinized independently by two reviewers (VN and AM) to establish eligibility based on design, participants, intervention and outcomes reported. Neither author was blinded to the names of authors, institutions, journal of publication or results. Disagreements were handled initially by discussion between reviewers and if no agreement resulted, a third reviewer (QAK) was consulted.
Data extraction and management
Data from eligible studies were extracted by two independent reviewers (VN and AM) onto standardized data collection forms and entered into Revman 5.0.24.
Assessment of risk of bias in included studies
The methodological rigor of the studies was independently assessed by two reviewers using the Cochrane Collaboration’s tool for assessing risk of bias to assess the risk of selection, performance, attrition, and detection bias. Briefly, the following domains were evaluated and rated as “adequate,” “inadequate,” or “unclear”: sequence generation; allocation concealment; blinding of participants, personnel, or outcome; incomplete outcome data; selective outcome reporting; and other sources of bias.
Measures of treatment effect
For RCTs, we attempted to calculate the RR for dichotomous outcomes and the 95% CI. For continuous data we aimed to calculate a weighted-mean difference. Due to the significant heterogeneity both in types of interventions, types of outcomes reported and lack of reporting standard, we were unable to combine data for meta-analysis.
Dealing with missing data
For missing or ambiguous data, authors of the studies were contacted both at eligibility assessment and data abstraction stages. We received responses from all except one of the authors contacted (7/8).
Results
Description of studies
Results of the search
As at January 2010 we obtained a total of 255 unique reports by our search strategy (see Figure 1). A total of 240 records were eliminated at screening, leaving 15 eligible reports that were examined in detail for eligibility assessment (full text obtained). Of the 15 reports, 11 reports of 10 independent studies were excluded and the remaining four reports detailed three suitable studies eligible for this review(Rotheram-Borus 2003, Slesnick 2005, Slesnick 2008).
Included studies
See characteristics of Included studies table.
Characteristics of included studies
| Rotheram-Borus 2003 | ||
| Methods | Cluster randomised controlled trial (start and end dates not reported). | |
| Participants | Four shelters in two clusters constituting a total of 311 runaway youth (11–18 years age, 49% female) admitted to one of three runaway shelters in New York City, USA or one runaway shelter in New Jersey, USA. The ethnicity of participants were: African American (59%), Hispanic (26%)and white/other (15%). The HIV status of participants was not assessed/reported. | |
| Interventions | Intervention: Street smart (2 shelters with a total of 167 youth) Control: ‘Current field practice’ (2 shelters with a total of 144 youth) Theoretical underpinnings of intervention: This intervention was based on social learning theory which holds that behaviour change can be effected by observational learning in a social context, imitation and overt reinforcement. The Streetsmart intervention addressed four components: training shelter staff in HIV education and counselling, providing training sessions for youth on social-skills training, making condoms available and providing access to health resources. Delivery, dosage and content of intervention Intervention was delivered in 10 small-group sessions over an approximately three week period (3 days/week). Sessions were led by a researcher and a shelter employee both trained in a 10 day training program run over 6 weeks preceding the study. All staff working at shelters (inclusive of cooks, social workers, security guards and shelter directors), in the intervention cluster received training. Each session started with exchanging compliments and reporting successes in HIV-prevention goals set at previous meetings followed by an overview of that sessions contents, and completed with delivery of actual content of the session including activities. and development of new goals and homework. The content of each session covered i) general and personal knowledge of HIV (including video and art workshops and role-play), ii) social-skills training (assertiveness, coping skills, use of the ‘feeling thermometer’ to identify emotional states in situations with HIV risk, and self-regulation skills to control feelings of anxiety, depression, anger and desire) and iii) addressing individual barriers to safer sex (delivered in private counselling sessions). Youth attending the sessions were rewarded with food at randomly selected sessions and USD1 for carrying a condom and arriving on time. The number of sessions received per youth highly correlated with length of stay in shelters. The mean number of sessions received was 9.2 (SD=6.13, range 1–28 sessions). Length of stay was longer at one shelter (4–6 weeks and youth completed the intervention i.e. at least 10 sessions). Condoms were made freely available in intervention shelters. Residents of intervention shelters made a weekly trip to an agency providing health and social services to youth. Details on control Current field practice consisted staff HIV education training but no systematic introduction of HIV prevention information to youth. HIV prevention activities occurred when staff provided individual counselling to youth and reviewed HIV prevention guidelines (e.g. condom use). |
|
| Outcomes | Sexual risk acts were evaluated through a 45-min structured interview at baseline, 3-,6-,12-, 18- and 24-months post intervention with each individual study participant by a staff interviewer not aware of the intervention status of the individual. During the interview participants reported the number of partners, specific sexual acts and whether condoms were used during each act. Three indices were calculated and reported:
|
|
| Notes | Investigators explain that it would not have been feasible to mount a properly powered trial consisting 22 shelters | |
| Risk of bias table | ||
| Item | Author’s Judgement | Description |
| Adequate sequence generation? | Unclear | Randomization procedure not reported. |
| Allocation concealment? | Yes | Cluster randomized-prior to triage of participants to shelter. |
| Blinding? | No | Participants and personnel were not uniformly blinded to study intervention and while study staff interviewers (assessors) were blinded to intervention, participants self-reporting were not |
| Incomplete outcome data addressed? | No | Differential, variable and large loss to follow up at each follow up period for both arms reported without reasons for loss. Losses were 76/167 and 58/144, 77/167 and 53/144, 98/167 and 58/144, 103/167 and 66/144, 57/167 and 37/144 for intervention and control arms at 3-,6-,12-,18- and 24 months. |
| Free of selective reporting? | No | In analysis, individuals with the lowest or highest risk behaviour were excluded as were youth who could not be matched to others based on propensity scores. |
| Free of other bias? | no | Intervention and control groups differed significantly at baseline (randomizations by shelter failed to eliminate bias adequately). Propensity scores were used to adjust for differences at baseline prior to data analysis. While cluster randomizations was conducted, no control for cluster effect was reported and outcomes were reported as for randomizations at the individual level. Per protocol assessment reported (youth who rotated through other shelters were excluded from analysis). Intention to treat would have been preferred. Outcomes were presented for males and females separately. It is unclear whether this stratification was pre-specified or not. This study was significantly underpowered (And was designed as such as it would not have been feasible to have conducted a powered study). |
| Slesnick 2005 | ||
| Methods | Randomised controlled trial (start and end dates not reported) | |
| Participants | 124 substance-abusing adolescents (12–17 years age, 59% female, 52% enrolled in school) referred from one of two runaway shelters in New Mexico, USA after a runaway episode with a history of at least 10 days of substance use in preceding 90 days, fulfilling criteria for at least one DSM-IV psychoactive substance use disorder and living within 60 miles of the two runaway shelters through which they were recruited. In addition, a parent/surrogate willing to participate was an inclusion criteria. Potential participants whose primary drug of abuse was alcohol were excluded, as were participants with unremitting psychosis or adolescents with no option to return to their home. The ethnicity of the participants were: Anglo (n=46), African American (n=9), Hispanic (n=51), native American (n=5) and other (n=13). HIV status of participants were not reported. Sexual orientation of participants were not reported. The HIV status of participants was not assessed/reported. | |
| Interventions | Intervention:Ecologically based family therapy (EBFT) (n=65) Control: Treatment/service as usual (n=59) Adolescents in both the intervention and control arm were free to obtain outside treatment. Theoretical underpinnings of intervention: This intervention was based on the homebuilders family preservation model based on crisis intervention theory (families are most open to change when in a crisis). A multisystemic treatment approach as per the multisystemic treatment model (behavioral problems in runaway youth are multiply determined and best addressed by multiple layers of interventions) was adopted here i.e.. approaching adolescents and parents individually first, then together, then approaching the extended family and involving other key role -players in the life of the adolescents. Techniques including cognitive-behavioural therapy and behavioural family therapy were used. Delivery, dosage and content of intervention Intervention was delivered in four phases over 15 sessions by therapists trained in behavioural, cognitive and environmental interventions. Four sessions focusing specifically on HIV prevention were incorporated in the first phase of intervention when the individual adolescent was engaged. The number of sessions in each phase of intervention and the detailed content were not reported but could be grouped into four phases:
Details on control Treatment as usual consisted housing the adolescent in the runaway shelter. Adolescents were housed in the shelter for a short time average of nine days SD 17.5 days and pretreatment assessment and 14 days at post-treatment assessment. Shelter provided for youth needs i.e. food, shelter, clothing, crises intervention and assistance with placements. |
|
| Outcomes | HIV risk behaviour’s as composite score out of 7 assessed by self-report behaviours (in a 3 hour diagnostic battery of self-report forms) at baseline, 3-, 6- and 12-months-post-intervention. The HIV risk behaviour score was calculated based on self report answers to seven questions on risk behavior in the preceding three months:
|
|
| Notes | Outcomes were not reported by arm in published reports. We obtained data from the authors for intent-to treat analysis. | |
| Risk of bias table | ||
| Item | Judgement | Description |
| Adequate sequence generation? | Yes | Urn Randomization used. |
| Allocation concealment? | Unclear | Insufficient information: following completion of the assessment battery all youth were randomised to intervention or control. |
| Blinding? | No | Unblinded study (participants and personnel not blinded). Outcome assessors (participants self-reporting sexual risk behavior) not blinded. |
| Incomplete outcome data addressed? | No | Differential and large loss to follow up (12/65 in intervention vs 15/59 in control). |
| Free of selective reporting? | No | Risk behavior outcomes reported as composite scores for all individuals by gender/ethnicity/period of assessment and not by treatment arm in published report. |
| Free of other bias? | No | A large proportion of participants did not complete the intervention. |
| Slesnick 2008 | ||
| Methods | Randomised controlled trial (November 2001-August 2005) | |
| Participants | 180 homeless adolescents (as per DHHS definition), (14–22 years age, 34% female) attending a drop-in centre for homeless youth in a southwestern city in USA, who met criteria for at least one DSM-IV diagnoses of alcohol or psychoactive substance use disorder and lived in the area of the study for the preceding three months with intention to stay in that area for subsequent six months. The ethnicity of participants were: Anglo (n=73), African American (n=6), Asian (n=1), Hispanic (n=54), native American (n=24), and other or mixed (n=22). HIV status of participants were not reported. Participants self identified their sexual orientation as heterosexual (n=147), homosexual (n=4) and bisexual (n=29). Forty-nine percent of participants had a DSM-IV axis one diagnosis other than substance abuse or dependence. The HIV status of participants was not assessed/reported. | |
| Interventions | Intervention: Integrated community reinforcement approach (CRA) (a cognitive-behavioral approach) and HIV prevention messaging (n=96) Control: Treatment/service as usual (n=84) Theoretical underpinnings of intervention: The CRA approach is based on an integrated cognitive-behavioural approach that included skills building to foster self-efficacy in the practice of preventative behaviours. The HIV prevention intervention was based on an intervention (Becoming a Responsible Teen B.A.R.T) covering AIDS education and assessment of risk, risk reduction and skills practice, sexual assertiveness and practicing negotiation as well as behavioral self-management and problem-solving strategies. Delivery, dosage and content of intervention Intervention consisted an integrated set of 12 CRA sessions and four HIV prevention sessions. each session lasted about 50 minutes. The HIV sessions were delivered after the 2nd CRA session, where convenient the HIV sessions were scheduled in the same week as the CRA session. The CRA sessions were delivered by trained therapists as follows, and incorporated role plays and homework :
The HIV prevention sessions and their content is as follows, and incorporated role-plays:
All sessions include role play. Details on control Treatment as usual consisted the standard extant care at a homeless persons drop-in centre including a place to rest during the day, food, showers clothing and case management that linked youth with community resources at the youth’s request. |
|
| Outcomes | HIV risk behaviour assessed at baseline, 3- and 6-month post intervention, as composite score of high-risk behaviours (out of 7),
Outcomes obtainable from authors and eligible for inclusion in this review were: number of participants having sexual intercourse, and the frequency of condom use. |
|
| Notes | ||
| Risk of bias table | ||
| Item | Judgement | Description |
| Adequate sequence generation? | Yes | Urn randomisation |
| Allocation concealment? | Yes | Central randomisation by project director communicated to personnel enrolling participant |
| Blinding? | No | Unblinded study |
| Incomplete outcome data addressed? | No | Significant and differential loss to follow up in two arms at both 3 month (31/96 in intervention and 17/84 in control arms) and 6 month (15/96 in intervention and 10/84 in control arms) assessment |
| Free of other bias? | No | Only 6.8/16 sessions attended by participants on average. A social networking intervention was concurrent with this trial in the same population-it is unclear in what direction this would have biased the results and whether the concurrent intervention may have been differentially affected the two trial arms. |
Three randomised controlled trials meeting the eligibility criteria for this review are included in this review:
Street Smart, n=311 youth 11–18 years (Rotheram-Borus 2003);
Ecologically Based Family Therapy (EBFT), n=124 youth 12–17 years (Slesnick 2005);
Community Reinforcement Approach and HIV prevention (CRA), n=180 youth 14–22 years (Slesnick 2008);
All three trials were performed in the United States of America and recruited substance-abusing male and female adolescents through runaway shelters into randomised controlled trials of independent and non-overlapping behavioural interventions. In all three trials, youth participants (or shelters in the case of one cluster-randomised trial, Rotheram-Borus 2003) were randomised to an intervention or a comparison control group that received the standard of care at that trial site at that time.
The three trials differed in theoretical background, delivery method, dosage (number of sessions,) content and outcome assessments. Additionally each differed in target group: one study targeted the individual, one targeted homeless youth in small groups and one study targeted individuals in their family context. All three trials included self-reported measures of sexual risk behaviour as outcomes but did not include any biological (primary outcome) measures of HIV/STI prevalence or incidence (not reported either at baseline or at intervention assessment). While each trial included HIV prevention messaging, the primary outcomes for each trial included other non sexual-risk behavior related measures of substance use, HIV knowledge, psychological/ individual functioning and family functioning. These additional outcomes are not included in this review.
We also identified three eligible ongoing studies, shown in the table: Characteristics of ongoing studies. The three studies test three different interventions in populations including or exclusively comprised of homeless youth and are being conducted in the United States of America. One trial (STRIVE 2004–9) has been completed but data were not available for inclusion in this review. The other two trials are due to be completed in 2011(Nyamathi 2008–11) and 2014 (Nyamathi 2009–14). None of the trials measure HIV incidence as an outcome but do measure baseline HIV prevalence (Nyamathi 2009–14) or HIV-risk behavior (Nyamathi 2008–11, STRIVE 2004–9).
Characteristics of ongoing studies
| Nyamathi 2008–11 | |
| Study name | An Arts Intervention for Drug-Using Homeless Youth |
| Methods | Open-label randomised control trial |
| Participants | 128 male and female unsheltered homeless substance-using youth 15–24 years of age recruited from Common Ground, Santa Monica, California, USA |
| Interventions | Experimental: Art Messaging: Experimental educational group which utilizes art, photography, film, painting to portray a message to reduce drug use, and prevent hepatitis A, B, & C delivered in four sessions. Control: Health Promotion education offering basic information about the prevention of hepatitis A, B & C delivered in four sessions. |
| Outcomes | Acceptability of the LIFE-MATTERS program, and impact in a subsample of the population (completion of the program; reduction of risky drug and alcohol use; completion of a HAV/HBV vaccine series; and improvement in knowledge about hepatitis).[Time Frame:2 years] |
| Starting date | April 2008 |
| Contact information | Contact: Adeline Nyamathi, PhD: 310-825-8405; anyamath@sonnet.ucla.edu OR Mary Marfisee, MD: 310-319-4700; mmarfisee@mednet.ucla.edu |
| Notes | Personal communication with principal investigator suggests that HIV risk behaviour measures are included in this trial. Due to reach completion in March 2011. |
| Nyamathi 2009–14 | |
| Study name | Hepatitis B Virus (HBV) Prevention for Homeless at Risk for HBV/Hepatitis C Virus (HCV)/HIV |
| Methods | Open-label randomised control trial |
| Participants | 500 homeless gay or bisexual men 18–39 years of age at Friends community centre, Los Angeles, California, USA |
| Interventions | Experimental: Nurse Case Management Plus Contingency Management and Tracking and the HBV vaccine vs Active Control: Standard with Contingency Management and Tracking (SCMT) and HBV vaccine |
| Outcomes | Primary Outcome Measures: Compare the NCMIT and SCMT programs among homeless young gay and bisexual stimulant using men with respect to completion of a HBV vaccination series administered in three doses over a four-month period. [Time Frame:5 years] Secondary Outcome Measures: Document the occurrences of HCV and HIV infections at baseline among these homeless HBV antibody negative stimulant users, and the factors associated with these infections at baseline. [Time Frame:5 years] |
| Starting date | July 2009 |
| Contact information | Cathy Reback, PhD: 323-463-1601; reback@friendsresearch.org |
| Notes | Primary population is not youth, but may include youth. Due to reach completion in March 2014. |
| STRIVE 2004–9 | |
| Study name | Support To Reunite Involve and Value Each Other (STRIVE): Diverting Homeless Youth From Chronic Homelessness and Risk for HIV |
| Methods | Open-label, randomised controlled trial |
| Participants | 302 male and female homeless youth 12–17 years of age recruited through homeless shelters. Location not provided. |
| Interventions | Behavioral: STRIVE family intervention Adolescent and parent attend a 5-session family-oriented cognitive-behavioral intervention aimed at giving runaway youths and their parents the tools to effectively deal with conflict. |
| Outcomes | Primary Outcome Measures: Improved residential stability [Time Frame:Assessed up to 24 months] Secondary Outcome Measures: Reduced HIV risk behavior [Time Frame: Up to 24 months] |
| Starting date | September 2004 |
| Contact information | Norweeta Milburn, PhD, UCLA Center for Community Health, NMilburn@mednet.ucla.edu |
| Notes | Study completed June 2009, but data not yet available at time of review. |
Excluded studies
See characteristics of Excluded studies table.
Characteristics of excluded studies
| Study | Reason for exclusion |
|---|---|
| Arnold 2007 | Not a RCT: a cohort of 11 youth 12–15 years in a feasibility study of strengths based case management |
| Booth 1999 | Not a RCT: a cross-sectional sample of 244 street youth half of whom receive a peer-based intervention |
| Gleghorn 1997 | Not a RCT: pre- and post-assessment of an intervention in 1146 adolescents versus comparison populations |
| Jemmot 2005 | Population inappropriate (not homeless): RCT of HIV/STD risk-reduction in 682 adolescent girls |
| Kidder 2007 | Population inappropriate. RCT of access to housing among 630 homeless adults living with HIV/AIDs with appropriate outcome measures. Included individuals 18–24 (youth)but not analysed separately and not the primary population |
| Lightfoot 2007 | Population inappropriate (not homeless). RCT of Streetsmart intervention in 100 youth living with HIV in Uganda |
| Linn 2003 | Population inappropriate (not adolescents). ’comparison group clinical trial’ of a cognitive-behavioural therapy intervention (SexG) in homeless mentally ill men |
| Nyamathi 2001 | Population inappropriate (not adolescents). A cluster randomised trial of three cognitive-behavioural HIV risk-reduction in homeless woman (18–50 years) |
| Rotheram-Borus 2009 | Population inappropriate (few adolescents). An RCT of 936 adults (including 7 participants 15–24 years) of healthy living program vs control for reducing risky sexual behavior |
| Susser 1998 | Population inappropriate (few adolescents). An RCT of a 15 session experimental vs 2-session control intervention in 97 mentally ill homeless men |
We excluded a total of 10 studies (detailed in 11 reports) which were of potential relevance but due either to ineligible study design (four studies: Arnold 2007; Booth 1999; Clements 1996/Gleghorn 1997) or ineligible study participants (six studies: Kidder 2007, Lightfoot 2007 ; Rotheram-Borus 2009; Jemmot 2005; Nyamathi 2001; Susser 1998; Linn 2003) were ineligible for inclusion.
Risk of bias in included studies
See Risk of bias in included studies.
In general, the included studies had significant risk of bias (see Figure 2, Figure 3).
Figure 2.
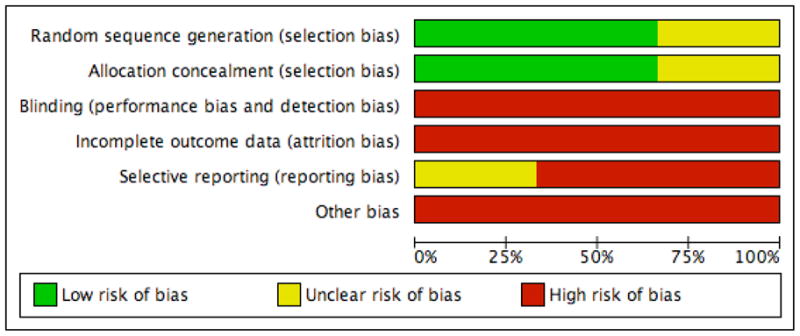
Risk of bias graphically presented by study
Figure 3.
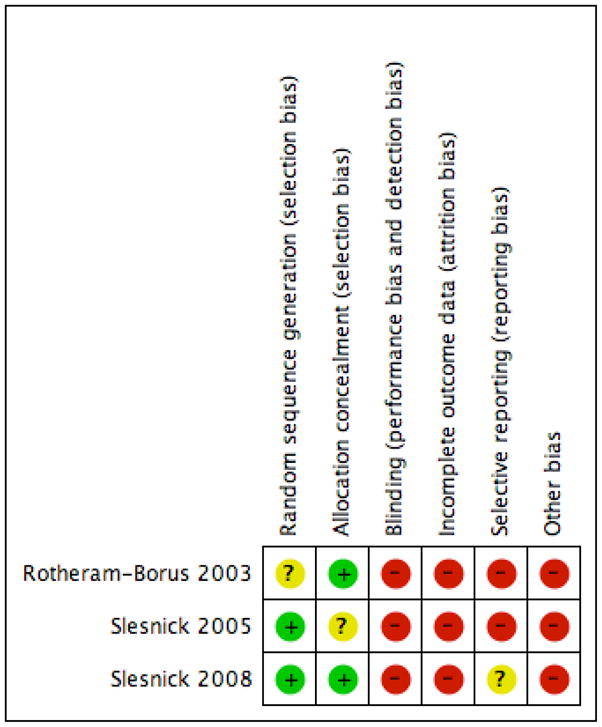
Summary: Risk of bias in included trials
All three trials have significant reporting (owing to incomplete outcome reporting) and attrition bias (owing to significant and differential follow-up rates in intervention and control arms). Furthermore the outcome assessment was performed by self report by unblinded participant, there is a significant, but arguably unavoidable, risk of detection bias.
The Streetsmart intervention had significant risk of selection and performance bias as, while it involved cluster randomizations, no adjustments for clustering/ intra-cluster correlations were reported and randomizations failed to ensure baseline similarity in exposures between intervention and control shelters (propensity scores were however used to try to achieve post-randomization baseline comparability for analysis). Additionally, the Street Smart intervention was not adequately powered for the outcomes of interest.
Effects of interventions
Due to the heterogeneity and non-traditional types of and reporting of outcomes, we were unable to calculate individual effect measures for outcomes and unable to estimate summary measures of effect. Further, the variability in intervention type precludes meta-analysis. Thus we present descriptive information for each trial.
None of the included trials reported protocol-specified primary outcomes of this review. In the Street Smart trial, three sexual behaviour outcomes were assessed at 3-,6- 12-,18- and 24- months post intervention and reported separately and (graphically only) for males and females (not clearly prespecified) after adjustment for baseline differences by the use of propensity scores (but not for intra-cluster correlation). The outcomes assessed were the total number of sexual partners, the number of unprotected sex acts and abstinence from vaginal or anal sex. We were unable to obtain data to calculate effect sizes or convert reported outcomes to standard outcome measures (RR or weighted mean difference with 95% confidence intervals) for reported outcomes. Based on reported outcomes in female participants, changes were reported for the number of sexual partners at 24 months (geometric mean number of sex acts in intervention 0.68 times that in control participants, 90% CI 0.47–0.98, p<0.10), the frequency of unprotected sexual acts at 3 months (geometric mean frequency of unprotected sexual acts in intervention 0.29 times that in control participants, 90% CI 0.10–0.83, p<0.10) and 24 months (geometric mean frequency of unprotected sexual acts in intervention 0.35 times that in control participants, 90% CI 0.17–0.71, p<0.05) and abstinence from unprotected vaginal and anal sex at 18 months (odds of being abstinent in the intervention 2.41 times that in control participants, 90% CI 1.04–5.58, p<0.10). In male participants, no significant effects for any of the sexual behaviour outcomes were reported at any timepoint.
In the EBFT trial, three sexual behaviour outcomes were assessed at 3-,6- and 12-months post intervention. The outcomes assessed were an index of risk based on seven questions (see included studies table), reported condom use and anal sex. No significant effects on sexual behaviour outcomes assessed were reported. Participants in this trial reported relatively low HIV risk behaviours (summarised as approximately 1.4 out of seven for both intervention and control groups on the HIV risk behaviour scale employed).
In the trial of CRA, three sexual behaviour outcomes were assessed at 3- and 6- months post intake. The outcomes assessed were the number of different sexual partners within a 24 hour period and within the last 3 months, and the frequency of condom use. Effects on condom use were reported using a numeric mean of self-reported condom use measured on a Lickert scale (scale: 1 to 5) in sub-analyses by age group (higher in intervention vs. control participants).
Discussion
Summary of main results
This review highlights the paucity of well-conducted randomised controlled trials of interventions to modify sexual risk behaviour for preventing HIV in homeless youth. We found three trials fulfilling the eligibility criteria for this review, but were unable to estimate a summary of effect measure for any of the outcomes for this review due to variability in outcomes assessed and intervention type. None of the three included trials measured or report biological (primary) outcomes. The limitations in the trials preclude assessment of their impact on modifying sexual risk behaviour. Nonetheless there are several studies in progress (see Characteristics of ongoing studies) that may add evidence to this critical area.
Overall completeness and applicability of evidence
We included three trials in this review enrolling a total N=615 participants; the paucity of trials is not compensated for by the sample size of the trials. While the participants included were youth, they were limited to urban youth residing in American cities; these may not be applicable to other types of homeless youth, or homeless youth living under different conditions and with different exposures. The interventions tested represent a small sample of the variety of behaviour-change interventions that have been evaluated for HIV (Padian 2010) or other conditions (Fisher 2000). Finally, while the trials included here assessed some outcomes relevant to sexual risk behaviours, none assessed or reported biological markers of sexual risk behaviour (pregnancy/STI’s or HIV acquisition). Similarly, the trials included did not assess or report measures of sexual risk behaviour consistently making it inappropriate to pool data for summary measures of effect.
The studies identified in this review are inadequate to permit evaluation and summary of the effectiveness of interventions for modifying sexual risk behaviours for preventing HIV in homeless youth.
Quality of the evidence
The body of evidence identified does not permit robust conclusions on the impact of interventions to modify sexual risk behaviour in homeless youth. We assessed these studies to be of low quality (per the GRADE approach) and to have high risk of bias in view of limitations in design and implementation, imprecision of results, and high probability of reporting, attrition, detection, selection and performance bias.
Potential biases in the review process
This review is robust to quality of design and conduct of studies. We chose to include studies which did not report on the outcomes of interest and were able to obtain these data from authors. Since study quality was not an eligibility criterion, this study is also unlikely to exclude studies based on quality measures.
The major limitation in this review is the inability to estimate summary effect measures or to report on primary outcomes of sexual behaviour change; the trials included reported self-reported behaviours only.
Agreements and disagreements with other studies or reviews
This review is not the first review of interventions to modify sexual risk behaviour in homeless youth, however its systematic approach differentiates it from three narrative reviews that include the subject (Arnold 2009; Badiaga 2008; Crane 1992) and account for the differences in study inclusion, results and conclusions. In Arnold and Rotheram-Borus’ recent review of prevention programs for homeless youth (Arnold 2009), they included six HIV prevention studies (three of which are included in this review, two are excluded due to design-Gleghorn 1997; Arnold 2007, and one included though ongoing) and assessed each study by a framework they had previously developed in order to summarise the robust components of interventions for homeless youth. From the evidence assembled in this review, the basis for conclusions on robust elements is weak as there is scant evidence of successful interventions to modify sexual risk behaviour for preventing HIV in homeless youth. In Badiaga and colleagues’ review of transmissible diseases in homeless of any age (Badiaga 2008), they review the rationale for interventions to prevent HIV, and highlight one intervention targeting homeless youth (Rotheram-Borus 2003) that is included in this systematic review. Crane and Carswell in their early review (Crane 1992), reviewed non-governmental organization-based prevention projects aimed at prevention of sexually-transmitted infections and HIV in street children. They report on several NGO-based non-randomised controlled interventions that provide service to homeless children. This review did not distinguish between the type of organization that performed the prevention project but aimed to assemble the evidence for interventions to modify sexual risk behavior in homeless youth that have been rigorously evaluated.
In addition to narrative reviews that have focused on homeless youth, there have been several systematic reviews and meta-analyses of behavioral interventions to reduce HIV-related sexual risk behaviour in defined populations excluding homeless youth (reviewed in Noar 2008). These include systematic reviews and meta-analysis of behavioral interventions to prevent HIV in adolescents (Mullen 2002, Johnson 2003), substance abusing individuals (Prendergast 2001, Semaan 2002 and Copenhaver 2006), and individuals with severe mental illness (Johnson-Masotti 2003). Importantly, these reviews highlight the feasibility of bringing about behaviour change. Hence, these reviews enable assessment of what factors characterise effective interventions (see Noar 2008) in populations that share similar characteristics (high rates of substance abuse, mental illness and being adolescents) to homeless youth: such as having a separate approach to participants of different race and gender, including skills-training and having a theory-based component to interventions. These characteristics may also prove to be important moderators of effectiveness in modifying sexual risk behavior for preventing HIV in homeless youth, but this systematic review is unable to draw conclusions in this regard.
But sexual risk behaviour, particularly when assessed by self-report, is an imperfect correlate of HIV incidence. This underscores the need for HIV prevention efforts to be evaluated in trials with HIV incidence as a directly measured outcome, at least where possible and until we have superior proxy measures for HIV risk. How to prevent HIV remains a major challenge not just in homeless youth but in general; of 37 randomised controlled trials with HIV incidence as the primary or secondary outcome, only 5 trials-three of circumcision(Auvert 2005, Bailey 2007, Gray 2007), one of STI treatment and care(Grosskurth 1995), and one vaccine trial(Rerks-Ngarm 2009)- have shown any positive effect (none were behavioural interventions) (Padian 2010). In addition, only three HIV prevention trials with HIV incidence as an outcome have been performed in adolescents (Ross 2007, Cowan 2008, Jewkes 2008,), and none have shown any effect thus far. Nonetheless, Padian and colleagues in their review state that “ lack of statistical power, poor adherence, and diluted versions of the intervention in comparison groups may have been important issues for the other trials that demonstrated ‘flat’ results”. Similarly, we believe that the lack of effective trials reported in this review need to be seen not just in the light of the unique challenges of working with homeless youth, but also the challenge of conducting robust clinical trials.
Authors’ conclusions
Implications for practice
The body of evidence from this systematic review limits robust conclusions on implications for practice. The reported success of the interventions in bringing forth some level of change in risk behavior i.e. a decrease in number of sexual partners and or unprotected sex acts should be viewed with caution. The unintended outcomes of the trials namely to retain sufficient participants for post intervention measures among this very mobile population, in particular for a 24 month period as reported in the Street Smart trial, might be a viewed as a significant outcome that is likely to facilitate other health promoting behavioural change. We believe that the CDC’s current policy (C:\Users\caprisa\AppData\Local\Microsoft\Windows\Temporary Internet Files\Content.Outlook\HCPXEC3U\DEBI Factsheet 08\09) of supporting the Street Smart approach may need re-examination in view of teh body of evidence presented here. More research is required before practice may be changed based on proven interventions in homeless youth.
Implications for research
This review highlights the high HIV risk in this population and paradoxical paucity of robust randomised controlled trials to evaluate the effectiveness of HIV prevention programmes among homeless youth and underscores an urgent need for more updated risk factor analysis to inform design and implementation of future trials targeting this population (Cohen 2010). Coupled with the growing rates of homelessness amongst orphaned youth in AIDS endemic regions, the UNAIDS mantra of ‘know your epidemic’ underscores the importance of continued research to monitor homeless youth and their HIV risk and prevalence so that tailored interventions may be robustly evaluated. While the psychosocial and contextual factors that fuel sexual risk behaviours among homeless youth challenge the stringent methodologies of RCT’s, novel interventions (e.g.. cash transfers or social security interventions, (The World Bank 2010)) and ways for program delivery and trial retention are in need of further development. Strategies to increase retention may include alternative ways of compensating for visits or increasing financia compensation. Future trials should endeavour to comply with rigorous methodology in design, delivery, measurement of risk behaviours and reporting. Using outcome measures that are common across clinical trials may permit fair comparison of various interventions in different populations, and future studies should consider using outcomes based on a common set of standardized outcome measures (for example, indicators for monitoring and evaluating national HIV/AIDS prevention programmes for young people (WHO 2004)). In particular, self-report of risky sexual behavioural change should be supported by biological markers i.e. HIV or STI prevalence and incidence rates where possible as these are more direct measures of effectiveness of interventions to prevent HIV, and may be feasible given the high incidence of HIV amongst homeless youth. Responsibility to ensure that interventions studies are designed and conducted to the highest standard is balanced by reponsibility sponsoring agencies have to provide resources to conduct these types of studies. The results of three ongoing and potentially eligible studies will be a useful addition to this review.
Supplementary Material
Acknowledgments
We gratefully acknowledge the support of the staff of the South African Cochrane centre and the HIV/AIDS Review group. In particular we acknowledge the assistance of Joy Olivier and Tara Horvath in assisting with searches, Elizabeth Pienaar, Vicki Badenhorst and Babalwa Zani for their technical support and Nandi Siegfried for her mentorship and guidance during the conduct of this review. We thank Regina El Dib for her translations of the non-English titled abstracts from LILACS for this review.
Funding: VN is supported through a fellowship jointly funded by LIFELab, a South African Department of Science and Technology platform, and the Columbia University-South Africa Fogarty AITRP
Financial support for CAPRISA from the National Institute of Allergy and infectious Disease (NIAID), National Institutes of Health (NIH) (grant# AI51794) is gratefully acknowledged.
Footnotes
Declarations of interest
None.
Differences between protocol and review
We modified the age of participants for eligible trials from 15-24 years(inclusive) to 12-24 years (inclusive).
Contributions of authors
VN designed and coordinated the conduct of this review.
VN and AM performed the data collection, abstraction and entry for the review with the assistance of the South African Cochrane centre and were responsible for the writing of this review.
QAK and NS secured funding for the review, provided general advice for the review and a methodological perspective, and critically read and appraised the final review.
References to studies
Included studies
- Rotheram-Borus 2003, Published data only (unpublished sought but not used).Rotheram-Borus MJ, Song J, Gwadz M, Lee M, Van Rossem R, Koopman C. Reduction in HIV risk among runaway youth. Prevention science. 2003;4(3):173–87. doi: 10.1023/a:1024697706033. [DOI] [PubMed] [Google Scholar]
- Slesnick 2005, Published and unpublished data.Slesnick N, Prestopnik JL. Ecologically based family therapy outcome with substance abusing runaway adolescents. Journal of Adolescence. 2005;28:277–98. doi: 10.1016/j.adolescence.2005.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slesnick 2008, Published and unpublished data.Slesnick N, Kang M. HIV risk reduction among substance-abusing. Proceedings of the 69th Annual Scientific Meeting of the College on Problems of Durg Dependence; June 16–21 2007; Quebec City, Canada. [Google Scholar]; * Slesnick N, Kang MJ. The impact of an integrated treatment on HIV risk behavior among homeless youth: a randomized controlled trial. Journal of behavioural medicine. 2008 Feb;31(1):45–59. doi: 10.1007/s10865-007-9132-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Excluded studies
- Arnold 2007.Arnold EM, Walsh AK, Oldham MS, Rapp CA. strengths-based case management: implementation with high-risk youth. Families in society: the journal of contemporary social services. 2007;88(1):86–94. [Google Scholar]
- Booth 1999.Booth RE, Zhang Y, Kwiatkwski CF. the challenge of changing drug and sex risk behaviors of runaway and homeless adolescents. Child abuse and neglect. 1999;23(12):1295–306. doi: 10.1016/s0145-2134(99)00090-3. [DOI] [PubMed] [Google Scholar]
- Gleghorn 1997.Clements KD, Gleghorn AA, Garcia D, Sabin M, Katz M. Can street outreach effectively reach a mobile population of homeless youth?. Proceedings of International Conference on AIDS; 1996. p. 51. [Google Scholar]; Gleghorn AA, Clements KD, Marx R, Vittinghoff E, Leee-Chu P, Katz M. The impact of intensive outreach on HIV prevention activities of homeless, runaway and street youth in San Francisco: the AIDS evaluation of street outreach project (AESOP) IDS and behaviour. 1997;1(4):261–71. [Google Scholar]
- Jemmot 2005, Published and unpublished data.Jemmott JB, Jemmott LS, Braverman PK, Fong GT. HIV/STD reduction interventions for african american and latino adolescent girls at an adolescent medicine clinic: a randomized controlled trial. Archives of pediatrics and adolescent medicine. 2005;159(4):440–9. doi: 10.1001/archpedi.159.5.440. [DOI] [PubMed] [Google Scholar]
- Kidder 2007, Published and unpublished data.Kidder DP, Wolitski RJ, Royal S, Aidala A, Courtenay-Quirk C, Holtgrave DR. Access to housing as a structural intervention for homeless and unstably housed people living with HIV: rationale, methods, and implementation of the housing and health study. IDS and Behavior. 2007;11(Suppl 2):S149–161. doi: 10.1007/s10461-007-9249-0. [DOI] [PubMed] [Google Scholar]
- Lightfoot 2007.Lightfoot MA, Kasirye R, Comulada WS, Rotheram-Borus MJ. Efficacy of a culturally adapted intervention for youth living with HIV in Uganda. Prevention Science. 2007;8(4):271–3. doi: 10.1007/s11121-007-0074-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linn 2003, Published data only (unpublished sought but not used).Linn LG, Neff JA, Theriot R, Harris JL, Interante J, Graham ME. Reaching impaired populations with HIV prevention programs: a clinical trial for homeless mentally ill african-american men. Cell and Molecular Biology. 2003;49(7):1167–75. [PubMed] [Google Scholar]
- Nyamathi 2001, Published and unpublished data.Nyamathi A, Flaskerud JH, Leake B, Dixon EL, Lu A. Evaluating the impact of peer, nurse case-managed, and standard HIV risk-reduction programs on psychosocial and health-promoting behavioral outcomes among homeless women. Research in Nursing and Health. 2001;24(5):410–22. doi: 10.1002/nur.1041. [DOI] [PubMed] [Google Scholar]
- Rotheram-Borus 2009, Published and unpublished data.Rotheram-Borus MJ, Desmond K, Comulada WS, Arnold EM, Johnson M. Reducing risky sexual behavior and substance use among currently and formerly homeless adults living with HIV. American Journal of Public Health. 2009;99(6):1100–7. doi: 10.2105/AJPH.2007.121186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Susser 1998, Published and unpublished data.Susser E, Valenci E, Berkman A, Sohler N, Conover S, Torres J, et al. Human immunodeficiency virus sexual risk reduction in homeless men with mental illness. Archive of Internal Medicine. 1998;158(5):266–72. doi: 10.1001/archpsyc.55.3.266. [DOI] [PubMed] [Google Scholar]
Studies awaiting classification
Ongoing studies
- Nyamathi 2008–11, Unpublished data only [ClinicalTrials.gov: NCT00862238].Nyamathi A and colleagues. University of California Los Angeles. An Arts Intervention for Drug-Using Homeless Youth. www.clinicaltrials.gov.
- Nyamathi 2009–14, Unpublished data only [ClinicalTrials.gov: NCT00926146].Nyamathi A and colleagues, University of California, Los Angeles. Hepatitis B Virus (HBV) Prevention for Homeless at Risk for HBV/Hepatitis C Virus (HCV)/HIV. www.clinicaltrials.gov.
- STRIVE 2004–9, Unpublished data only [ClinicalTrials.gov: NCT00996541].Milburn N and colleagues. Support To Reunite Involve and Value Each Other (STRIVE) University of California, Los Angeles, Center for Community Health; www.clinicaltrials.gov. [Google Scholar]
Other references
Additional references
- Anarfi 1997.Anarfi JK. Vulnerability to sexually transmitted disease: street children in Accra. Health Transition Review. 1997;7(Suppl):281–306. [PubMed] [Google Scholar]
- Arnold 2009.Arnold EM, Rotheram-Borus MJ. Comparisons of prevention programs for homeless youth. Prevention Science. 2009;10:76–86. doi: 10.1007/s11121-008-0119-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Auvert 2005.Auvert B, Taljaard D, Lagarde E, Sobngwi-Tambekou J, Sitta R, Puren A. Randomized, controlled intervention trial of male circumcision for reduction of HIV infection risk: the ANRS 1265 trial. PLoS Med. 2005 Nov 2;2(11):e298. doi: 10.1371/journal.pmed.0020298. EPub 2005 Oct 25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Badiaga 2008.Badiaga S, Raoult D, Brouqui P. Preventing and controlling emerging and reemerging transmissible diseases in the homeless. Emerging infectious diseases. 2008 Sep 9;14(9):1353–9. doi: 10.3201/eid1409.082042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bailey 2007.Bailey RC, Moses S, Parker CB, Agot K, Maclean I, Krieger JN, Williams CF, Campbell RT, Ndinya-Achola JO. Male circumcision for HIV prevention in young men in Kisumu, Kenya: a randomised controlled trial. Lancet. 2007 Feb 24;369(9562):643–56. doi: 10.1016/S0140-6736(07)60312-2. [DOI] [PubMed] [Google Scholar]
- Barker 1993.Barker G. Research on AIDS: knowledge, attitudes and practices among street youth. Children Worldwide. 1993;20(2–3):41–2. [PubMed] [Google Scholar]
- Baybuga 2004.Baybuga MS, Celik SS. The level of knowledge and views of the street children/youth about AIDS in Turkey. Internation journal of nursing studies. 2004;41(6):591–7. doi: 10.1016/j.ijnurstu.2003.12.010. [DOI] [PubMed] [Google Scholar]
- Bernier 1995.Bernier M, Ascensio P. [Street children and AIDS in Haiti] Sante. 1995;5(2):125–30. [PubMed] [Google Scholar]
- Black 1997a.Black B, Farrington AP. Preventing HIV / AIDS by promoting life for Indonesian street children. Aidscaptions. 1997;4(1):14–7. [PubMed] [Google Scholar]
- Black 19997b.Black B, Farrington AP. Promoting life for Indonesia’s street children. AIDSlink. 45:10–1. [PubMed] [Google Scholar]
- Boivin 2005.Boivin JF, Roy E, Haley N, Galbaud du Fort G. The health of street youth: a Canadian perspective. Canadian journal of public health. 2005;96(6):432–7. doi: 10.1007/BF03405183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cauce 2000.Cauce A, Paradise M, Ginzler J, Embry L, Morgan C, Lohr Y. The characteristics of mental health of homeless adolescents: age and gender differences. Journal of Emotional and Behavioural Disorders. 2000;8(4):230–9. [Google Scholar]
- Chinazo 2007.Chinazo O, Cunningham MD, Sanches JP, Heller DI, Sohler NL. Assessment of a medical outreach program to improve access to HIV care among marginalized individuals. American Journal of Public Health. 2007;97(10):1758–61. doi: 10.2105/AJPH.2006.090878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clements 1997.Clements K, Gleghorn A, Garcia D, Katz M, Marx R. A risk profile of street youth in northern California: implications for gender-specific human immunodeficiency virus prevention. Journal of Adolescent Health. 1997;20(5):343–53. doi: 10.1016/S1054-139X(97)00033-5. [DOI] [PubMed] [Google Scholar]
- Cohen 2010.Cohen J. HIV Moves In on Homeless Youth. Science. 2010 Jul 9;329(5988):170–1. doi: 10.1126/science.329.5988.170. [DOI] [PubMed] [Google Scholar]
- Copenhaver 2006.Copenhaver MM, Johnson BT, Lee I, Harman JJ, Carey MP. Behavioral HIV risk reduction among people who inject drugs: meta-analytic evidence of efficacy. Journal of substance abuse treatment. 2006;31:163–71. doi: 10.1016/j.jsat.2006.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cowan 2008.Cowan FM, Pascoe SL, Langhau LF, Dirawo J, Chidiya S, Jaffar S, Mbizvo M, Stephenson JM, Johnson AM, Power RM, Woelk G, Hayes RJ. The Regai Dzive Shiri project: a cluster randomised controlled trial to determine the effectiveness of a multicomponent community-based HIV prevention intervention for rural youth in Zimbabwe – study design and baseline results. Trop Med Int Health. 2008;13(10):1235–44. doi: 10.1111/j.1365-3156.2008.02137.x. [DOI] [PubMed] [Google Scholar]
- Crane 1992.Crane SF, Carswell JW. A review and assessment of non-governmental organization-based STI/AIDS education and prevention projects for marginalized groups. Health education research. 1992;7(2):175–94. doi: 10.1093/her/7.2.175. [DOI] [PubMed] [Google Scholar]
- de Carvalho 2006.de Carvalho FT, Neiva-Silva L, Ramos MC, Evans J, Koller SH, Piccinini CA, et al. Sexual and drug use risk behaviors among children and youth in street circumstances in Porto Alegre, Brazil. AIDS and behavior. 2006;10(4 Suppl):S57–66. doi: 10.1007/s10461-006-9124-4. [DOI] [PubMed] [Google Scholar]
- DEBI Factsheet 08/09. [accessed October 2010.];Diffusion of Effective Interventions Project. http://www.effectiveinterventions.org/en/home.aspx.
- DeMatteo 1999.DeMatteo D, Major C, Block B, Coates R, Fearon M, Goldberg E, et al. Toronto street youth and HIV/AIDS: prevalence, demographics, and risks. Journal of Adolescent Health. 1999;25(5):358–66. doi: 10.1016/s1054-139x(99)00059-2. [DOI] [PubMed] [Google Scholar]
- DiClemente 1995.DiClemente RJ, Wingood GM. A randomized controlled trial of an HIV sexual risk-reduction intervention for young African-American women. JAMA. 1995;274(16):1271–6. [PubMed] [Google Scholar]
- Doyle AM 2010.Doyle AM, Napierala MS, Ross DA. HIV prevention in young people in sub-Saharan Africa: a systematic review and update of the evidence (WEAC0201). XVIII International AIDS Conference (AIDS 2010); Vienna, Austria. 2010. [Google Scholar]
- Fisher 2000.Fisher JD, Fisher WA. Theoretical approached to individual-level change in HIV risk behavior. In: Peterson, DiClemente, editors. Handbook of HIV Prevention. New York: Kluwer Academic/Plenum; 2000. pp. 3–55. [Google Scholar]
- Gatu 2000.Gatu R. Solomon Islands: reaching street children in Honiara. Pac AIDS Alert Bull Pacific AIDS alert bulletin. 2000;19:11. [PubMed] [Google Scholar]
- Gleghorn 1998.Gleghorn A, Marx R, Vittinghoff E, Katz M. Association between drug use patterns and HIV risk among homeless, runaway, and street youth in Northern California. Drug and Alcohol Dependence. 1998;51:219–27. doi: 10.1016/s0376-8716(98)00042-8. [DOI] [PubMed] [Google Scholar]
- Gray 2007.Gray RH, Kigozi G, Serwadda D, Makumbi F, Watya S, Nalugoda F, Kiwanuka N, Moulton LH, Chaudhary MA, Chen MZ, Sewankambo NK, Wabwire-Mangen F, Bacon MC, Williams CF, Opendi P, Reynolds SJ, Laeyendecker O, Quinn TC, Wawer MJ. Male circumcision for HIV prevention in men in Rakai, Uganda: a randomised trial. Lancet. 2007 Feb 24;369(9562):657–66. doi: 10.1016/S0140-6736(07)60313-4. [DOI] [PubMed] [Google Scholar]
- Greene 1997.Greene J, Ringwalt C, Iachan R. Shelters for runaway and homeless youths: Capacity and occupancy. Child Welfare. 1997;76:549–561. [PubMed] [Google Scholar]
- Greene 1999.Greene JM, Ennett ST, Ringwalt CL. Prevalence and correlates of survival sex among runaway and homeless youth. American journal of public health. 1999;89(9):1406–9. doi: 10.2105/ajph.89.9.1406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grosskurth 1995.Grosskurth H, Todd J, Mwijarubi E, Mayaund P, ka-Gina G, Mabey D, Hayes R, Mosah F, Senkoro K, Changalucha J, Klokke A, Mugeye K. Impact of improved treatment of sexually transmitted diseases on HIV infection in rural Tanzania: randomised controlled trial. The Lancet. 1995 Aug 26;346(8974):530–6. doi: 10.1016/s0140-6736(95)91380-7. [DOI] [PubMed] [Google Scholar]
- Halcon 2004.Halcon L, Lifson A. Prevalence and predictors of sexual risks among homeless youth. Journal of youth and adolescence. 2004;33(1):71–80. [Google Scholar]
- Haley 2004.Haley N, Roy E, Leclerc P, Boudreau JF, Boivin JF. HIV risk profile of male street youth involved in survival sex. Sex Transm Infect. 2004;80(6):526–30. doi: 10.1136/sti.2004.010728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hammer 2002.Hammer H, Finkelhor D, Sedlak A. [accessed 8 Mar 2008];Runaway/ throwaway children: national estimates and characteristics. 2002 http://www.ncjrs.org/pdffiles1/ojjdp/196469.pdf.
- Jewkes 2008.Jewkes R, Nduna M, Levin J, Jama N, Dunkle K, Puren A, Duvvury N. Impact of stepping stones on incidence of HIV and HSV-2 and sexual behaviour in rural South Africa: cluster randomised controlled trial. BMJ. 2008;337:a506. doi: 10.1136/bmj.a506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson 2003.Johnson BT, Carey MP, Marsh KL, Levin KD, Scott-Shelfon LAJ. Interventions to reduce sexual risk for the human immunodeficiency virus in adolescents, 1985–2000: a research synthesis. Archives of pediatric and adolescent medicine. 2003;157:381–8. doi: 10.1001/archpedi.157.4.381. [DOI] [PubMed] [Google Scholar]
- Johnson-Masotti 2003.Johnson-Masotti AP, Weinhardt LS, Pinkerton SD, Otto-Salaj LL. Efficacy and cost-effectiveness of the first generation of HIV prevention interventions for people with severe mental illness. The journal of mental health policy and economics. 2003;6:23–35. [PubMed] [Google Scholar]
- Kegeles 1996.Kegeles SM, Hays RB, Coates TJ. The Mpowerment Project: a community-level HIV prevention intervention for young gay men. American journal of public health. 1996;86(8):1129–36. doi: 10.2105/ajph.86.8_pt_1.1129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly 2003.Kelly PJ, Grajcer B, Rigato FD. Children Living on the Street. Online Brazilian Journal of Nursing (OBJN_ISSN 1676–4285) [accessed 5 March 2008];Online Brazilian Journal of Nursing. 2003 2(2) www.uff.br/nepae/objn202kellyetal.htm. [Google Scholar]
- Kidd 2004.Kidd S, Scrimenti K. Evaluating child and youth homelessness. Evaluation review. 2004;28(4):325–41. doi: 10.1177/0193841X04264820. [DOI] [PubMed] [Google Scholar]
- Kipke 1995.Kipke MD, O’Connor S, Palmer R, MacKenzie RG. Street youth in Los Angeles: profile of a group at high risk for human immunodeficiency virus infection. Archives of Pediatric and Adolescent Medicine. 1995;149(5):513–9. doi: 10.1001/archpedi.1995.02170180043006. [DOI] [PubMed] [Google Scholar]
- Kissin 2007.Kissin DM, Zapata L, Yorick R, Vinogradova EN, Volkova GV, Cherkassova E, Lynch A, Leigh J, Jamieson DJ, Marchbanks PA, Hillis S. HIV seroprevalence in street youth, St Petersburg, Russia. AIDS. 2007;21:2333–40. doi: 10.1097/QAD.0b013e3282f125b3. [DOI] [PubMed] [Google Scholar]
- Klein 2000.Klein J, Woods A, Wilson K, Prospero M, Greene J, Ringwalt C. Homeless and runaway youth’s access to health care. Journal of Adolescent Health. 2000;27:331–9. doi: 10.1016/s1054-139x(00)00146-4. [DOI] [PubMed] [Google Scholar]
- Lambert 2005.Lambert M, Torrico F, Billot C, Mazina D, Marleen B, Van der Stuyft P. Street youths are the only high-risk group for HIV in a low-prevalence South American country. Sexually Transmitted Diseases. 2005;32(4):240–2. doi: 10.1097/01.olq.0000158493.89520.db. [DOI] [PubMed] [Google Scholar]
- Luna 1991.Luna GC. Street youth: adaptation and survival in the AIDS decade. Journal of adolescent health. 1991;12(7):511–4. doi: 10.1016/0197-0070(91)90079-2. [DOI] [PubMed] [Google Scholar]
- MacDonald 1994.MacDonald NE, Fisher WA, Wells GA, Doherty JA, Bowie WR. Canadian street youth: correlates of sexual risk-taking activity. Pediatr Infect Dis J The pediatric infectious disease journal. 1994;13(8):690–7. [PubMed] [Google Scholar]
- MacLean 1999.MacLean M, Embry L, Cauce A. Homeless adolescents’ paths to separation from family: Comparison of family characteristics, psychological adjustment, and victimization. Journal of Community Psychology. 1999;27(2):179–87. [Google Scholar]
- Malamud 1995.Malamud S. At risk and abandoned: street children, AIDS and human rights. AIDS link. 1995;31:6–7. [PubMed] [Google Scholar]
- Mantell 1997.Mantell JE, DiVittis AT, Aurbach MI. Evaluating HIV prevention interventions. New York: Plenum Press; 1997. [Google Scholar]
- Milburn 2007.Milburn NG, Stein JA, Rice E, Rotheram-Borus MJ, Mallett S, Rosenthal D, et al. AIDS Risk Behaviors among American and Australian Homeless Youth. Journal of Social Issues. 2007;63:543–65. [Google Scholar]
- Moore 2006.Moore J. [accessed 5 Mar 2008];Unaccompanied and homeless youth: review of the literature (1995–2005) 2006 http://www.cde.state.co.us/cdeprevention/download/pdf/Homeless%20Youth%20Review%20of%20Literature.pdf.
- Mullen 2002.Mullen PD, Ramirez G, Strouse D, Hedges LV, Sogolow E. Meta-analysis of the effects of behavioral HIV prevention interventions on the sexual risk behavior of sexual experienced adolescents in controlled studies in the United States. Journal of Acquired Immune Decificiency Syndromes. 2002;30:S94–105. [PubMed] [Google Scholar]
- Noar 2008.Noar SM. Behavioral Interventions to Reduce HIV-related Sexual Risk Behavior: Review and Synthesis of Meta-Analytic Evidence. AIDS and Behavior. 2008;12:335–353. doi: 10.1007/s10461-007-9313-9. [DOI] [PubMed] [Google Scholar]
- Ommundsen 1993.Ommundsen C. [Brazil: street children in the risk zone for HIV and AIDS] Vardfacket. 1993;17(13):24–5. [PubMed] [Google Scholar]
- Padian 2010.Padian NS, McCoy SI, Balkus JE, Wasserheit JN. Weighting the gold in the gold standard: challenges in HIV prevention research. AIDS. 2010;24:621–35. doi: 10.1097/QAD.0b013e328337798a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Panter-Brick 2002.Panter-Brick C. Street children, human rights, and public health: a critique and future directions. Annual Review of Anthropology. 2002;31(1):147–71. [Google Scholar]
- Pennbridge 1992.Pennbridge JN, Freese TE, MacKenzie RG. High-risk behaviors among male street youth in Hollywood, California. AIDS Educ Prev AIDS education and prevention. 1992 Fall;(Suppl):24–33. [PubMed] [Google Scholar]
- Podschun 1993.Podschun GD. Teen Peer Outreach-Street Work Project: HIV prevention education for runaway and homeless youth. Public health reports. 1993;108(2):150–5. [PMC free article] [PubMed] [Google Scholar]
- Poulin 2001.Poulin C, Alary M, Bernier F, Carbonneau D, Boily MC, Joly JR. Prevalence of Chlamydia trachomatis and Neisseria gonorrhoeae among at-risk women, young sex workers, and street youth attending community organizations in Quebec City, Canada. Sexually transmitted diseases. 2001;28(8):437–43. doi: 10.1097/00007435-200108000-00002. [DOI] [PubMed] [Google Scholar]
- Prendergast 2001.Prendergast ML, Urada D, Podus S. Meta-analysis of HIV risk-reduction interventions within drug abuse treatment programs. Journal of consulting and clinical psychology. 2001;69:389–405. doi: 10.1037//0022-006x.69.3.389. [DOI] [PubMed] [Google Scholar]
- Raffaelli 2003.Raffaelli M, Campos R, Merritt AP, Siqueira E, Antunes CM, Parker R, et al. Sexual practices and attitudes of street youth in Belo Horizonte, Brazil. Social science & medicine. 1993;37(5):661–70. doi: 10.1016/0277-9536(93)90105-d. [DOI] [PubMed] [Google Scholar]
- Raleigh-DuRoff 2004.Raleigh-DuRoff C. Factors that influence adolescents to leave or stay living on the street. Child and adolescent social work journal. 2004;21(6):561–72. [Google Scholar]
- Ramphele MA 1997.Ramphele MA. Adolescents and violence: “adults are cruel: “they just beat, beat, beat!”. Social Science & Medicine. 1997;45(8):1189–97. doi: 10.1016/s0277-9536(97)00025-7. [DOI] [PubMed] [Google Scholar]
- Rerks-Ngarm 2009.Rerks-Ngarm S, Pitisuttithum P, Nitayaphan S, Kaewkungwal J, Chiu J, Paris R, Premsri N, Namwat C, de Souza M, Adams E, Benenson M, Gurunathan S, Tartaglia J, McNeil JG, Francis DP, Stablein D, Birx DL, Chunsuttiwat S, Khamboonruang C, Thongcharoen P, Robb ML, Michael NL, Kunasol P, Kim JH MOPH-TAVEG Investigators. Vaccination with ALVAC and AIDSVAX to prevent HIV-1 infection in Thailand. N Engl J Med. 2009 Dec 3;361(23):2209–20. doi: 10.1056/NEJMoa0908492. [DOI] [PubMed] [Google Scholar]
- Rew 2001.Rew L, Taylor-Seehafer M, Thomas N, Yockey R. Correlates of resilience in homeless adolescents. Journal of Nursing Scholarship. 2001;33(1):33–40. doi: 10.1111/j.1547-5069.2001.00033.x. [DOI] [PubMed] [Google Scholar]
- Ribeiro 2001.Ribeiro M, Trench Ciampone M. Homeless children: The lives of a group of Brazilian street children. Journal of advanced nursing 2001: The lives of a group of Brazilian street children Journal of Advanced Nursing. 2001;35(42–49) doi: 10.1046/j.1365-2648.2001.01847.x. [DOI] [PubMed] [Google Scholar]
- Richter 1995.Richter LM, Swart-kruger J. AIDS-risk among street children and youth: implications for intervention. South african journal of psychology. 1995;25(1):31–8. doi: 10.1177/008124639502500105. [DOI] [PubMed] [Google Scholar]
- Ringwalt 1998.Ringwalt C, Greene J, Robertson M. Familial backgrounds and risk behaviours of youth with throwaway experiences. Journal of Adolescence. 1998;21:241–52. doi: 10.1006/jado.1998.0150. [DOI] [PubMed] [Google Scholar]
- Robbins 2010.Robbins CL, Zapata L, Kissin DM, Shevchenko N, Yorick R, Skipalska H, Finnerty E, Ornstein T, Marchbanks PA, Jamieson DJ, Hillis SD. Multicity HIV seroprevalence in street youth, Ukraines. International Journal of STD & AIDS. 2010;21:489–96. doi: 10.1258/ijsa.2010.010097. [DOI] [PubMed] [Google Scholar]
- Robinson 2001.Robinson T, Thompson T, Bain B. Sexual risk-taking behavior and HIV knowledge of Kingston’s street boys. Journal of AIDS prevention & education of adolescent children. 2001;4:127–47. [Google Scholar]
- Rohde 2001.Rohde P, Noell J, Ochs L, Seeley J. Depression, suicidal ideation and STD-related risk in homeless older adolescents. Journal of Adolescence. 2001;24:447–60. doi: 10.1006/jado.2001.0382. [DOI] [PubMed] [Google Scholar]
- Rosenthal 2007.Rosenthal D, Mallett S, Gurrin L, Milburn N, Rotheram-Borus MJ. Changes over time among homeless young people in drug dependency, mental illness and their co-morbidity. Psychology, Health & Medicine. 2007;12(1):70–80. doi: 10.1080/13548500600622758. [DOI] [PubMed] [Google Scholar]
- Ross 2006.Ross DA, Dick B, Ferguson J. Preventing HIV/AIDS in young people : a systematic review of the evidence from developing countries. UNAIDS technical report series. 2006;(938) [PubMed] [Google Scholar]
- Ross 2007.Ross DA, Changalucha J, Obasi AI, Todd J, Plummer ML, Cleophas-Mazige B, Anemona A, Everett D, Weiss HA, Mabey DC, Grosskurth H, Hayes RJ. Biological and behavioural impact of an adolescent sexual health intervention in Tanzania: a community randomized trial. AIDS. 2007 Sep 12;21(14):1943–55. doi: 10.1097/QAD.0b013e3282ed3cf5. [DOI] [PubMed] [Google Scholar]
- Rotheram-Borus 1993.Rotheram-Borus MJ, Song J, Gwadz M, Lee M, Van Rossem R, Koopman C. Reductions in HIV Risk Among Runaway Youth. Prevention Science. 1993;4(3):173–87. doi: 10.1023/a:1024697706033. [DOI] [PubMed] [Google Scholar]
- Rotheram-Borus 1996.Rotheram-Borus MJ, Mahler KA, Koopman C, Langabeer K. Sexual abuse history and associated multiple risk behavior in adolescent runaways. American journal of orthopsychiatry. 1996;66(3):390–400. doi: 10.1037/h0080189. [DOI] [PubMed] [Google Scholar]
- Rotheram-Borus 1997.Rotheram-Borus M, Van Rossem R, Gwadz M, Koopman C, Lee M. Reductions in HIV risk among runaway youths. doi: 10.1023/a:1024697706033. [DOI] [PubMed] [Google Scholar]
- Rotheram-Borus 1999.Rotheram-Borus MJ, Koopman C, Haignere C, Davies M. Reducing HIV sexual risk behaviours among runaway adolescents. JAMA. 1999;266(9):1237–41. [PubMed] [Google Scholar]
- Roy 2000.Roy E, Haley N, Leclerc P, Lemire N, Boivin JF, Frappier JY, et al. Prevalence of HIV infection and risk behaviours among Montreal street youth. Int J STD AIDS International journal of STD & AIDS. 2000;11(4):241–7. doi: 10.1258/0956462001915778. [DOI] [PubMed] [Google Scholar]
- Roy 2003.Roy E, Haley N, Leclerc P, Cedras L, Weber AE, Claessens C, et al. HIV incidence among street youth in Montreal, Canada. AIDS. 2003;17(7):1071–5. doi: 10.1097/00002030-200305020-00017. [DOI] [PubMed] [Google Scholar]
- Roy 2004.Roy E, Haley N, Leclerc P, Sochanski B, Boudreau JF, Boivin JF. Mortality in a cohort of street youth in Montreal. JAMA. 2004;292(5):569–74. doi: 10.1001/jama.292.5.569. [DOI] [PubMed] [Google Scholar]
- Ruiz 1994.Ruiz J. Street youth in Colombia: lifestyle, attitudes and knowledge. AIDS health promotion exchange. 1994;1:12–4. [PubMed] [Google Scholar]
- Semaan 2002.Semaan S, Jarlais DCD, Sogolow E, Johnson WD, Hedges GR, Lores FSA, Normal L, Swear MD, Needle R. A meta-analysis of the effect of HIV prevention interventions on the sex behaviors of drug users in the United States. Journal of acquired immune deficiency syndromes. 2002;30:573–593. [PubMed] [Google Scholar]
- Snell 2002.Snell CL. Help-seeking and risk-taking behavior among Black street youth: implications for HIV/AIDS prevention and social policy. The journal of adolescent health. 2002;16(1–2):21–32. doi: 10.1300/j045v16n01_03. [DOI] [PubMed] [Google Scholar]
- Swart-Kruger 1997.Swart-Kruger J, Richter LM. AIDS-related knowledge, attitudes and behaviour among South African street youth: reflections on power, sexuality and the autonomous self. Social science & medicine. 1997;45(6):957–66. doi: 10.1016/s0277-9536(96)00417-0. [DOI] [PubMed] [Google Scholar]
- Taylor 2004.Taylor D, Lyndon J, Bougie E, Johannsen K. “Street kids” toward an understanding of their motivational context. Canadian Journal of Behavioural Science. 2004;36(1):1–16. [Google Scholar]
- Tenner 1998.Tenner AD, Trevithick LA, Wagner V, Burch R. Seattle Youth Care’s prevention, intervention, and education program: a model of care for HIV-positive, homeless, and at-risk youth. The journal of adolescent health. 1998;23(2 Suppl):96–106. doi: 10.1016/s1054-139x(98)00057-3. [DOI] [PubMed] [Google Scholar]
- The World Bank 2010.The World Bank. New Bank Studies. Cash Payments Can Reduce HIV/Sexually Transmitted Infections in Africa? Press release no: 2011/027/HDN 18 July 2010. [Google Scholar]
- UNAIDS 2004.UNAIDS/WHO. AIDS epidemic update: December 2004. 2004. [Google Scholar]
- UNAIDS 2009.UNAIDS. AIDS epidemic update: November 2009. UNAIDS/09.36E/JC1700E. [Google Scholar]
- UNAIDS. AIDS ep1.UNAIDS. AIDS epidemic update. Geneva: WHO; Dec, 2007. Contract No. ;December 2007 Contract No.:Document Number|. [Google Scholar]
- Underhill 2008.Underhill K, Montgomery P, Operario D. Abstinence-plus programs for HIV infection prevention in high-income countries. Cochrane Database of Systematic Reviews. 2008;(1) doi: 10.1002/14651858.CD007006. [DOI] [PubMed] [Google Scholar]
- United Nations 2007.United Nations: department of economic and social affairs. World youth report 2007: Young people’s transition to adulthood: progress and challenges. 2007. [Google Scholar]
- Unknown 1995.No authors listed. Street children turn to sex-work to survive. AIDS Analysis Africa. 1995 Aug;5(4):6–7. [PubMed] [Google Scholar]
- US Code Title 42.United States Code. Title 42, Chapter 119, Subchapter I, subsection 11302.
- van den Hoek 1997.van den Hoek A. STD control in drug users and street youth. Genitourinary medicine. 1997;73(4):240–4. doi: 10.1136/sti.73.4.240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Wormer 2003.Van Wormer R. Homeless youth seeking assistance: a research-based study from Duluth, Minnesota. Child and youth forum. 2003;32(2):89–103. [Google Scholar]
- Walters 1999.Walters AS. HIV prevention in street youth. The journal of adolescent health. 1999;25(3):187–98. doi: 10.1016/s1054-139x(98)00155-4. [DOI] [PubMed] [Google Scholar]
- WHO 2004. [accessed 6 Feb 2008];National AIDS programs: A guide to indicators for monitoring and evaluating national HIV/AIDS prevention programmes for young people. http://www.unaids.org/en/in+focus/monitoringevaluation/m_e+library.asp.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.