Abstract
Objective
To determine whether high weight for length at the 18-month well-baby visit is predictive of overweight or obese body mass index (BMI) at the 4- to 6-year well-child visit.
Design
Retrospective cohort study using objective electronic medical record measurements.
Setting
Eighteen family practices forming a community family health organization in Peterborough, Ont.
Participants
All children from the family health organization practices with at least 1 set of weight and length or height measurements at age 17 to 19 months and age 4 to 6 years (N = 126).
Main outcome measure
Relative risk (RR) of overweight BMI and RR of obese BMI at 4 to 6 years of age for normal versus overweight or obese 18-month-olds.
Results
Children who were either overweight or obese at their 18-month visits (n = 37) were more than twice as likely to be obese at age 4 to 6 years than children who had healthy weights at 18 months were (n = 89; RR = 2.71, 95% CI 1.13 to 6.47). The subgroup of obese 18-month-olds (n = 13) were at more than 3 times the risk of being obese at age 4 to 6 years than their healthy-weight-for-length counterparts (RR = 3.42, 95% CI 1.20 to 9.78). Thirty-one percent of obese 18-month-olds were obese at 4 to 6 years and a further 31% were overweight.
Conclusion
High weight for length at 18 months substantially increased a child’s risk of being overweight or obese at 4 to 6 years of age. Most overweight and obese 18-month-olds in this study did not achieve healthy BMIs by 4 to 6 years of age. A brief glance at the 18-month weight-for-length chart can easily help identify these high-risk toddlers.
Résumé
Objectif
Déterminer si l’enfant qui a un rapport poids : taille élevé lors de l’examen de santé de 18 mois risque d’avoir un indice de masse corporelle (IMC) indiquant un surpoids ou une obésité à l’examen de santé entre 4 et 6 ans.
Type d’étude
Étude de cohorte rétrospective à l’aide de mesures objectives provenant de dossiers médicaux électroniques.
Contexte
Dix-huit cliniques de médecine familiale faisant partie d’une organisation communautaire de santé familiale à Peterborough, Ontario.
Participants
Tous les enfants des cliniques de l’organisation de santé familiale ayant eu au moins une série de mesures de la taille et du poids entre 17 et 19 mois, et entre 4 et 6 ans (n = 126).
Principaux paramètres à l’étude
Risque relatif (RR) d’avoir un IMC de surpoids et RR d’avoir un IMC d’obésité entre 4 et 6 ans chez les enfants de 18 mois de poids normal par rapport à ceux présentant un surpoids ou de l’obésité.
Résultats
Par rapport aux enfants qui avaient un poids santé à la visite de 18 mois, ceux qui présentaient un surpoids ou de l’obésité (n = 37) étaient plus de 2 fois plus susceptibles d’être obèses entre 4 et 6 ans (n = 89; RR = 2,71, IC à 95 % 1,13 à 6,47). Ceux qui faisaient partie du sous-groupe des obèses à 18 mois (n = 13) étaient 3 fois plus à risque d’être obèses entre 4 et 6 ans par rapport à ceux qui avaient un rapport poids : taille santé (RR = 3,42, IC à 95 % 1,20 à 9,78). Parmi ceux qui étaient obèses à 18 mois, 31 % de plus étaient obèses entre 4 et 6 ans et 31 % avaient un surpoids.
Conclusion
Un rapport poids : taille élevé à 18 mois augmente de façon importante le risque de présenter un surpoids ou de l’obésité entre 4 et 6 ans. Dans cette étude, la plupart de ceux qui présentaient un surpoids ou de l’obésité à 18 mois n’atteignaient pas un IMC santé entre 4 et 6 ans. Un simple coup d’œil au tableau des valeurs poids : taille à l’âge de 18 mois permet d’identifier les bambins à haut risque.
The past decade has seen escalating global concern regarding the rising prevalence of being overweight or obese in childhood. In Canada, from 1978 and 1979 to 2004, the prevalence of overweight children aged 2 to 17 increased from 15% to 26%, and the prevalence of obese children almost tripled, from 3% to 8%.1 This epidemic has important implications for Canadian children. Obese children often become obese adults,2,3 and the myriad complications of obesity are well documented.4,5 However, the psychological toll of obesity on children is often overlooked. Being an overweight or obese child is associated with significantly lower self-esteem, as reported by parents (P ≤ .001),6 as well as decreased physical, social, and psychological function.7 Moreover, being a severely obese child or adolescent is comparable to having a diagnosis of cancer in terms of its effect on health-related quality of life.7 Thus, considerable damage can be done even if weight normalizes by adulthood.
Given the above complications, emphasis on early obesity prediction, recognition, and intervention has increased dramatically. This interest has produced a growing understanding of the factors that place a child at increased risk of being overweight or obese (Table 1).1,4,8–17 In addition, these factors often cluster together to form particularly unhealthy circumstances.8,18,19 Unfortunately, these clusters can be identified in children as young as 2 years of age.18 Despite this, most studies on childhood obesity are conducted well beyond the preschool years. By this time, behaviour and attitudes are more ingrained, and psychological damage might have already been done. Among the studies that did examine obesity during the preschool years, one showed that 60% of overweight 2- to 3-year-olds remained overweight at the age of 12.20 Another demonstrated a significant increase in the risk of adult obesity among overweight children as young as 3 years of age (odds ratio 4.1, 95% CI 2.5–6.7), although not among 1- to 2-year-olds. In that study, overweight 6-year-olds had a 50% chance of becoming overweight adults.21
Table 1.
Summary of risk factors and protective factors for overweight and obese BMI in childhood
| CHARACTERISTICS | RISK FACTORS | PROTECTIVE FACTORS |
|---|---|---|
| Sociodemographic4,8–10 |
|
|
| Dietary4,8–14 |
|
|
| Physical activity1,8–10,14,15 |
|
|
| Genetic4,16 |
|
|
| Prenatal4,9,10,14,17 |
|
|
| Other4 |
|
|
BMI—body mass index, NA—not applicable.
Endocrine conditions do not typically cause obesity in the absence of other manifestations; routine screening is not recommended.
Beyond the above studies, very few published studies exist on the relationship between weight in infancy and weight in early childhood or adulthood, particularly for children younger than 2 years of age. The purpose of this study was to use objective family practice data to determine if high weight for length at the 18-month well-baby visit increases a child’s risk of being overweight or obese at the 4- to 6-year well-child visit. It was predicted that weight for length above the 85th percentile at 18 months would substantially increase the risk of a child being overweight or obese at 4 to 6 years of age, and that weight for length above the 97th percentile at 18 months would place a child at even greater risk.
METHODS
This was a retrospective cohort study using objective measurements extracted from an electronic medical record (EMR) system that included 18 family practices forming a community family health organization in Peterborough, Ont. This study was approved by the Queen’s University and Affiliated Hospitals Health Science Research Ethics Board.
Chart selection
Electronic charts of rostered children were reviewed if, based on the child’s date of birth, the chart potentially included visits at 17 to 19 months and 4 to 6 years of age. Charts of children who were 17 to 19 months of age before the adoption of the EMR in early 2006 and those of children who had not yet reached their fourth birthdays were excluded. There were no additional exclusion criteria. Each potentially eligible electronic chart was reviewed, and was included in the final data set if the chart contained at least 1 set of weight and length measurements at both 17 to 19 months of age and 4 to 6 years of age. To help maintain patient anonymity, and because this study was intended to demonstrate the utility of electronic growth chart review, no paper chart data were reviewed.
Outcome measurements
Age, sex, weight, and length or height were extracted retrospectively from the EMR. If more than 1 set of measurements was recorded in the 17- to 19-month and 4- to 6-year time frames, the sets closest to 18 months and 6 years were used. Each child was classified as healthy weight, overweight, or obese at each age using age- and sex-adjusted percentiles for weight for length (17- to 19-month visit) and body mass index (BMI) (4- to 6-year visit). Consistent with standard Canadian practice, weight-for-length and BMI percentiles were based on the 2006 World Health Organization (WHO) growth standards. To maintain consistency for the purpose of this study, obesity was defined as weight for length or BMI above the 97th percentile at each age, and overweight was defined as weight for length or BMI above the 85th percentile for age and sex. Both of these percentiles are identified by lines on the WHO growth curves, facilitating rapid, visual interpretation of measurements in day-to-day family practice. Notably, these definitions differ somewhat from the traditional WHO definitions of overweight and obese, which vary for children aged 0 to 2 years, 2 to 5 years, and 5 to 19 years. For this study, a consistent definition of overweight and obese across age groups was necessary to make data analysis and interpretation practical.
Statistical testing
Relative risk (RR) ratios and 95% CIs were calculated to determine the extent to which being overweight or obese at the 18-month visit predicted overweight or obese BMI at the 4- to 6-year visit. The following comparisons were conducted: RR of obesity at 4 to 6 years of age among healthy-weight versus combined overweight and obese 18-month-olds; RR of being overweight or obese at 4 to 6 years of age among healthy-weight versus combined overweight and obese 18-month-olds; and RR of obesity at 4 to 6 years among obese versus healthy-weight 18-month-olds.
RESULTS
Final sample
Based solely on patient date of birth, a total of 720 potentially eligible electronic charts were reviewed. Among these charts, matched measurements at 17 to 19 months and 4 to 6 years of age were available for 126 children, including 64 females and 62 males. The mean age at the 4- to 6-year visit was 4 years, 9 months. Table 2 explains the reasons for missing data in the charts that were potentially eligible but that were eventually excluded. In most cases, this was because the child had joined the clinic after 19 months of age (31%) or because the child had other measurements in the chart but none during the target time frames (45%). In about 18% of cases, measurements were either incomplete or absent entirely.
Table 2.
Reasons for missing data among children within the target age group: N = 594; some missing measurements for some practices might have been present on older paper charts.
| REASON | N (%) |
|---|---|
| Measurements in EMR at other ages, but no measurements in target age ranges | |
| • No measurements at 17–19 mo | 105 (18) |
| • No measurements at 4–6 y | 77 (13) |
| • Neither set of measurements | 88 (15) |
| No length or height recorded for 1 or both visits | |
| • No length for visit at 17–19 mo | 23 (4) |
| • No height for visit at 4–6 y | 12 (2) |
| • No height at either visit | 2 (< 1) |
| Missing 3 of 4 measurement parameters | |
| • Only 18-mo weight recorded | 20 (3) |
| • Only 4- to 6-y weight recorded | 13 (2) |
| • Only 18-mo length recorded | 1 (< 1) |
| Visits but no measurements in EMR at any time | 35 (6) |
| Joined clinic after age 17–19 mo | 184 (31) |
| No longer a clinic patient | 20 (3) |
| Age 17–19 mo before implementation of EMR in specific practice | 10 (2) |
| Invalid measurements (eg, height of 10 m) | 4 (1) |
EMR—electronic medical record.
The prevalence of healthy weight, overweight, and obese weight for length at the 18-month visits and BMI at the 4- to 6-year visits is shown in Table 3. More than 1 in 4 children in this study (29%) was classified as overweight or obese at 18 months, and 1 in 3 (32%) was classified as overweight or obese at 4 to 6 years.
Table 3.
Prevalence of healthy, overweight, and obese weight for length at 18-month well-baby visits and BMI at 4- to 6-year well-child visits: N = 126; overweight defined as 18-month weight for length or 4-to 6-year BMI above the 85th percentile for age and sex; obesity defined as 18-month weight for length or 4- to 6-year BMI above the 97th percentile for age and sex.
| CATEGORY | AT 18 MO, N (%) | AT 4–6 Y,* N (%) |
|---|---|---|
| Healthy weight | 89 (71) | 85 (67) |
| Overweight | 24 (19) | 24 (19) |
| Obese | 13 (10) | 17 (13) |
BMI—body mass index.
As a result of rounding, percentages do not equal 100%.
Predicting overweight and obese BMI at 4 to 6 years of age
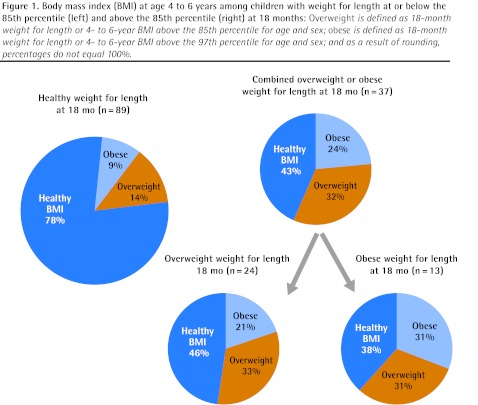
Figure 1 illustrates the difference in BMI at 4 to 6 years of age between children who were at healthy weights at their 18-month well-baby visits (n = 89) compared with those who were overweight (n = 24) or obese (n = 13) at their 18-month well-baby visits. Children who were overweight or obese at 18 months were more than twice as likely to be overweight or obese at 4 to 6 years than children who had healthy weights at 18 months (RR = 2.53, 95% CI 1.57 to 4.07 for being at least overweight at 4 to 6 years; RR = 2.71, 95% CI 1.13 to 6.47 for being obese at 4 to 6 years). Among those who were overweight or obese at 18 months, 57% were still overweight or obese at 4 to 6 years.
Figure 1.
Body mass index (BMI) at age 4 to 6 years among children with weight for length at or below the 85th percentile (left) and above the 85th percentile (right) at 18 months: Overweight is defined as 18-month weight for length or 4- to 6-year BMI above the 85th percentile for age and sex; obese is defined as 18-month weight for length or 4- to 6-year BMI above the 97th percentile for age and sex; and as a result of rounding, percentages do not equal 100%.
The effect of high weight for length is even more notable for the subgroup of 18-month-olds with weight for length above the 97th percentile. Compared with 18-month-olds with weight for length at or below the 85th percentile, the obese 18-month-olds were at more than 3 times the risk of being obese at 4 to 6 years (RR = 3.42, 95% CI 1.20 to 9.78). In fact, 31% of obese 18-month-olds remained obese at 4 to 6 years and a further 31% continued to be overweight; only a minority of obese 18-month-olds (38%) achieved healthy weights. Overall, looking across the healthy-weight, overweight, and obese groups of 18-month-olds, the risk of obesity at age 4 to 6 progressively increased from 9% to 21% to 31%, and the chances of being at a healthy weight at 4 to 6 years progressively decreased from 78% to 46% to 38%, respectively.
DISCUSSION
Early childhood is a key period in the development of both nutritional and behavioural habits.18 Thus, the purpose of this study was to determine whether children with high weight for length as early as the 18-month well-baby visit are at increased risk of obesity in later childhood. Using objective EMR data, it was determined that children in this study with weight for length above the 85th percentile at 18 months were at more than twice the risk of being overweight or obese at 4 to 6 years than their healthy-weight counterparts, and those with weight for length above the 97th percentile were at more than triple the risk. In all, 62% of obese 18-month-olds were overweight or obese at 4 to 6 years. In other words, most overweight or obese 18-month-olds in this study did not outgrow this condition.
These findings have important implications for family practice. They suggest that children who are at risk of childhood obesity, and likely adult obesity, can and should be identified even earlier than previously suggested. Previous evidence has suggested that 60% of overweight preschoolers remained overweight as 12-year-olds,20 and that overweight 3-year-olds are at an increased risk of adult obesity.21 Taken with the findings of the present study, it is plausible that obese 18-month-olds might be at a higher risk of adult obesity.
A recent study has also suggested that obesity in childhood significantly increases the risk of later cardiovascular disease (P ≤ .002) if weight does not normalize by adulthood.22 Similarly, the profound psychological effects of obesity on children6,7 cannot be ignored. Thus, the finding that obese 18-month-olds tend to become overweight or obese 4- to 6-year-olds provides us with an opportunity to intervene at a very early stage in the hope of preventing these physical and psychological complications.
These findings also highlight the importance of obtaining and reviewing accurate measurements at every well-child visit. Unfortunately, more than 1 in 6 electronic charts reviewed for this study contained incomplete measurements or no measurements at all. Further, a study of family physicians in the United States revealed that, based on self-report, nearly 1 in 10 never used the weight-for-length chart, and only approximately 50% routinely calculated childhood BMI.23 In the era of EMRs, viewing these measurements requires only a glance at an electronic growth chart. Overall, a brief review of weight for length at all 18-month visits appears appropriate to rapidly and objectively identify toddlers whose risk of later obesity could be double or triple that of their peers.
This study has several key strengths that make it applicable to daily family practice. All children were patients of community family practices, as opposed to specialty pediatric, referral, or self-selected samples of children. The measurements used are already a part of routine well-child care, and the weight-for-length and BMI cutoffs used to identify children as overweight or obese are easily identifiable as important percentile lines on the Canadian WHO growth charts. As such, family physicians can see at a glance which category a child falls into, and counsel families appropriately. Finally, matched, objective height and weight measurements eliminate potential problems with self-reported and case-control data.
Limitations
The final sample of 126 children was derived through review of more than 700 charts. The prevalence of unhealthy weight in children in the final study sample was higher than that in the Canadian population as of 2004.1 Ours was also a relatively small sample and it might not be representative of the Canadian population. Future studies, including several that are in progress, will track larger samples of children for longer periods of time, ideally into adulthood. Studies should also work to determine whether family physician counseling at the 18-month visit can ultimately change toddlers’ outcomes. Finally, it is important to note that high weight for length is only one of many risk factors (Table 1), and that any proposed treatment plan must clearly be multi-factorial and centred on appropriate family nutrition and physical activity.
Conclusion
For the toddlers in this study, weight for length above the 85th percentile, especially above the 97th percentile, by 18 months of age was a red flag suggesting a substantially increased risk of being overweight or obese at 4 to 6 years of age. Most children who were overweight or obese at 18 months did not attain healthy weights over time, and this could have profound long-term mental and physical health implications for them. A brief glance at the 18-month weight-for-length chart could provide family physicians with valuable risk stratification information within the time limits of routine well-child care.
EDITOR’S KEY POINTS
In this study, children with weight for length above the 85th percentile at 18 months were at more than twice the risk of being overweight or obese at 4 to 6 years than their healthy-weight counterparts were, and those with weight for length above the 97th percentile were at more than triple the risk.
Most children who were overweight or obese at 18 months did not attain healthy weights over time, and this could have profound long-term mental and physical health implications.
These findings also highlight the importance of obtaining and reviewing accurate measurements at every well-child visit.
POINTS DE REPÈRE DU RÉDACTEUR
Dans cette étude, les enfants qui, à 18 mois, avaient un rapport poids : taille supérieur au 85e percentile avaient un risque de présenter un surpoids ou de l’obésité entre 4 et 6 ans plus de 2 fois plus grand que ceux qui avaient un poids santé, alors que pour ceux qui avaient un rapport au-dessus du 97e percentile, le risque était 3 fois plus grand.
La plupart des enfants qui présentaient un surpoids ou de l’obésité à 18 mois n’ont pas atteint un poids santé avec le temps, ce qui, à long terme, pourrait avoir des conséquences majeures sur le plan de la santé physique et mentale.
Ces observations soulignent aussi l’importance de faire des mesures précises et de les répéter à chaque visite.
Footnotes
This article has been peer reviewed.
Cet article a fait l’objet d’une révision par des pairs.
Competing interests
None declared
References
- 1.Shields M. Nutrition: findings from the Canadian Community Health Survey. 1. Ottawa, ON: Statistics Canada; 2005. Measured obesity. Overweight Canadian children and adolescents. Available from: www.statcan.gc.ca/pub/82-620-m/2005001/pdf/4193660-eng.pdf. Accessed 2013 Mar 15. [Google Scholar]
- 2.Whitaker RC, Wright JA, Pepe MS, Seidel KD, Bietz MH. Predicting obesity in young adulthood from childhood and parental obesity. N Engl J Med. 1997;337(13):869–73. doi: 10.1056/NEJM199709253371301. [DOI] [PubMed] [Google Scholar]
- 3.Guo SS, Wu W, Chumlea WC, Roche AF. Predicting overweight and obesity in adulthood from body mass index values in childhood and adolescence. Am J Clin Nutr. 2002;76(3):653–8. doi: 10.1093/ajcn/76.3.653. [DOI] [PubMed] [Google Scholar]
- 4.Speiser PW, Rudolf MC, Anhalt H, Camacho-Hubner C, Chiarelli F, Eliakim A, et al. Childhood obesity. J Clin Endocrinol Metab. 2005;90(3):1871–87. doi: 10.1210/jc.2004-1389. Epub 2004 Dec 14. [DOI] [PubMed] [Google Scholar]
- 5.Katzmarzyk PT, Janssen I. The economic costs associated with physical inactivity and obesity in Canada: an update. Can J Appl Physiol. 2004;29(1):90–115. doi: 10.1139/h04-008. [DOI] [PubMed] [Google Scholar]
- 6.Hesketh K, Wake M, Waters E. Body mass index and parent-reported self-esteem in elementary school children: evidence for a causal relationship. Int J Obes Relat Metab Disord. 2004;28(10):1233–7. doi: 10.1038/sj.ijo.0802624. [DOI] [PubMed] [Google Scholar]
- 7.Schwimmer JB, Burwinkle TM, Varni JW. Health-related quality of life of severely obese children and adolescents. JAMA. 2003;289(14):1813–9. doi: 10.1001/jama.289.14.1813. [DOI] [PubMed] [Google Scholar]
- 8.Veugelers PJ, Fitzgerald AL. Prevalence of and risk factors for childhood overweight and obesity. CMAJ. 2005;173(6):607–13. doi: 10.1503/cmaj.050445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Birch LL, Ventura AK. Preventing childhood obesity: what works? Int J Obes (Lond) 2009;33(Suppl 1):S74–81. doi: 10.1038/ijo.2009.22. [DOI] [PubMed] [Google Scholar]
- 10.Vos MB, Welsh J. Childhood obesity: update on predisposing factors and prevention strategies. Curr Gastroenterol Rep. 2010;12(4):280–7. doi: 10.1007/s11894-010-0116-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Anzman SL, Birch LL. Low inhibitory control and restrictive feeding practices predict weight outcomes. J Pediatr. 2009;155(5):651–6. doi: 10.1016/j.jpeds.2009.04.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Metzger MW, McDade TW. Breastfeeding as obesity prevention in the United States: a sibling difference model. Am J Hum Biol. 2010;22(3):291–6. doi: 10.1002/ajhb.20982. Epub 2009 Aug 19. [DOI] [PubMed] [Google Scholar]
- 13.Grummer-Strawn LM, Mei Z, Centers for Disease Control and Prevention Pediatric Nutrition Surveillance System Does breastfeeding protect against pediatric overweight? Analysis of longitudinal data from the Centers for Disease Control and Prevention Pediatric Nutrition Surveillance System. Pediatrics. 2004;113(2):e81–6. doi: 10.1542/peds.113.2.e81. [DOI] [PubMed] [Google Scholar]
- 14.Han JC, Lawlor DA, Kimm SY. Childhood obesity. Lancet. 2010;375(9727):1737–48. doi: 10.1016/S0140-6736(10)60171-7. Epub 2010 May 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Janssen I, Katzmarzyk PT, Boyce WF, King MA, Pickett W. Overweight and obesity in Canadian adolescents and their associations with dietary habits and physical activity patterns. J Adolesc Health. 2004;35(5):360–7. doi: 10.1016/j.jadohealth.2003.11.095. [DOI] [PubMed] [Google Scholar]
- 16.Silventoinen K, Rokholm B, Kaprio J, Sørensen TI. The genetic and environmental influences on childhood obesity: a systematic review of twin and adoption studies. Int J Obes (Lond) 2010;34(1):29–40. doi: 10.1038/ijo.2009.177. Epub 2009 Sep 15. [DOI] [PubMed] [Google Scholar]
- 17.Yu ZB, Han SP, Zhu GZ, Zhu C, Wang XJ, Cao XG, et al. Birth weight and subsequent risk of obesity: a systematic review and meta-analysis. Obes Rev. 2011;12(7):525–42. doi: 10.1111/j.1467-789X.2011.00867.x. Epub 2011 Mar 28. [DOI] [PubMed] [Google Scholar]
- 18.Gubbels JS, Kremers SP, Stafleu A, Dagnelie PC, de Vries SI, de Vries NK, et al. Clustering of dietary intake and sedentary behaviour in 2-year-old children. J Pediatr. 2009;155(2):194–8. doi: 10.1016/j.jpeds.2009.02.027. Epub 2009 Apr 25. [DOI] [PubMed] [Google Scholar]
- 19.Cameron AJ, Crawford DA, Salmon J, Campbell K, McNaughton SA, Mishra GD, et al. Clustering of obesity-related behaviors in children and their mothers. Ann Epidemiol. 2011;21(2):95–102. doi: 10.1016/j.annepidem.2010.11.001. [DOI] [PubMed] [Google Scholar]
- 20.Nader PR, O’Brien M, Houts R, Bradley R, Belsky J, Crosnoe R, et al. Identifying risk for obesity in early childhood. Pediatrics. 2006;118(3):e594–601. doi: 10.1542/peds.2005-2801. [DOI] [PubMed] [Google Scholar]
- 21.Whitaker RC, Wright JA, Pepe MS, Seidel KD, Dietz WH. Predicting obesity in young adulthood from childhood and parental obesity. N Engl J Med. 1997;337(13):869–73. doi: 10.1056/NEJM199709253371301. [DOI] [PubMed] [Google Scholar]
- 22.Juonala M, Magnussen CG, Berenson GS, Venn A, Burns TL, Sabin MA, et al. Childhood adiposity, adult adiposity, and cardiovascular risk factors. N Engl J Med. 2011;365(20):1876–85. doi: 10.1056/NEJMoa1010112. [DOI] [PubMed] [Google Scholar]
- 23.Huang TTK, Borowski LA, Liu B, Galuska DA, Ballard-Barbash R, Yanovski SZ, et al. Pediatricians’ and family physicians’ weight-related care of children in the U.S. Am J Prev Med. 2011;41(1):24–32. doi: 10.1016/j.amepre.2011.03.016. [DOI] [PMC free article] [PubMed] [Google Scholar]