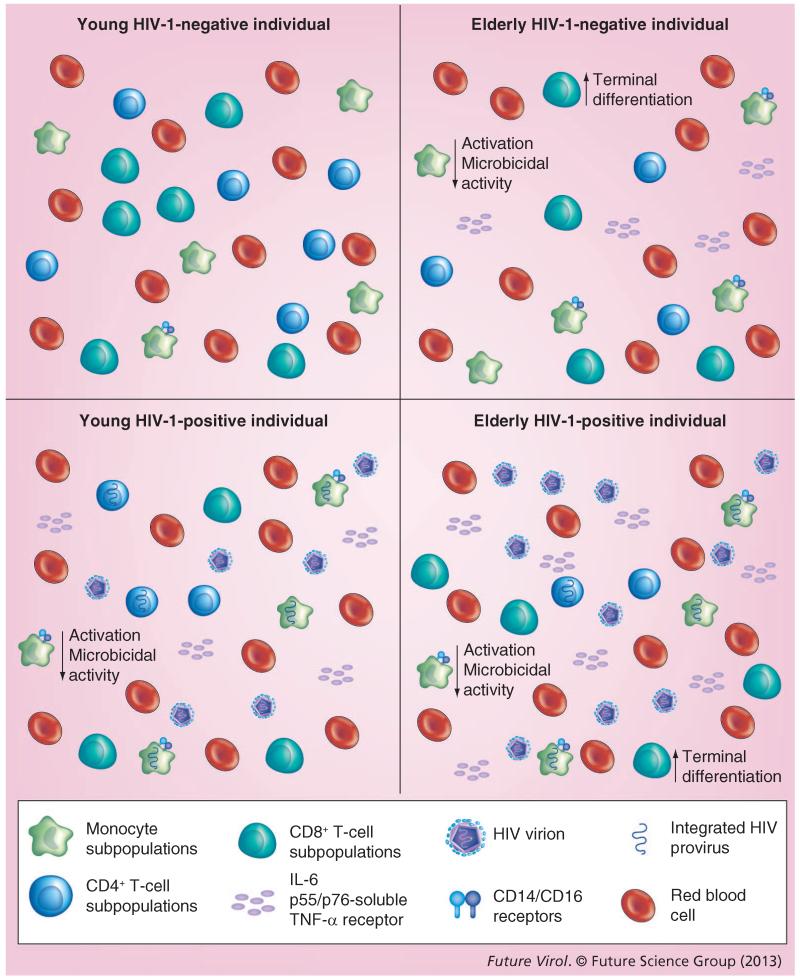
Figure 2. Immune regulation in response to aging and HIV-1 infection.
As an individual ages, immune competence declines and changes occur in the overall function of the immune system. With aging, the number of terminally differentiated CD8+ T cells increases, while their ability to proliferate decreases and CD28 expression decreases. There are also fewer naive CD8+ T cells. Aging also decreases the number and function of CD4+ T cells. This decrease has also been shown to lead to a decrease in the overall CD4+:CD8+ T-cell ratio. HIV-1 infection itself also induces changes in the overall number and function of CD4+ T cells, increasing the number of terminally differentiated CD8+ T cells and decreasing the ability of CD8+ T cells to proliferate. Even though the number of CD4+ T cells decreases, the number of memory CD4+ T cells increases; however, these memory cells are less able to respond to pathogens. Blood monocytes and tissue macrophages typically have a decreased level of activation in older, uninfected patients. Large increases have also been shown in CD14+/CD16+ receptors on mature monocytes in the elderly. This was similar to what was observed in younger HIV-1-infected patients. Within both the older uninfected population, as well as HIV-1-infected patients, macrophages appeared to have diminished microbicidal capability. However, not all aging-related changes have centered on a loss of function. IL-6 cytokine levels increase with aging, as well as independently with HIV-1 infection. p55- and p75-soluble TNF-α receptor levels also increase. These levels all increase further in HIV-1-infected patients as they age.