Abstract
The aim of the study was to evaluate the mid-term clinical results and survivorship of a rotating-hinge knee prosthesis (LINK® Endo-Model) in difficult primary and complex revision situations. Results after primary implantation were compared with those of revision procedures. Forty-nine prostheses in 45 patients were reviewed clinically during follow up. Twenty-one of these were implanted in primary and 28 in revision situations. Outcome was evaluated using commonly used scores (Knee Society, UCLA Activity, Lequesne) and a visual analog scale after a mean follow up of 56±37 months for 49 prostheses. Implant survival was analyzed using the Kaplan-Meier method. There were no significant differences in clinical examination and evaluation scores between the two groups (P>0.05). Survival rates at final follow up were 95% after primary implantation and 76% in revision procedures. The risk of prosthesis loss (odds ratio 5.7) was significantly higher after revision procedures (P=0.004). These data suggest that rotating-hinge knee prostheses provided good clinical and functional results in selected cases of advanced primary gonarthrosis associated with severe bone loss, ligamentous instability or comminuted fractures. They also provide good results in revision situations. However, the failure rate was significantly higher in cases of revision surgery.
Key words: rotating-hinge knee prosthesis, knee, TKA, revision, survivorship.
Introduction
Routine use of total knee arthroplasty (TKA) began in the mid-1970s. Particular challenges for primary implantation are major axis deviations, deformity and ligament instability.1 Inevitably, the growing number of primary implants also led to an increasing number of revision procedures.2 It is often not possible to undertake these revision procedures adequately using conventional non-linked knee prostheses. Further development of early hinged prostheses produced intracondylar knee joint prostheses with a rotational capacity.3 These provide an alternative in clinical situations that cannot be solved by non-constrained knee prostheses. In primary implantations, such situations include axis deviations, loss of bone substance, and marked insufficiency of the collateral ligaments.4
Recently, clinical and radiological results for rotating-hinge prostheses have been reported, but conclusions are contradictory. Some authors suggest that rotating-hinge prostheses should be used mainly in salvage procedures in revision cases,5–7 whereas others have described rotating-hinge prostheses to be suitable for advanced and difficult primary osteoarthritis.8 However, the literature is difficult to analyze because most of the studies use rotating-hinge prostheses in revision situations. In cases of advanced primary osteoarthritis (in which less constrained prostheses would possibly not restore a well-balanced and aligned knee joint), rotating-hinge prostheses could be more favorable. Only one study has analyzed a relatively high number of primary rotating-hinge prostheses with patient-related outcome and survivorship.8
The prevalence of complications seems to be higher compared with non-constrained TKA owing to the greater level of invasiveness in the implantation of hinged prostheses with intramedullary fixation.9,10 Survivorship will also be reduced due to the increased stress placed at the implant-bone interface, secondary to the less normal kinematics of the joint and resulting increased forces generated.11 Even the scores for clinical results seem to be worse than in conventional non-constrained replacement of the knee.12 In cases requiring explantation or a revision procedure, surgical options are limited and can be accompanied by a related loss of function.9
Several complex cases are being treated in our university hospital. These include valgus or varus deformities of over 20°, cases with rheumatoid arthritis or Charcot joints, as well as unstable joints with complex bone damage. The aim of the present study was to investigate the mid-term results and survivorship after implantation of LINK® Endo-Model rotating-hinge knee prostheses. In particular, we compared the differences in difficult primary and complex revisions.
Materials and Methods
Between 1995 and 2005, 121 LINK® Endo-Model rotating-hinge knee prostheses were implanted in 113 patients in a single center. Fifty-three patients (46 female, 7 male) underwent primary arthroplasties, and 59 (42 female, 17 male) patients underwent revision procedures. One patient received primary implantation as well as a revision procedure. Seven patients underwent bilateral arthroplasty. At follow up, 69 patients with 72 prostheses could not be further investigated: nine patients could no longer be contacted or did not give their consent to further investigation and 23 patients had died; 12 patients were disabled from medical conditions that prevented objective evaluation of the status of their knee arthroplasty; implant failure was reported in 18 patients; 7 patients refused a clinical investigation or did not attend such an investigation for other reasons; however, they were willing to be interviewed by telephone. Forty-nine prostheses in 45 patients were clinically documented during follow up. Of these, 21 were primary implants and 28 were revision procedures (Figure 1).
Figure 1.
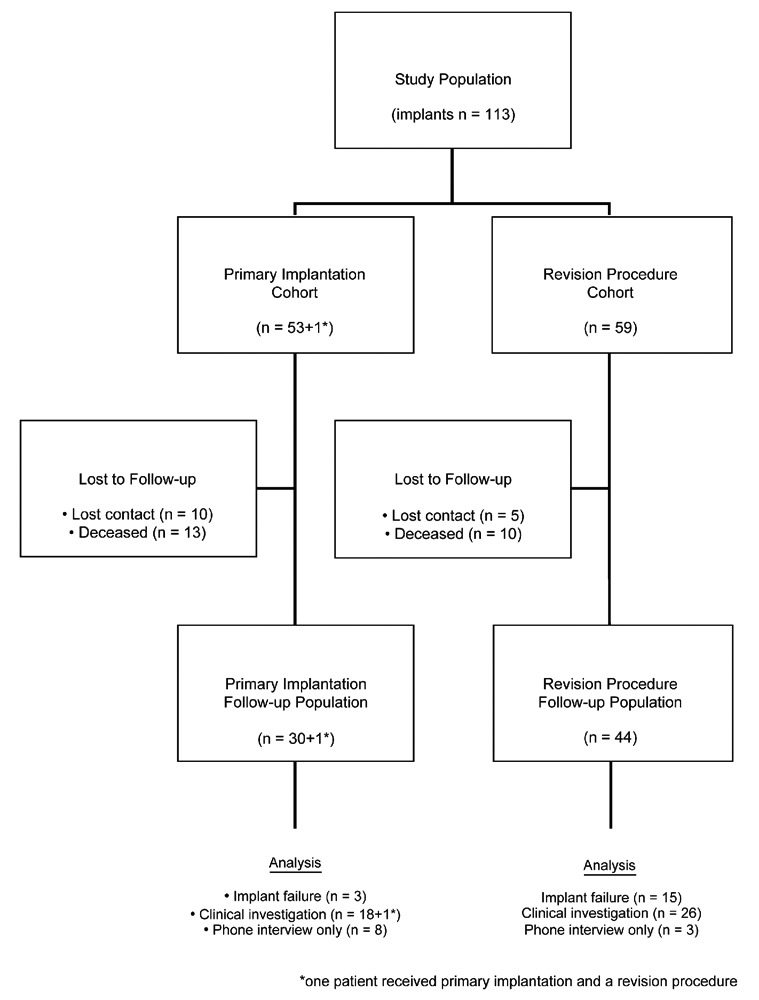
Patient outcome within the two study populations.
Mean follow up was 56±37 months (range 10–133; median 55) for 49 prostheses. Mean body mass index was 25.9±4.4 kg/m2 (range 17.7–37.7; median 30) for primary implantations and 30±5.2 kg/m2 (range 19.1–47.3; median 30) for revision procedures. Mean age was 73.7 years for primary implantations and 72.5 years for revision procedures.
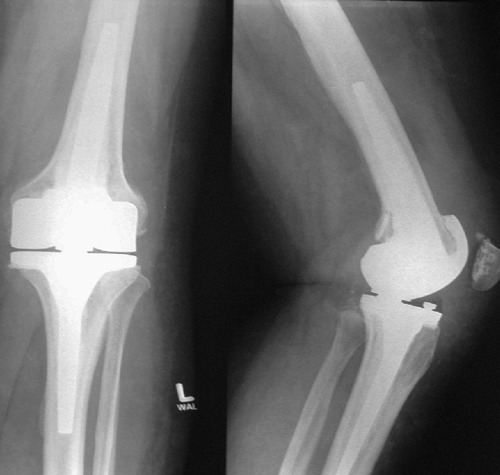
Indications for use of the Endo-Model rotating-hinge knee prostheses in primary implantation (Figure 2) were primary osteoarthritis in 31 cases, rheumatoid arthritis in 20, and post-traumatic conditions in 5. In these cases, primary rotating-hinge knee prostheses were considered necessary owing to severe bone loss, ligamentous instability, knee malalignment, comminuted distal femur fractures, and ankylosis requiring mass bone resection. Finally, 2 cases of infection were indications for primary implantation. Main indications for revision procedures were infection in 26 cases and aseptic loosening in 23 cases, as well as instability in 6 cases, periprosthetic fractures in 4, malimplantation in 2 and bad range of motion or progressive arthrosis in one.
Figure 2.

Pre-operative X-ray of a patient with severe destruction of the left knee joint caused by rheumatoid arthritis.
The Endo-Model rotating-hinge knee prosthesis was developed in 1979 by Waldemar LINK GmbH (Hamburg, Germany).3 The stem of the femoral component has a valgus angle of 6°. The prostheses were implanted with complete cementation of the stems using medullary plugs and a second-generation cementation technique (Figure 3). Patella resurfacing was undertaken in 25 cases of primary implantation and 30 cases of revision procedures.
Figure 3.
X-ray after treatment with a LINK® Endo-Model® rotating-hinge knee prosthesis.
Tables 1 and 2 provide a synopsis of the causes for implant failure after primary implantations as well as after revision procedures. In cases of infection, a 2-stage revision was carried out with the interim use of a bone cement spacer before implantation of another prosthe-sis. Explantations after revision procedures occurred at a mean time interval of 21.6 months (range 1–54; median 19) after implantation. Eight prostheses were explanted during the first 12 months (3 during the first 24 months). The most common cause for explantation was deep infection; this was most commonly associated with revision procedures (Table 2).
Table 1. Causes of implant failure after primary implantation (n=3).
| Event leading to implant failure | |
|---|---|
| N=1 | Recurrent dislocation |
| N=1 | Periprosthetic femoral fracture |
| N=1 | Infection |
Table 2. Causes of implant failure after revision procedure (n=15).
| Event leading to implant failure (clinical consequence) | |
|---|---|
| N=8 | Infection (5 arthrodeses, 3 above knee amp.) |
| N=2 | Aseptic loosening (1 change of prosthesis, 1 above knee amp.) |
| N=1 | Inlay-breakage (1 arthrodesis) |
| N=1 | Periprosthetic femoral fracture (1 change of prosthesis) |
| N=1 | Chronic pain (1 change of prosthesis) |
| N=1 | Septic loosening (1 change of prosthesis) |
| N=1 | Recurrent dislocation (1 change of prosthesis) |
All patients available for clinical investigation underwent physical examination and application of patient-related outcome measurements. Parameters [pain, stability, range of motion (ROM), axial alignment] were documented using the Knee Society Score (KSS),13 which consists of clinical and functional sections. The clinical section quantifies the parameters of pain, ROM, stability and axis deviation. In the functional section, the load capacity on the knee joint is evaluated. Scores of 80 or over are considered to be excellent, 79–70 to be good, 69–60 to be fair, and below 60 to be poor. Patients were also asked to rate their pain on a horizontal, 100-mm line bounded by no pain on the left and intolerable pain on the right using a visual analogue scale (VAS). The Lequesne Index is a 10-question survey.14 Five questions deal with pain or discomfort, one question deals with maximum walking distance, and four questions address the activities of daily living. The questionnaire is scored on a scale of 0 to 24. Lower scores indicate less functional impairment.
Statistical analyses
Differences in measurements of patient-related outcome between primary and revision implants were verified using the Mann-Whitney U-Test. P<0.05 was considered significant. Data analyses were carried out using Microsoft Excel (Microsoft Corporation, Seattle, WA, USA) and SPSS (SPSS-Science, Chicago, IL, USA) software programs. Lifetime survival functions were set up according to the Kaplan-Meier analysis.
Results
The clinical section of the KSS (part A) gave an average score of 82±13 (range 57–97; median 87) points after primary implantation and 80±15 (range 46–94; median 86) after revision procedures (P=0.12) (Figure 4). In scores concerning pain symptomatology, patients with primary implantations (mean 45±5; median 45) tended to fare better than patients after revision procedures (38±14; median 45; P=0.05). Eighty-six percent of the patients reported slight or no pain after primary implantation, whereas 61% reported the same after revision procedures (P=0.84). The mean ROM was 88±25° after primary implantation and 89±23° after revision procedures (P=0.67). With over 90° flexion, most of the patients showed satisfactory results in this regard (67% for primary implantations and 68% for revision procedures). Ranges of motion with flexion below 90° were observed in 7 primary implantations (33%) and 9 revision procedures (32%). Six out of 7 patients with primary implantations showed a flexion contracture before surgery. For patients with revision procedures, poor results were mainly due to flexion deficits in 8 cases.
Figure 4.
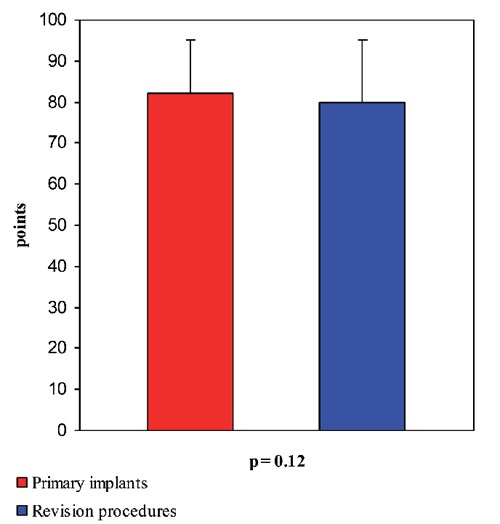
Outcome of the clinical section of the KSS (part A): primary implants versus revision procedures.
The functional section of the KSS (Part B) showed an average score of 58±29 (range −20 to 100; median 50) points after primary implantation and 47±26 (range −20 to 100; median 45) after revision procedures (P=0.08) (Figure 5). With regard to the mean walking distance, patients after revision procedures (38±13, median 40) were slightly better (P=0.02) than patients after primary implantations (27±14, median 30). With respect to the ability to climb stairs, no significant differences were noted between the two groups (P=0.39). The same applied to the use of walking frames P=0.79). In both groups, most of the patients had to use walking frames (81% for primary implantations and 79% for revision procedures).
Figure 5.
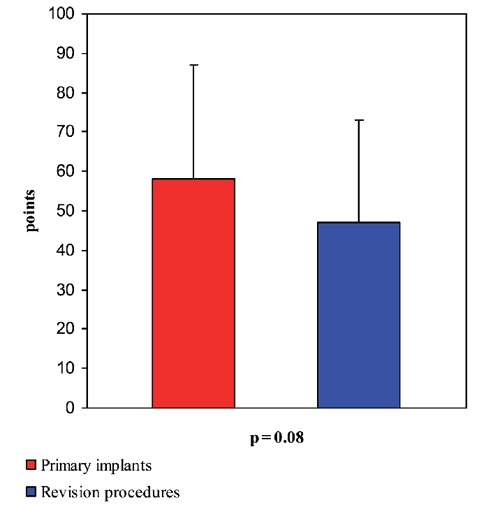
Outcome of the functional section of the KSS (part B): primary implants versus revision procedures.
Patients after primary implantation achieved results of 12±5 (range 0–22; median 11) points and after revision procedures achieved 10±5 (range 0–22, median 9) points in the Lequesne Index (P=0.13). Activity levels of 4±1 (range 2–6; median 4) after primary implantation and 4±1 (range 2–7, median 4) after revision procedures were reached in the University of California at Los Angeles (UCLA) Activity Score (P=0.11). No significant differences were found regarding the VAS: mean 30±23 mm, median 31 mm for primary implantations; and mean 30±24 mm, median 31 mm for revision procedures (P=0.85).
Eighteen rotating-hinge knee prostheses (3 primary and 15 revision implants) had to be explanted. Survival rates in study populations at final follow up were 95% after primary implantation and 76% in revision procedures (Figure 6). The risk of prosthesis loss (odds ratio 5.7) was significantly higher after revision procedures (P=0.004).
Figure 6.
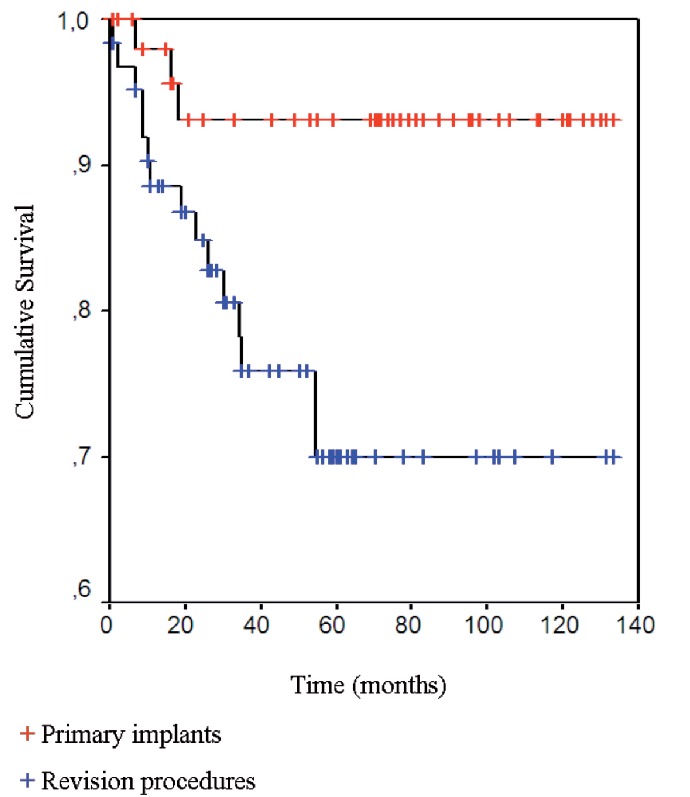
Kaplan-Meier survival analyses: primary implants versus revision procedures.
Discussion
The rotating-hinge knee prostheses used in the present study provided good clinical and functional results in difficult primary and complex revision knee arthroplasty. There was no significant difference in clinical and functional results between the two groups. However, patients after revision procedures showed a longer walking distance in the KSS than patients after primary implantation. Clinical scores are undoubtedly influenced by the mean age of the patient population and the completeness of the follow up.15 Of the clinical points available in the KSS, 30 points relate to a walking distance of 500–1000 m. It seems that patients who were used to managing a knee prosthesis before surgery could adapt better to the post-operative situation than primary cases. This may be due to a pre-existing change in biomechanics, as can sometimes be found after TKA. Pain reduction after implantation is an essential aim in TKA.16 Surprisingly, patients after primary implantation and patients after revision procedures showed almost similar results on the VAS. The same applied to the ROM. A significant improvement in walking distance, as well as in the ability to climb stairs, was achieved postoperatively in both groups. However, patients should be informed that they may have to use crutches or walking frames for a long period of time after surgery. It does seem to be possible to achieve good clinical results after revision procedures. However, there is a higher risk of implant failure because a significantly higher revision rate for rotating-hinged knee prosthe-ses was seen in patients after implantation in revision procedures.
Rotating-hinge knee prostheses may be an option as a primary implant in older patients. These prostheses could be suited for the deformed and malaligned knee with severe bony and ligamentous defects. Most of the patients in the present study were 70 years old or over at the time of surgery. This may explain the progressive deformities of the affected knees at the time of primary implantation or the revision situation after primary prosthetic surgery. However, we agree with other authors that, due to considerable constraints, the decision to use hinged prostheses requires careful consideration.1 The use of long-stem cemented prostheses in younger patients should be considered only in selected complex cases. Patients should be informed about the risks and possible consequences of implantation of rotating-hinge knee prostheses in revision situations. The surgical options in cases of revision are clearly limited: arthrodesis or even amputation may be the only options in some cases.
The outcome of the rotating-hinge TKA has been evaluated in several studies. Barrack et al.5 reported promising results in a study comprising 23 cases of revision TKA using different types of hinged-knee prostheses over 2–9 years. Results were comparable with those of standard primary TKAs (although the cases were much more complex). Pradhan et al.17 found satisfying clinical results after a mean follow up of 48 months in 51 cases of revision using Endo-Model hinged-knee prostheses. Improvements in ROM, stability and pain could be noted for patients who underwent revision for infection or aseptic loosening (with better results being observed in patients with aseptic loosening). Joshi et al.18 made similar findings in 78 cases of revision for aseptic loosening using the Endo-Model with a mean follow up of 94 months. Seventy-three percent of patients showed excellent results with a ROM up to 0/0/104°. Yang et al.1 evaluated the long-term outcome of primary TKA using the Endo-Model rotating-hinge prosthesis. Overall, the rotating-hinge total knee prosthesis provided substantial improvement in function and pain reduction. Besides these favorable findings at final follow up, 7 (14%) deep infections were observed. The rate of implant survivorship of the Endo-Model rotating-hinge prosthesis used in the present study has been reported to be between 89.2–96.1% after a follow up of 6–20 years.3,8,19,20 Even if the results of the various studies are favorable, routine implantation of the rotating-hinge prosthesis cannot be supported if condylar prosthesis can be implanted. The risk of loosening due to bone resection after primary implantation increases, as does the risk of bone loss after explantation.18 Infections seem to be much more common after revision procedures. Inglis and Walker found infection rates of approximately 20% after failed revisions of hinged prostheses.21 Infection was also the main reason for the relatively high rates of implant failure in the present study.
One weakness of the present study was that many patients were lost to follow up, mainly due to death and medical conditions that prevented objective evaluation of the status of their knee arthroplasty. Our department is the regional referral center. This leads to a concentration of severe cases in terms of the affected joint as well as other comorbidities (e.g. severe cardiovascular disease, hypertension, vascular disease, pulmonary disease). The severity of concomitant diseases in the patient population is also reflected in high rates of mortality and care dependency at follow up. Felson et al.22 showed that 26.9% of the population died before follow up (mean 8.1 years) in the Framingham Osteoarthritis study. Another possible weakness is that long-term follow-up results may be more favorable. However, as mentioned above, due to the severity of concomitant diseases in the patient population, evaluation of mid-term results was undertaken so as to include the largest number of subjects, a proportion of which would inevitably be lost at long-term review.
Conclusions
The results of the present study suggest that rotating-hinge knee prostheses are also suitable in selected cases of difficult primary osteoarthritis with deformed or malaligned knees with severe bone and ligament defects if non-hinged implants cannot restore a satisfactory aligned and balanced knee joint. They also provide good results in revision situations. However, the failure rate was significantly higher in cases of revision surgery.
Acknowledgments:
the authors thank Dr. Johanna Schmitt for proofreading the manuscript.
References
- 1.Yang JH, Yoon JR, Oh CH, Kim TS. Primary total knee arthroplasty using rotating-hinge prosthesis in severely affected knees. Knee Surg Sports Traumatol Arthrosc. 2012;20:517–23. doi: 10.1007/s00167-011-1590-1. [DOI] [PubMed] [Google Scholar]
- 2.Kurtz S, Mowat F, Ong K, et al. Prevalence of primary and revision total hip and knee arthroplasty in the United States from 1990 through 2002. J Bone Joint Surg Am. 2005;87:1487–97. doi: 10.2106/JBJS.D.02441. [DOI] [PubMed] [Google Scholar]
- 3.Papachristou G. Experience with knee arthroplasty. Clin Orthop Relat Res. 1989:81–5. [PubMed] [Google Scholar]
- 4.Hernandez-Vaquero D, Sandoval-Garcia M. Hinged total knee arthroplasty in the presence of ligamentous deficiency. Clin Orthop Relat Res. 2010:1248–53. doi: 10.1007/s11999-009-1226-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Barrack RL. Evolution of the rotating hinge for complex total knee arthroplasty. Clin Orthop Relat Res. 2001:292–9. doi: 10.1097/00003086-200111000-00038. [DOI] [PubMed] [Google Scholar]
- 6.Bistolfi A, Massazza G, Rosso F, Crova M. Rotating-hinge total knee for revision total knee arthroplasty. Orthopedics. 2012;35:e325–30. doi: 10.3928/01477447-20120222-34. [DOI] [PubMed] [Google Scholar]
- 7.Hossain F, Patel S, Haddad FS. Midterm assessment of causes and results of revision total knee arthroplasty. Clin Orthop Relat Res. 2010;468:1221–8. doi: 10.1007/s11999-009-1204-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Petrou G, Petrou H, Tilkeridis C, et al. Medium-term results with a primary cemented rotating-hinge total knee replacement. A 7- to 15-year follow-up. J Bone Joint Surg Br. 2004;86:813–7. doi: 10.1302/0301-620x.86b6.14708. [DOI] [PubMed] [Google Scholar]
- 9.Guenoun B, Latargez L, Freslon M, et al. Complications following rotating hinge Endo-Modell (Link) knee arthroplasty. Orthop Traumatol Surg Res. 2009;95:529–36. doi: 10.1016/j.otsr.2009.07.013. [DOI] [PubMed] [Google Scholar]
- 10.Neumann D, Hofstaedter T, Dorn U. Follow-up of a modular rotating hinge knee system in salvage revision total knee arthroplasty. J Arthroplasty. 2012;27:814–9. doi: 10.1016/j.arth.2011.08.015. [DOI] [PubMed] [Google Scholar]
- 11.Willing R, Kim IY. Design optimization of a total knee replacement for improved constraint and flexion kinematics. J Biomech. 2011;44:1014–20. doi: 10.1016/j.jbiomech.2011.02.009. [DOI] [PubMed] [Google Scholar]
- 12.Fuchs S, Sandmann C, Gerdemann G, et al. Quality of life and clinical outcome in salvage revision total knee replacement: hinged vs total condylar design. Knee Surg Sports Traumatol Arthrosc. 2004;12:140–3. doi: 10.1007/s00167-003-0401-8. [DOI] [PubMed] [Google Scholar]
- 13.Insall J, Dorr L, Scott R, Scott W. Rationale of the Knee Society clinical rating system. Clin Orthop Relat Res. 1989;248:13–4. [PubMed] [Google Scholar]
- 14.Lequesne MG, Mery C, Samson M, Gerard P. Indexes of severity for osteoarthritis of the hip and knee. Validation: value in comparison with other assessment tests. Scand J Rheumatol Suppl. 1987;65:85–9. doi: 10.3109/03009748709102182. [DOI] [PubMed] [Google Scholar]
- 15.Fuchs S, Friedrich M. [Effect of patient age on use of the knee joint score] Z Orthop Ihre Grenzgeb. 1999;137:322–9. doi: 10.1055/s-2008-1039719. [Article in German] [DOI] [PubMed] [Google Scholar]
- 16.Dieppe P. Recommended methodology for assessing the progression of osteoarthritis of the hip and knee joints. Osteoarthritis Cartilage. 1995;3:73–7. doi: 10.1016/s1063-4584(05)80040-8. [DOI] [PubMed] [Google Scholar]
- 17.Pradhan NR, Bale L, Kay P, Porter ML. Salvage revision total knee replacement using the Endo-Model rotating hinge prosthesis. Knee. 2004;11:469–73. doi: 10.1016/j.knee.2004.03.001. [DOI] [PubMed] [Google Scholar]
- 18.Joshi N, Navarro-Quilis A. Is there a place for rotating-hinge arthroplasty in knee revision surgery for aseptic loosening? J Arthroplasty. 2008;23:1204–11. doi: 10.1016/j.arth.2007.10.016. [DOI] [PubMed] [Google Scholar]
- 19.Gudnason A, Milbrink J, Hailer N. Implant survival and outcome after rotating-hinge total knee revision arthroplasty: a minimum 6-year follow-up. Arch Orthop Trauma Surg. 2011;131:1601–7. doi: 10.1007/s00402-011-1330-5. [DOI] [PubMed] [Google Scholar]
- 20.Nieder E. [Sled prosthesis, rotating knee and hinge prosthesis: St. Georg model and ENDO-model. Differential therapy in primary knee joint arthroplasty.] Orthopade. 1991;20:170–80. [Article in German] [PubMed] [Google Scholar]
- 21.Inglis A, Walker P. Revision of failed knee replacements using fixed-axis hinges. J Bone Joint Surg. 1991;73:757–61. doi: 10.1302/0301-620X.73B5.1894661. [DOI] [PubMed] [Google Scholar]
- 22.Felson DT, Zhang Y, Hannan MT, et al. The incidence and natural history of knee osteoarthritis in the elderly. The Framingham osteoarthritis study. Arthritis Rheum. 1995;38:1500–5. doi: 10.1002/art.1780381017. [DOI] [PubMed] [Google Scholar]


