Abstract
Aims
The goals of the study were to describe the transition of youth with Type 1 diabetes from paediatric to adult healthcare services, examine the link of this transition with self care and glycaemic control, and distinguish youth who received medical treatment from different physicians in terms of demographic and parent relationship variables.
Methods
Youth with Type 1 diabetes (n = 118) were enrolled in a prospective study that examined the transition from the paediatric to adult healthcare systems and were evaluated during their senior year of high school (time 1) and 1 year later (time 2). Data on self care, glycaemic control and parent relationship were collected.
Results
The majority of youth saw a paediatric endocrinologist at both assessments (n = 64); others saw an adult care physician at both assessments (n = 26) or transitioned from a paediatric endocrinologist to an adult care physician (n = 19). Nine youth saw no physician between time 1 and time 2. There were group differences in demographic and parent relationship variables and self-care behaviour and glycaemic control related to the transition of care. Youth who remained in the paediatric healthcare system had the best self care and did not experience declines in glycaemic control over time.
Conclusions
Early transition from the paediatric healthcare system to the adult healthcare system is associated with psychosocial variables and worse glycaemic control. Future research should identify factors that determine optimal timing and strategies to avoid deterioration of care and control during this transition.
Introduction
Transition of adolescents and young adults from paediatric health care to adult health care has been recognized as an important and difficult transition for decades [1–4]. This transition is difficult in part because of gaps in care and in part because of differences in the approach to health care and support provided in paediatric and adult settings [5]. Paediatric services are more likely to provide integrated services and supports, whereas adult services more often rely on patient initiative to make decisions about following through on medical advice [3]. Thus, the transition from paediatric to adult care settings represents a formidable change in healthcare delivery for adolescents and emerging adults with chronic illness, and may be particularly challenging for those with Type 1 diabetes, an illness requiring a high level of patient involvement and self care.
A recent position statement by the American Diabetes Association and other interested groups has described this transition as ’a high-risk period for a person with diabetes, a perfect storm during which interruption of care is likely for multiple reasons‘ [3]. The transition from paediatric to adult health care may coincide with other life transitions that could interfere with engagement in the healthcare system. Youth may be moving away from home, pursuing employment or post-secondary education and exploring other aspects of adult life, such as significant romantic relationships. These normative transitions add to the complexity of emerging adulthood for youth with diabetes and may contribute to difficulties in healthcare transitions. In addition, older adolescents begin to take on increasing responsibility for diabetes care and parents reduce their role in everyday diabetes tasks [6]. Although skilled in many aspects of diabetes management, adolescents and emerging adults do not have the same level of sophistication at navigating the healthcare system as do their parents and may not even have much experience with basic tasks such as scheduling their own medical appointments. The transition from paediatric to adult care also may coincide with a loss of health insurance coverage and an increase in financial barriers to healthcare access [7].
Although there is consensus that the transition from paediatric to adult care is challenging, little work has described the outcomes experienced by individuals as they navigate this transition [8]. A few retrospective studies indicate that the frequency of clinic visits decreases after the transition to adult care [9–12] and some evidence suggests that infrequent clinic visits are associated with poor glycaemic control [13]. Although concerns have been raised about the implications of the transition for glycaemic control [5,14], few studies have systematically investigated this issue [3,12,15]. Although it did not specifically focus on the care transition, one longitudinal study followed adolescents into early adulthood and found an increased rate of diabetes complications, behavioural problems and increased psychiatric disorders in the following decade [16,17], suggesting that the period in which care transitions occur is associated with negative outcomes. It also is not well documented whether patients transition to adult endocrinology providers or primary care physicians [11,18]. Given the differing levels of expertise and availability of a diabetes care team between endocrinologists and primary care physicians, this choice may have a substantial impact on later diabetes outcomes (19).
The current study has three goals. First, we describe the transition from paediatric to adult healthcare services among a sample of youth with Type 1 diabetes at the onset of emerging adulthood (i.e. high school graduation), documenting physician specialty and transition timing. Second, we examine the link of this transition to self-care behaviour and glycaemic control. Third, we distinguish youth who see different kinds of physicians by demographic characteristics and relationships with parents. There are likely to be demographic and psychosocial variations in patients who change providers at different points in time.
Participants and methods
Study design
We conducted a prospective study of youth from a single paediatric diabetes centre in the USA. Adolescents with Type 1 diabetes were recruited from a previous study that was conducted with patients from the Children’s Hospital of Pittsburgh in 2002–2004 to assess the effects of psychosocial variables on successful progression through adolescence (see Helgeson et al. [20] for details). After receiving signed consent forms by post, we sent participants a questionnaire to complete in the spring of their senior year of high school [time 1 (T1)] and again 1 year later [time 2 (T2)]. If youth were under the age of 18 years, parents provided written consent and youth provided assent. When youth reached 18 years of age, they were re-consented. The majority of participants used an online questionnaire at T1 (86%) and at T2 (89%); the remainder completed a written version sent by post.
The paediatric diabetes centre from which youth were recruited does not have a formal time of transition to adult care. The general philosophy is to offer continued Children’s Hospital of Pittsburgh care until their permanent domicile has been determined (usually after college graduation or when they have a job). However, physicians and educators introduce the issue of transition during the later teen years and work on increasing independence in terms of self care over a period of time on a case-by-case basis. Group education classes are provided during the time of transition and efforts are made to link youth with an appropriate diabetes adult care provider.
At each study time point, participants indicated whether they had seen a physician for their diabetes care in the past year and, if so, they provided the name of their physician. We contacted all of these physicians to verify that the patient had been seen in the past year and to obtain the HbA1c value, if it was measured. For patients who remained at the Children’s Hospital of Pittsburgh, HbA1c was measured by HPLC (Tosoh Instruments, XXXXX, XXXX), with a normal range of 4.6–6.1%. Other patients saw physicians from a variety of practices; thus, measurement of HbA1c varied. In general, the measurement of HbA1c from these other laboratories used methods that were comparable with, or if anything ≥ 0.5 lower than, the Children’s Hospital of Pittsburgh assay [e.g. Quest Laboratories (XXXXX, XXXX, XXX) or DCA (XXXXX, XXXX XXXX) point of care]. Thus, the present analysis is conservative in testing whether youth who leave the Children’s Hospital of Pittsburgh have higher HbA1c levels than those who remain in paediatric care.
The questionnaire included a number of psychosocial variables, one of which was a self-report measure of self care, the 14-item Self Care Inventory [21,22]. The instrument has high internal consistency and test–retest reliability, and is related to interview-based measures of adherence and good glycaemic control [22]. Respondents were asked how well they followed their physician’s recommendations for glucose testing, insulin administration, diet, exercise and other diabetes-related behaviours. Each item is rated on a 1 (never do it) to 5 (always do this as recommended) scale. We updated this scale by adding eight more contemporary items (e.g. made up blood test results, skipped meals), as described in Helgeson et al. [23]. The internal consistency for this study was good at T1 (α = 0.84) and T2 (α = 0.88). The self-care index was not significantly related to glycaemic control at T1 (r = −0.15, P = 0.14), but was at T2 (r = − 0.39, P < 0.001).
We also measured several characteristics of the parent–child relationship to see if these were related to the physician seen for diabetes care. We administered three of Kerr and Statin’s [24] scales: child disclosure of daily activities, child disclosure of feelings, and parental monitoring. Because the three variables were highly correlated at each assessment (r values ranged from 0.63 to 0.78), we standardized the scores and created a composite index of parental involvement in the child’s life at T1 (α = 0.94) and T2 (α = 0.93).
Statistical analysis
We categorized youth into groups based on who they saw for their diabetes care at T1 and T2 (described below). We used χ2 and analysis of variance to compare these groups on T1 background variables. To determine how self care and glycaemic control changed over time as a function of physician group, we used repeated-measures analyses of variance. We used three time points in these analyses. In addition to T1 and T2, we used the last year that youth participated in the previous study (referred to as T0) as a comparison [20]. At T0, participants were on average 16.2 years old and in their second year of high school. At T0, nearly all (91%) participants were seeing a paediatric endocrinologist, whereas by T1 22% of participants had transitioned. We also used analysis of variance to compare the groups on parent relationships variables. Finally, we calculated the age at which participants transferred from a paediatric to an adult care physician and correlated that variable with diabetes outcomes. For participants who had not made the transfer, we used their T2 age as the age at transition rather than exclude them from the analysis.
Ethical approval
The study was approved by the Institutional Review Boards of Carnegie Mellon University and the University of Pittsburgh and complies with the 1964 Declaration of Helsinki recommendations.
Results
Sample characteristics
Of the 132 children who participated in the previous study, 127 agreed to be contacted, but five dropped out of the study and four missed one of the assessments, leaving a final sample size of 118. The average HbA1c was 74 mmol (8.9%) at T1.
Physician groups
We examined the type of physician participants saw at T1 and T2 and developed four groups: group 1 saw a paediatric endocrinologist at both T1 and T2 (‘paediatric‘; n = 64); group 2 saw an adult services physician (adult endocrinologist, primary care physician) at T1 and T2 (‘adult services‘; n = 26); group 3 saw a paediatric endocrinologist at T1, but switched to adult services at T2 (‘transition‘; n = 2); group 4 saw a physician at T1 but saw no physician at T2 (‘no physician‘; n = 9).
Physician group comparisons on background variables
In terms of T1 background variables, there were no differences between the four groups on participant sex, household structure, duration of diabetes or insulin delivery method (pump vs. injection; see Table 1). There were group differences on age (F3,114 = 4.15, P < 0.01, ηp2 = 0.10; race, χ23 = 12.37, P < 0.01) and a trend on social status (as measured by the Hollingshead index [25]) (F3,114 = 2.22, P = 0.09; ηp2 = 0.06). The adult services group was significantly older than the paediatric group, was less likely to be white than the paediatric or transition groups and had marginally lower social status than the paediatric group, as shown in Table 1.
Table 1.
Demographic characteristics at time 1 (T1) (n = 118)
| Paediatric | Adult services | Transition | No physician | ||
|---|---|---|---|---|---|
| n = 64 | n = 26 | n = 19 | n = 9 | ||
| % or mean (SD) | % or mean (SD) | % or mean (SD) | % or mean (SD) | ||
| Sex (female) | 55% | 50% | 58% | 33% | NS |
| Race (white) | 97% | 77% | 100% | 89% | * |
| Social status | 44.76 (11.36) | 38.58 (10.60) | 40.71 (10.19) | 42.39 (9.08) | † |
| Household structure (lives with mother and father) | 80% | 69% | 90% | 56% | NS |
| Age | 18.05 (0.36) | 18.37 (0.48) | 18.20 (0.29) | 18.09 (0.48) | * |
| Insulin delivery method (pump) | 67% | 42% | 63% | 44% | NS |
| Diabetes duration | 11.39 (3.10) | 10.54 (3.22) | 11.43 (2.89) | 9/71 (2.59) | NS |
Xxxxxxxxxxxxxxx.
Xxxxxxxxxxxxxxx.
NS, not significant.
We also compared the four groups on baseline (T0) measures of self care and glycaemic control. There were no group differences in self care, but there was a group difference in HbA1c (F3,111 = 5.98, P = 0.001; ηp2 = 0.14). The paediatric group had a significantly lower HbA1c [M = 67 mmol (8.32%)] than the adult services group [M = 85 mmol (9.96%)] at baseline. The transition group and the no physician group fell between the two [M = 74 mmol (8.94%) and 80 mmol (9.44%), respectively] and did not significantly differ from either.
We conducted the analyses below on self care and glycaemic control with and without controls for age, social status and race, as these demographic variables could account for group differences in diabetes outcomes. We omitted the no physician group from these analyses as this group did not have a measure of glycaemic control at T2.
Group comparisons on self care and glycaemic control
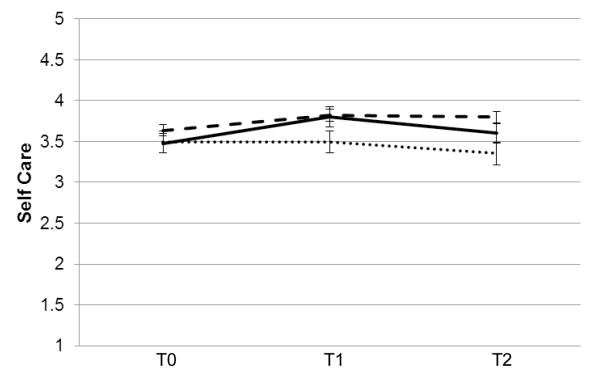
Repeated measures analysis of variance on self-care behaviour revealed a main effect of time (F2,99 = 5.93, P < 0.005, ηp2 = 0.11) and a main effect of physician group (F2,100 = 3.49, P < .05, ηp2 = 0.07). The time by physician group interaction was not statistically significant (F4,200 = 1.88, P = 0.12, ηp2 = 0.04). When we controlled for age, race and social status, only the effect of physician group remained (F2,97 = 3.03, P = 0.05, ηp2 = 0.06). As shown in Fig. 1, the paediatric group has the best self care and seems to improve with time, whereas the transition group deteriorates over time.
Figure 1.
Changes in self care over time for paediatric (n = 62, 97%; - - - - ), adult services (n = 24, 92%; –– ––) and transition (n = 17, 89%; ·······) groups.
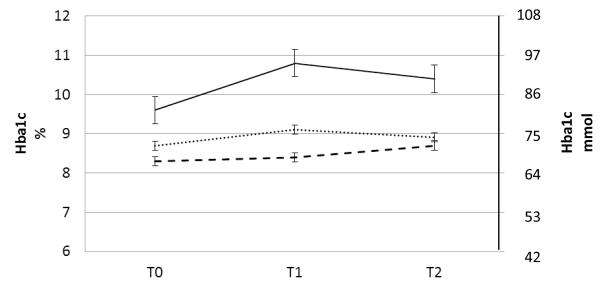
Repeated-measures analysis of variance on glycaemic control revealed a main effect of time (F2,82 = 3.98, P < 0.05, ηp2 = 0.09), a main effect of physician group (F2,83 = 11.64, P < 0.001, ηp2 = 0.22) and an interaction between physician group and time (F4,166 = 2.73, P < 0.05, ηp2 = 0.06). When we controlled for age, race and social status, the main effect of time disappeared, but the main effect of physician group (F1,80 = 8.02, P = 0.001, ηp2 = 0.17) and the interaction between time and physician group remained (F4,160 = 2.47, P < 0.05, ηp2 = 0.06). As shown in Fig. 2, all groups showed some increases in HbA1c over time, but the adult services group showed the largest increase and remained much higher than the paediatric group or the transition group at T2.
Figure 2.
Changes in glycaemic control over time for paediatric (n = 62, 97%; - - - - - ), adult services (n = 10, 36%; ––––– ) and transition (n = 14, 74%; ·······) groups.
The analyses for glycaemic control are limited because some patients saw a physician but did not have a measure of HbA1c. As shown in Fig. 2, 97% of the patients in the paediatric group had an HbA1c at all three assessments compared with 36% of the patients in the adult services group and 74% of the patients in the transition group. The group difference in complete HbA1c assessment was significant (χ22 = 38.27, P < 0.001).
Group differences on other variables
To determine if we could further distinguish participants who were in these four groups, we examined what participants were doing at T2. We examined college attendance and living situation. There was a marginally significant group difference on college attendance (χ23 = 6.41, P = 0.09. Whereas 84% of the transition group and 81% of the paediatric group were attending college full-time, only 62% of the adult services group and 56% of the no physician group were enrolled in college full-time. There was a significant difference in living situation at T2 (χ23 = 13.08, P < 0.05). Similar percentages of each group were likely to be living at home (range 35–44%), but more of the adult services group and no physician group lived on their own in an apartment (20 and 22%, respectively) compared with the paediatric and transition groups (2 and 6%)—because the latter two groups were more likely to be living on a college campus.
We also examined the parent involvement index. There was a group difference at T1 (F1,110 = 6.06, P = 0.001, ηp2 = 0.14), such that parents were significantly more involved with the paediatric group (M = 3.66) than the transition group (M = 2.82), with the other two groups falling between the two (adult services group: M = 3.24; no physician: M = 3.46). Similar findings appeared at T2. Although the overall effect was significant (F1,113 = 2.75, P < 0.05, ηp2 = 0.07), the contrasts between groups were not significant.
Age at transition
Another way to examine transitioning from paediatric to adult health care is to identify the age at transition. Younger age at transition was correlated with poorer glycaemic control at T1 (r = −0.38, P < 0.001) and at T2 (r = −0.34, P < 0.001). Age at transition was unrelated to the self-care behaviour index at T1 and T2.
Age at transition was unrelated to the demographic variables shown in Table 1 and unrelated to college attendance and parent involvement.
Discussion
The study was designed to prospectively follow patients who were part of a longitudinal study from one centre to assess factors that affect glycaemic control and self-care behaviour over the transition to emerging adulthood. These results show that youth who choose to remain in the paediatric healthcare system for a longer period of time seem to be protected from the deterioration in self care and glycaemic control that youth who transition out of paediatric services experience. It was not the group who transitioned to adult healthcare services after high school who were at the greatest risk for poor glycaemic control, but the group who transitioned to adult healthcare services before they graduated from high school. Thus, these data do not show that the transition in and of itself is inevitably linked to deterioration in glycaemic control, but rather that an earlier age at transition is associated with poorer glycaemic control.
The adult services group was distinct from the other groups in terms of several demographic variables. Youth in the adult services group were modestly older (about 2 months), more likely to be non-white, had lower social status, were less likely to be full-time college students and more likely to be living on their own 1 year after high school graduation.
The adult services group also was distinct from the paediatric and transition groups in that they had a poorer HbA1c at baseline and were much less likely to have an HbA1c tested at each assessment. We do not know whether their physicians were less likely to order an HbA1c or whether patients did not comply with the order. Although both the adult services and transition groups were seeing an adult physician at T2 (by definition), the transition group was more likely to be seeing an adult endocrinologist [16 of 19 (84%)] than the adult services group [14 of 26 (54%)]. Adult endocrinologists may place more importance on the HbA1c test than primary care physicians. We did not have a large enough sample to explore differences between adult endocrinologist and primary care physician care.
The paediatric group was distinct from the other groups in terms of parent involvement, even at baseline. Those who remained in the paediatric system had parents who were more involved in their everyday life. Although adolescence and emerging adulthood is typically regarded as a time in which youth separate from parents, the data from this study are consistent with previous research in showing that connections to parents continue to be important and that parent support and involvement in youth’s lives continues to be protective during emerging adulthood [26,27]. In fact, it may be that youth who have more involved parents prefer to remain in the paediatric healthcare system. These youth may be more receptive to the structured guidance of paediatric care. We speculate that these youth will do well when they transfer to an adult care provider, in part because of their strong connections to family and in part because of the fact that they will have had additional time to prepare themselves for the transition.
We must note the serious concern that nine youth with Type 1 diabetes did not see a physician for their diabetes care during the past year. The number of persons in this group was not large enough to statistically distinguish it from the other groups in terms of demographic variables, but it appeared as if they were more similar to the adult services group. Although we were unable to examine their glycaemic control, we are concerned that they are in poor control and at risk for future diabetes complications. Their HbA1c at T0 was 80 mmol (9.4%), similar to the adult services group—a group that ended up deteriorating over time. Researchers need to explore the barriers that keep older adolescents and emerging adults with Type 1 diabetes from seeing a physician.
The aim of the study was to assess the factors that influence diabetes care and glycaemic control during the transition to emerging adulthood. Because participants were not randomly assigned to different avenues of clinical care, it is not possible to determine whether the differences in demographics and family relations among the groups or the effects of the transfer of care led to the subsequent outcomes. Youth who are having difficulties with diabetes and family relations may be the most likely to leave the paediatric healthcare system and to do so at an earlier time. The recruitment from a single diabetes centre is a strength of the study because we were able to examine how youth who received similar treatment at study outset fare at a later period of time when one group remains at the centre and other groups do not. The use of a single centre, however, limits the generalizability of our findings. Future research in this area should examine this issue across multiple centres and possible standardize intervention strategies across centres.
We also note that this study only captures 1 year into the transition—albeit an important one, as high school graduation signifies the onset of emerging adulthood [28] and many of these youth are leaving home for the first time. During this year, a small number of youth made the transition from paediatric to adult care. Over the coming years, additional youth will make this particular transition, and those who have recently made the change will have greater opportunity to adjust to their new clinical care.
Despite these caveats, this is one of the few prospective studies to examine how youth fare as they transition from paediatric to adult services. We view these data as preliminary and in need of replication. These data showed that an early transfer from the paediatric healthcare system to the adult healthcare system is associated with deterioration in glycaemic control. Youth who are most likely to transfer to adult services during high school are characterized by lower social status, non-white race, lower likelihood of pursuing college after high school graduation and lower levels of parent involvement in their daily lives. Thus, we are unable to distinguish whether it is the transition itself, these other factors or some combination of the two that are associated with deteriorated glycaemic control.
Acknowledgements
We appreciate the assistance of the research assistants at Carnegie Mellon University, Abigail Kunz and Jamie Vance, who helped to collect these data.
Funding sources This research was supported by National Institutes of Health (NIH) R01 DK060586.
Footnotes
Competing interests None declared.
References
- 1.Blum RW, Garell D, Hodgman C. Transition from child-centered to adult health care systems for adolescents with chronic conditions: a position paper of the Society for Adolescent Medicine. J Adolesc Health. 1993;14:570–576. doi: 10.1016/1054-139x(93)90143-d. [DOI] [PubMed] [Google Scholar]
- 2.American Academy of Pediatrics. American Academy of Family Physicians. American College of Physicians. American Society of Internal Medicine A consensus statement on health care transitions for young adults with special health care needs. Pediatrics. 2002;110:1304–1306. [PubMed] [Google Scholar]
- 3.Peters A, Laffel L. Diabetes care for emerging adults: recommendations for transition from pediatric to adult diabetes care systems. Diabetes Care. 2011;34:2477–2485. doi: 10.2337/dc11-1723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Betz CL. Transition of adolescents with special health care needs: review and analysis of the literature. Issues Compr Pediatr Nurs. 2004;27:179–241. doi: 10.1080/01460860490497903. [DOI] [PubMed] [Google Scholar]
- 5.Fleming E, Carter B, Gillibrand W. The transition of adolescents with diabetes from the children’s health care service into the adult health care service: a review of the literature. J Clin Nurs. 2002;11:560–567. doi: 10.1046/j.1365-2702.2002.00639.x. [DOI] [PubMed] [Google Scholar]
- 6.Anderson BJ, Ho J, Brackett J, Finkelstein D, Laffel L. Parental involvement in diabetes management tasks: relationships to blood glucose monitoring adherence and metabolic control in young adolescents with insulin-dependent diabetes mellitus. J Pediatr. 1997;130:257–265. doi: 10.1016/s0022-3476(97)70352-4. [DOI] [PubMed] [Google Scholar]
- 7.Willoughby LM, Fukami S, Bunnapradist S, Gavard JA, Lentine KL, Hardinger KL, et al. Health insurance considerations for adolescent transplant recipients as they transition to adulthood. Pediatr Transplant. 2007;11:127–131. doi: 10.1111/j.1399-3046.2006.00639.x. [DOI] [PubMed] [Google Scholar]
- 8.Pai ALH, Ostendorf HM. Treatment adherence in adolescents and young adults affected by chronic illness during the health care transition from pediatric to adult health care: a literature review. Child Health Care. 2011;40:16–33. [Google Scholar]
- 9.Sparud-Lundin C, Ohrn I, Danielson E, Forsander G. Glycaemic control and diabetes care utilization in young adults with Type 1 diabetes. Diabet Med. 2008;25:968–973. doi: 10.1111/j.1464-5491.2008.02521.x. [DOI] [PubMed] [Google Scholar]
- 10.Kipps S, Bahu T, Ong K, Ackland FM, Brown RS, Fox CT, et al. Current methods of transfer of young people with Type 1 diabetes to adult services. Diabet Med. 2002;19 doi: 10.1046/j.1464-5491.2002.00757.x. XX–XX. [DOI] [PubMed] [Google Scholar]
- 11.Busse FP, Hiermann P, Galler A, Stumvoll M, Wiessner T, Kiess W, et al. Evaluation of patients’ opinion and metabolic control after transfer of young adults with type 1 diabetes from a pediatric diabetes clinic to adult care. Horm Res. 2007;67:132–138. doi: 10.1159/000096583. [DOI] [PubMed] [Google Scholar]
- 12.Nakhla M, Daneman D, Frank M, Guttmann A. Translating transition: a critical review of the diabetes literature. J Pediatr Endocrinol Metab. 2008;21:507–516. [PubMed] [Google Scholar]
- 13.Bowen ME, Henske JA, Potter A. Health care transition in adolescents and young adults with diabetes. Clin Diabetes. 2010;28:99–106. [Google Scholar]
- 14.Kollipara S, Kaufman FR. Transition of diabetes care from pediatrics to adulthood. School Nurse News. 2008;25:27–29. [PubMed] [Google Scholar]
- 15.McGill M. How do we organize smooth, effective transfer from paediatric to adult diabetes care? Horm Res. 2002;57:66–68. doi: 10.1159/000053316. [DOI] [PubMed] [Google Scholar]
- 16.Bryden KS, Neil A, Peveler RC, Mayou RA, Stein A, Dunger DB. Clinical and psychological course of diabetes from adolescence to young adulthood. Diabetes Care. 2001;24:1536–1540. doi: 10.2337/diacare.24.9.1536. [DOI] [PubMed] [Google Scholar]
- 17.Bryden KS, Peveler RC, Dunger DB, Neil A, Mayou RA. Poor prognosis of young adults with type 1 diabetes. Diabetes Care. 2003;26:1052–1057. doi: 10.2337/diacare.26.4.1052. [DOI] [PubMed] [Google Scholar]
- 18.Neu A, Lösch-Binder M, Ehehalt S, Schweizer R, Hub R, Serra E. Follow-up of adolescents with diabetes after transition from paediatric to adult care: results of a 10-year prospective study. Exp Clin Endocrinol Diabetes. 2010;118:353–355. doi: 10.1055/s-0029-1246215. [DOI] [PubMed] [Google Scholar]
- 19.Zgibor JC, Songer TJ, Kelsey SF, Weissfeld J, Drash AL, Becker D, et al. The association of diabetes specialist care with health care practices and glycemic control in patients with type 1 diabetes. Diabetes Care. 2000;23:472–476. doi: 10.2337/diacare.23.4.472. [DOI] [PubMed] [Google Scholar]
- 20.Helgeson VS, Escobar O, Siminerio L, Becker D. Unmitigated communion and health among adolescents with and without diabetes: the mediating role of eating disturbances. Pers Soc Psychol Bull. 2007;33:519–536. doi: 10.1177/0146167206296953. [DOI] [PubMed] [Google Scholar]
- 21.La Greca AM, Swales T, Klemp S, Madigan S. Self-care behaviors among adolescents with diabetes. 9th Annual Sessions of the Society of Behavioral Medicine; City, Country, XX–XX Xxxxx XXXX. [Google Scholar]
- 22.Lewin AB, La Greca AM, Geffken GR, Williams LB, Duke DC, Storch EA, et al. Validity and reliability of an adolescent and parent rating scale of type 1 diabetes adherence behaviors: the self-care inventory. J Pediatr Psychol. 2009;34:999–1007. doi: 10.1093/jpepsy/jsp032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Helgeson VS, Reynolds KA, Siminerio L, Escobar O, Becker D. Distribution of parent and adolescent responsibility for diabetes self care: emerging impact of shared responsibility. J Pediatr Psychol. 2008;33:497–508. doi: 10.1093/jpepsy/jsm081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kerr M, Stattin H. What parents know, how they know it, and several forms of adolescent adjustment: further evidence for a reinterpretation of monitoring. Dev Psychol. 2000;36:366–380. [PubMed] [Google Scholar]
- 25.Hollingshead AB. Four Factor Index of Social Status. Yale University; New Haven: 1975. [Google Scholar]
- 26.Wood MD, Read JP, Mitchell RE, Brand NH. Do parents still matter? Parent and peer influences on alcohol involvement among recent high school graduates. Psychol Addict Behav. 2004;18:19–30. doi: 10.1037/0893-164X.18.1.19. [DOI] [PubMed] [Google Scholar]
- 27.Turner AP, Larimer ME, Sarason IG. Family risk factors for alcohol-related consequences and poor adjustment in fraternity and sorority members: exploring the role of parent–child conflict. J Stud Alcohol. 2000;61:818–826. doi: 10.15288/jsa.2000.61.818. [DOI] [PubMed] [Google Scholar]
- 28.Arnett JJ. Emerging adulthood: a theory of development from the late teens through the twenties. Am Psychol. 2000;55:469–480. [PubMed] [Google Scholar]