Introduction
Arnold Chiari malformations (ACM) are a group of anomalies with herniation of the cerebellum through the foramen magnum and downward displacement of the pons and the medulla. ACM type I (ACM-I) presents typically in adulthood with headache, pain in the neck and upper extremities, and other neurological features suggestive of increased intracranial pressure (ICP) and syringomyelia. Owing to paucity of the literature of ACM in pregnancy, no firm recommendations regarding management of labor and analgesia/anesthesia are available [1]. We describe a successful pregnancy outcome in a woman whose progressive symptoms of ACM were halted by surgical decompression in the second trimester of pregnancy.
Case Report
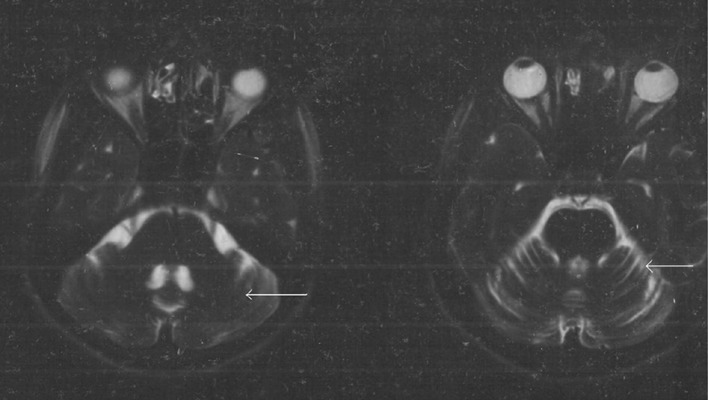
Mrs. P.D. aged 26 years (P1+0, L.I.-1, LCB-normal delivery 3 years back, LMP 25/02/08) attended antenatal OPD of our hospital at 12 weeks gestation with progressively increasing weakness of upper and lower extremities since about 1 year. On examination, she had motor weakness more in the upper than in the lower limbs with ataxic gait and without any sensory loss or higher function impairment. MRI of brain showed the descent of cerebellar tonsil and medulla (Figs. 1 and 2) through the foramen magnum favoring a diagnosis of ACM type I. She was advised decompression surgery by the neurosurgical team but she refused surgery and was lost to follow up. However, as her symptoms gradually deteriorated, she consulted another hospital (Bisuddhananda Hospital, Kolkata) where she was given the same advice. On 07/24/2008, she underwent decompression of foramen magnum with removal of posterior arch of first and second cervical vertebrae and duroplasty with gelatin patch, under general anesthesia in that hospital with perioperative tocolysis with ritordine. After the operation, she partially recovered from her motor weakness. Eventually, she turned up for antenatal care again to our hospital. An USG revealed that her gestations were corresponding to her dates and her fetus had no anomaly. Her antenatal visits were regular and uneventful other than her unstable lie which later became transverse lie at term. She received iron, folic acid, and calcium supplementation. Her motor weakness did not deteriorate further all through the rest of pregnancy. There were no other signs and symptoms of increased ICP.
Fig. 1.

Herniation of cerebellar tonsil through foramen magnum
Fig. 2.
Loss of gyri of cerebellum
She was admitted at term, and elective LSCS was planned due to transverse lie. The case was thoroughly discussed with the department of anesthesia and neurosurgery. As the patient had decompression surgery and no features of increased ICP, spinal anesthesia was planned. The unlikely possibility of tentorial herniation with bulbar compression requiring urgent surgical intervention and chances of further peripheral neurological impairment of lower limbs after spinal anesthesia was discussed with the patient by the neurosurgical team, and the patient accepted spinal anesthesia after properly understanding it. A healthy female baby of 2.7 kg was delivered by LSCS on 12/03/2008. She was administered spinal anesthesia with 27 gauze needle with hyperbaric bupivacaine and fentanyl. The procedure was uneventful. Postoperatively her neurological status was closely monitored, and there was no exacerbation. Her postoperative recovery was uneventful, and she was discharged after 7 days with her residual motor weakness of her lower limbs. She had an uneventful puerperium and had satisfactory follow up after 3 months.
Discussion
The obstetric and anesthetic management of women with ACM-I remains a dilemma as it has been scarcely reviewed because of paucity of cases, and no uniform recommendations regarding mode of delivery (vaginal vs. abdominal) and choice of anesthesia (regional vs. general) is available. Vaginal operative delivery without maternal voluntary expulsive efforts under epidural analgesia has been reported in patients of ACM-I especially in the 2nd stage of labor [2]. However, in most reviews, patients were delivered by planned LSCS. Spinal anesthesia has been safely used in most of the surgically decompressed cases of ACM-I [3].
In conclusion, this article emphasizes the importance of a multidisciplinary and individualized approach in a pregnant woman with an uncommon, non-pregnancy-specific disorder like ACM-I which an obstetrician seldom comes across.
References
- 1.Krysztof MK. Spinal anesthesia for cesarean delivery in a parturient with Arnold-Chiari type I malformation. Can J Anesth. 2004;51:639. doi: 10.1007/BF03018412. [DOI] [PubMed] [Google Scholar]
- 2.Parker JD, Broberg JC, Napolitano PG. Maternal arnold chiari type I malformation and syringomyelia : a labor management dilemma. Am J Perinatol. 2002;19:445–450. doi: 10.1055/s-2002-36841. [DOI] [PubMed] [Google Scholar]
- 3.Ruth L, Raphael G, Vincent D, et al. Spinal anesthesia for cesarean delivery in a woman with a surgically corrected type I Arnold Chiari malformation. Anesth Analg. 2003;97:253–255. doi: 10.1213/01.ane.0000066312.32029.8b. [DOI] [PubMed] [Google Scholar]