Abstract
Purpose
The most safe and effective dose of vitamin D supplementation for healthy adolescents is currently unknown. The aim of this study was to compare the efficacy of 200 IU vs. 1000 IU of daily vitamin D3 for supplementation in healthy adolescents with baseline vitamin D sufficiency.
Methods
We conducted a double-blind, randomized clinical trial. Fifty-six subjects, ages 11–19 years, with baseline vitamin D sufficiency received 1000 IU or 200 IU of daily vitamin D3 for 11 weeks. Compliance was assessed using MEMS6 Trackcaps and pill counts.
Results
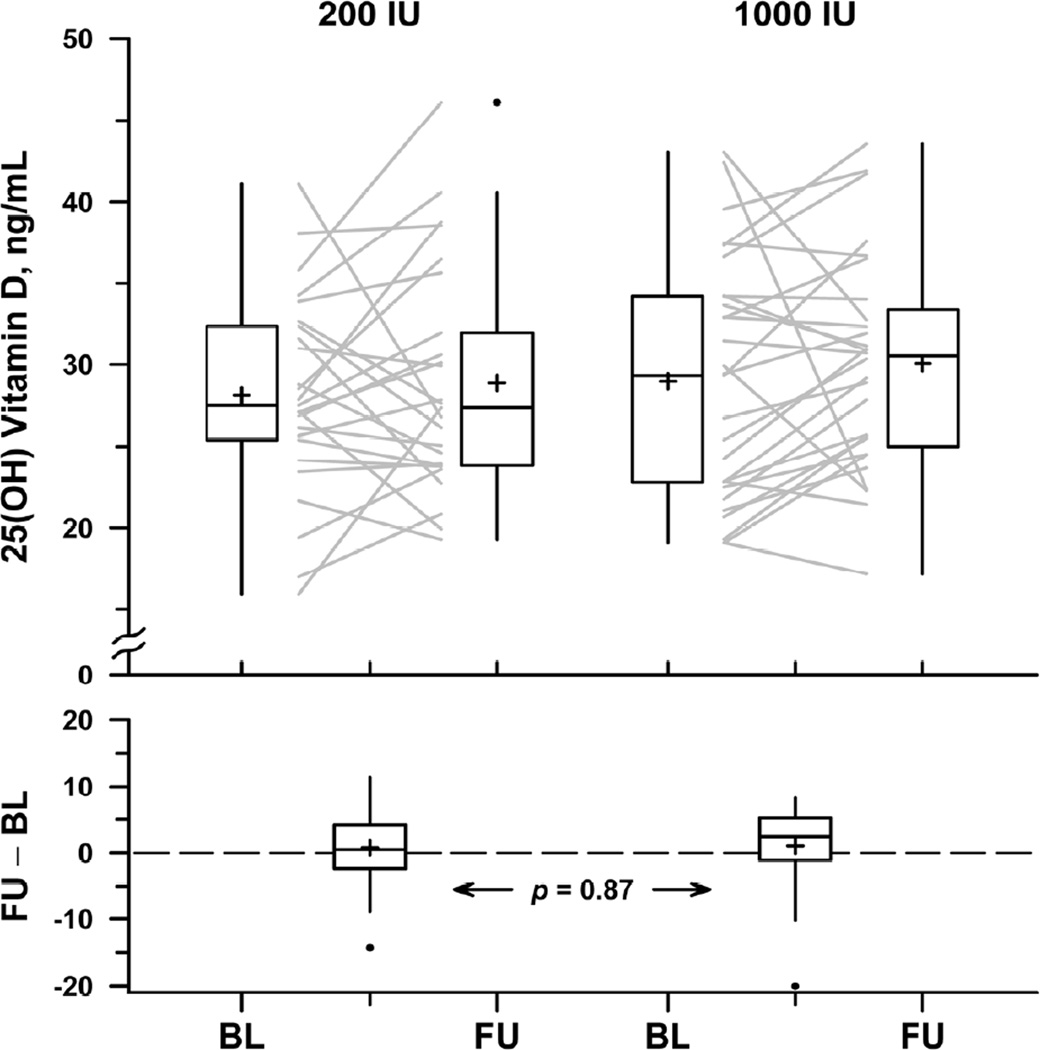
Fifty-three subjects completed the clinical trial. Subjects in the two treatment arms were similar in terms of age, race, gender, BMI, and dietary calcium and vitamin D intake. Serum 25(OH)D level in the 200 IU treatment arm was 28.1 ± 6.2 ng/mL at baseline (mean ± SD) and 28.9 ± 7.0 ng/mL at follow-up. In the 1000 IU treatment arm, 25(OH)D levels were 29.0 ± 7.3 and 30.1 ± 6.6 at baseline and follow-up, respectively. Mean change in 25(OH)D level did not differ significantly between treatment arms (p=0.87), nor did mean change in PTH, calcium, phosphate, bone turnover markers, fasting glucose, or fasting insulin.
Conclusions
In healthy adolescents with baseline vitamin D sufficiency, supplementation with vitamin D3 doses of 200 and 1000 IU for 11 weeks did not increase serum 25(OH)D levels, with no significant difference observed between treatment arms.
Keywords: Vitamin D, supplementation, adolescent, bone turnover markers
INTRODUCTION
Recent studies have shown a high prevalence of vitamin D deficiency in otherwise healthy adolescents, with varying results depending on the limit of serum 25(OH)D used to define deficiency. 1–7 These findings in young adolescents raise concern about long-term health consequences that may stem from this deficiency, especially because adolescence is a crucial time for bone accrual. Although limited, available data suggest a direct association between bone density, vitamin D supplementation, and 25(OH)D status in adolescents.8–14
Clinical trials evaluating the optimal vitamin D supplementation dose in healthy adolescents are sparse, and the recommendations for this population are controversial. When this study began, the official Institute of Medicine (IOM) Adequate Intake (AI) of vitamin D in children and adolescents was 200 international units (IU) daily.15 More recently, IOM proposed a supplemental Recommended Daily Allowance (RDA) of 600 IU daily for healthy individuals age 1–70 years.16 The American Academy of Pediatrics currently recommends vitamin D supplementation with 400 IU daily for all infants, children and adolescents.17 However, many experts suggest that a dose of 1000 IU or more daily is required to ensure adequate serum 25(OH)D levels for skeletal and overall health. 18–20 In adults, studies suggest that 100 international units of vitamin D3 increases blood level of 25(OH)D by 1 ng/mL,21,22 but studies in adolescents are lacking.
Given the limited data in the medical literature to drive the formulation of vitamin D supplementation recommendations for pediatric health providers, this study was designed to evaluate the safety and efficacy of 1000 IU vs. 200 IU of daily vitamin D3 on serum 25(OH)D levels in healthy adolescents with baseline vitamin D sufficiency (as defined by a baseline 25(OH)D level above 20 ng/mL).
SUBJECTS AND STUDY METHODS
Study Subjects
Subjects were recruited from the Boston Children’s Hospital (BCH) Adolescent Medicine Outpatient Program and from the community via flyers, internet postings, and newspaper advertisements. Enrollment began September 1, 2008 and ended March 18, 2011. To minimize variability due to ultraviolet B exposure during the summer months, enrollment was limited to September through March.
All subjects underwent screening at the BCH Clinical and Translational Study Unit (CTSU). Healthy adolescents, ages 11–19 years, were eligible if clinically stable and likely to comply with treatment. Exclusion criteria included a history of chronic disease; use of oral glucocorticoids or anticonvulsant therapy within the previous 3 months; pregnancy; BMI below the 5th or above the 95th percentile for age and sex; and any medical or psychiatric condition or situation that would compromise study participation. Serum 25(OH)D, calcium, and phosphorus levels were assessed at the screening visit. Subjects were excluded if they had baseline vitamin D deficiency or toxicity (<20 ng/mL or >100 ng/mL)23 or baseline hypo- or hypercalcemia (serum calcium <8 or >10.5 mg/dL).24
Adolescents with vitamin D deficiency at screening (<20 ng/mL) were offered treatment with 50,000 IU of vitamin D2 by mouth weekly or 2000 IU daily of vitamin D3 for 6 weeks. Following treatment, these subjects were invited to return for a second screening including re-consent and labs.
The protocol was approved by the BCH institutional review board. Subjects aged 18 years and over provided written informed consent. Younger subjects provided verbal assent, with parents providing written consent.
Study Design
This was a single-center, double-blind, randomized clinical trial. Subjects were interviewed by research staff using a survey with questions regarding nutrition, previous vitamin D supplementation, socioeconomic status, and time spent outdoors. Anthropometric data including height and weight were measured on a single scale and standiometer. Skin color was evaluated using established methods.25,26 A standardized 24-hr food record was administered at baseline by a CTSU dietician. Subjects were provided forms to collect another 48 hr of food and beverage intake at home. Baseline blood samples were obtained as detailed below.
Participants were randomly assigned in a double-blind fashion to receive 200 IU or 1000 IU of daily vitamin D3 in an oral capsule. All vitamin D3 supplements were supplied by Tishcon and assayed using HPLC to ensure dosage accuracy. Treatment lasted 11 weeks. Subjects were asked to refrain from taking other vitamin D supplements during the study. The randomization was stratified by skin color to balance light- and dark-skinned subjects in each treatment arm. The random assignments for each stratum were permuted in blocks of 2, 4, and 6 to maintain balance and ensure unpredictability.
Subjects’ compliance with treatment was assessed using MEMS6 Trackcaps, a medication event monitoring system.27,28 In addition, subjects rated their compliance at the follow-up visit, using a scale of 1 to 5 to rate how often they took the study medication.
Subjects returned for a follow-up visit within 1–2 weeks of completion of therapy. Repeat anthropometric measures were obtained and a survey was administered evaluating time spent outdoors, nutritional intake, and study medication compliance. Subjects met with a research dietician for a standardized 24 hr dietary intake review and were provided forms to collect another 48 hr of food and beverage intake at home. Blood was drawn for follow-up laboratory evaluations as detailed below.
Laboratory Studies
Screening serum 25(OH)D levels were performed by radio immunoassay (RIA) by Labcorp (Raritan, New Jersey). Baseline and follow up labs were obtained in the morning after fasting overnight and processed through the Harvard Catalyst Central Laboratory. Baseline and follow-up serum 25(OH)D levels were obtained by RIA (Diasorin, Inc., Stillwater, MN, inter-assay variation 6.2–12.5%). Parathyroid hormone (PTH) and bone specific alkaline phosphatase (BSAP) levels were obtained by Access chemiluminescent immunoassay (Beckman Coulter, Fullerton CA, inter-assay variation 2.8–5.8 and 3.3–5.9%, respectively). C-telopeptide (CTX) levels were obtained by immunoradiometric assay (Immunodiagnostic Systems, Fountain Hills, AZ, inter-assay variation 5.6–7.4%), and osteocalcin (OC) by enzyme linked immunosorbent assay (ALPCO Diagnostics, Salem, NH, inter-assay variation 4.8–5.5%). Insulin levels were obtained by Access Chemluminescent Immunoassay (Beckman Coulter, Fullerton, CA, inter-assay variation 3.1–5.6%). All serum was stored at −80°C to ensure sample integrity.
Outcome Measures
The primary outcome was the mean change in 25(OH)D levels after treatment. Secondary endpoints included the mean change in serum level of fasting glucose and insulin, PTH, calcium, alkaline phosphatase, phosphorus, bone formation (as reflected by serum BSAP and OC measurements), and bone resorption (serum CTX).
Statistical Analysis
Sample Size
The sample-size determination was based on data from our previous study in adolescents,1 in which the standard deviation of 25(OH)D was 11.2 ng/mL. A sample of 20 per arm provided 80% power to detect a treatment difference in mean change of 10 ng/mL, which we judged clinically meaningful.
Statistical Analysis
Baseline characteristics and mean changes were compared between the two supplementation arms by independent two-tailed t-tests, replaced by non-parametric comparison in cases of skewed distribution. Categorical variables were compared using Fisher’s exact test. Paired t-tests were used to assess within-group change. P=0.05 was used as critical level for statistical significance
To test for potential bias from pre-enrollment high dose vitamin D supplementation, the analysis was repeated after excluding the 13 pre-treated subjects. Multivariate analysis was performed to account for covariates including age, gender, BMI, race, sun exposure during the study period, compliance, baseline 25(OH)D level, season of enrollment, use of other vitamins during the study period, and pre-treatment with high dose ergocalciferol or other over-the-counter vitamins.
RESULTS
Enrolled Subjects
Fifty-six healthy adolescents were enrolled in this clinical trial. Two subjects who were randomized to a treatment group did not complete a baseline visit, and one subject who completed the baseline visit was subsequently lost to follow-up. Fifty-three subjects completed the study. Baseline characteristics of enrolled subjects who completed the baseline visit are presented in Table 1.
Table 1.
Characteristics of Enrolled Subjects
| 200 IU (n=25) |
1000 IU (n=29) |
p value | |
|---|---|---|---|
| Age (y) | 16.1 ± 2.2 | 16.1 ± 2.2 | 0.99 |
| Gender | 0.13 | ||
| Male | 4 (16) | 11 (38) | |
| Female | 21 (84) | 18 (62) | |
| Ethnicity | 0.74 | ||
| Hispanic | 4 (16) | 6 (21) | |
| Non-Hispanic | 21 (84) | 23 (79) | |
| Race | 0.80 | ||
| Caucasian | 10 (40) | 14 (48) | |
| African American | 4 (16) | 4 (14) | |
| Asian | 6 (24) | 4 (14) | |
| Other | 5 (20) | 7 (24) | |
| BMI (kg/m2) | 21.3 ± 2.8 | 21.5 ± 3.5 | 0.78 |
| BMI percentile (%) | 53.7 ± 28.1 | 55.4 ± 30.1 | 0.83 |
| Dietary Ca intake (mg/d) | 977 ± 487 | 930 ± 305 | 0.68 |
| Dietary Vitamin D intake (IU/d) | 160 ± 128 | 187 ± 119 | 0.43 |
| Prior vitamin D supplement use | |||
| High dose vitamin D2 treatment | 3 (12) | 10 (34) | 0.065 |
| OTC vitamin use | 9 (26) | 14 (48) | 0.42 |
| Compliance (% doses taken) | 84 ± 20 | 81 ± 28 | 0.69 |
| Season of enrollment | 0.60 | ||
| Fall | 14 (56) | 14 (56) | |
| Winter | 11 (44) | 15 (51) | |
Continuous measures are expressed as mean ± SD and compared by t-test. Discrete variables are expressed as n (%) and compared by Fisher exact test.
Subjects in the two treatment arms were similar in terms of age, gender, race (because of the stratified randomization), BMI, and socioeconomic status as reflected by self-reported annual household income and receipt of federal assistance. Self-reported sun sensitivity and tanning tendency were also similar between groups. Subjects who had been pre-treated with high dose ergocalciferol or cholecalciferol for vitamin D deficiency prior to enrollment were more frequent in the 1000 IU treatment arm, but the imbalance was not statistically significant (p=0.065).
Dietary calcium and vitamin D
Dietary intake of calcium was similar between treatment arms at both baseline (p=0.69) and at follow up (p=0.98). Treatment groups also did not vary in terms of dietary vitamin D intake at baseline (p= 0.43) and follow up (p=0.59). The adolescents in this sample consumed approximately 952 ± 398 mg/day of calcium (mean ± SD) along with 174 ± 123 IU/day of vitamin D in their diet at the baseline visit and 997 ± 477 mg/day of dietary calcium and 244 ± 190 IU/day of dietary vitamin D at the follow-up visit.
Sun exposure
Subjects were enrolled during the fall and winter months (September–March) in Boston in order to minimize the effects of sun exposure on serum 25(OH)D results. At the follow up visit, 15% of subjects reported significant sun exposure over the course of the trial period (as defined by self-report of spending more than 30 minutes outside without sunscreen with arms and legs or more exposed), a similar finding between treatment arms (p=0.82).
Compliance
Mean compliance as measured by MEMS Trackcaps was 84 ± 20% in the 200 IU group and 81 ± 28% in the 1000 IU group, a non-significant difference (p=0.69). Self-reported compliance was similarly high and was strongly correlated with MEMS Trackcaps (Pearson r = 0.68, p <0.001). The median time from final dose of vitamin D until follow up visit was 2 days in the 200 IU treatment group (range 0–20 days) and 1 day in the 1000 IU treatment group (range 0–17 days), with no significant difference between treatment groups (p=0.67).
Serum studies results
Mean serum 25(OH)D levels remained unchanged at follow-up compared to baseline in both treatment arms. (Table 2). The mean change in 25(OH)D level from baseline to follow-up was 0.7 ± 6.3 ng/mL in the 200 IU treatment group and 1.0 ± 6.0 ng/mL in the 1000 IU groups. The mean change in 25(OH)D level was not significantly different between treatment arms (p=0.87). (Figure 1). Within group change was also not significant with either dose of vitamin D supplementation (p=0.56 in the 200IU group, p=0.37 in the 1000IU group). No subject developed signs of vitamin D intoxication, as defined by hypercalcemia or a 25(OH)D level >100 ng/mL. Two subjects, one from each treatment arm, developed vitamin D deficiency over the course of the study with a serum 25(OH)D level below 20 ng/mL at the follow up visit. Of note, the subject in the 1000 IU treatment group who developed vitamin D deficiency had a low compliance rate, taking only 21% of doses.
Table 2.
Laboratory Results
| 200 IU | 1000 IU | p value |
|||||
|---|---|---|---|---|---|---|---|
| Baseline | Follow-Up | Change | Baseline | Follow-Up | Change | ||
| 25(OH)D (ng/mL) | 28.1 ± 6.2 | 28.9 ± 7.0 | 0.8 ± 6.3 | 29.0 ± 7.3 | 30.1 ± 6.6 | 1.0 ± 6.0 | 0.87 |
| PTH (pg/mL) | 39.6 ± 15.4 | 34.5 ± 16.5 | −5.2 ± 11.0 | 37.9 ± 14.0 | 36.0 ± 16.4 | −2.2 ± 11.9 | 0.35 |
| Ca (mg/dL) | 9.4 ± 0.4 | 9.5 ± 0.3 | 0.1 ± 0.4 | 9.5 ± 0.5 | 9.5 ± 0.4 | 0.0 ± 0.4 | 0.23 |
| Phos (mg/dL) | 4.3 ± 0.5 | 4.1 ± 0.6 | −0.1 ± 0.4 | 4.3 ± 0.6 | 4.3 ± 0.6 | 0.0 ± 0.5 | 0.20 |
| Mg (mg/dL) | 2.1 ± 0.1 | 2.1 ± 0.1 | 0.0 ± 0.1 | 2.0 ± 0.1 | 2.0 ± 0.1 | 0.0 ± 0.2 | 0.84 |
| Alk phos (U/L) | 127.5 ± 97.3 | 123.4 ± 85.6 | −4.1 ± 33.8 | 137.7 ± 123.7 | 140.8 ± 141.6 | 0.3 ± 26.5 | 0.60 |
| OC (ng/mL) | 24.9 ± 21.1 | 21.5 ± 15.5 | −3.4 ± 17.3 | 27.1 ± 20.5 | 34.4 ± 30.2 | 6.9 ± 19.8 | 0.15* |
| BSAP (ug/L) | 36.9 ± 37.5 | 31.1 ± 31.1 | −5.8 ± 19.0 | 36.9 ± 36.1 | 32.3 ± 32.3 | −5.7 ± 20.4 | 0.98 |
| CTX (ng/mL) | 1.61 ± 0.89 | 1.40 ± 0.84 | −0.21 ± 0.69 | 1.62 ± 0.85 | 1.74 ± 1.09 | 0.09 ± 0.79 | 0.16 |
| Insulin (uIU/mL) | 6.5 ± 2.3 | 7.3 ± 3.2 | 0.8 ± 2.7 | 5.9 ± 2.5 | 7.3 ± 2.8 | 1.3 ± 2.6 | 0.48 |
| Glucose (mg/dL) | 89.3 ± 5.0 | 87.7 ± 13.5 | −1.6 ± 12.1 | 88.5 ± 5.6 | 87.4 ± 9.3 | −1.1 ± 8.9 | 0.88 |
Data are expressed as mean ± SD. p-value tests the hypothesis of no difference in mean change between treatment groups, by independent t-test except as noted.
Skewed distributions compared by Wilcoxon rank-sum test.
Figure 1.
Serum 25(OH) vitamin D in the 200 IU treatment arm (left) and 1000 IU treatment arm (right). Each subject’s 25(OH)D levels are represented by a grey line connecting baseline (BL) with follow-up (FU). Box plots illustrate the distribution of baseline and follow-up levels (upper panel) and within-subject changes from baseline to follow-up (lower panel). Top and bottom of the box indicate quartile boundaries (25th and 75th percentiles); center belt indicates median; cross (+) indicates mean. Individual points (●) indicate outliers, falling outside the box by at least 1.5 times its height. Vertical lines extend to position of farthest non-outlier above and below the box. P-value in the lower panel tests the hypothesis that the distribution of changes is equal in the two treatment arms.
Multivariate adjustment for age, gender, BMI, race, sun exposure during the study period, compliance (as determined by MEMS Trackcaps), baseline 25(OH)D level, season of enrollment, use of other vitamins during the study period, pre-treatment with high dose ergocalciferol or other over-the-counter vitamins prior to study enrollment did not affect these results. Of these potential confounders, change in 25(OH)D level over time was significantly associated with age, prior treatment with vitamin D, compliance, season of enrollment, and baseline 25(OH)D level. In addition, statistical analysis was repeated after excluding subjects who had been previously treated for vitamin D deficiency with high dose vitamin D prior to enrollment, and no significant difference in change in serum 25(OH)D was noted (data not shown).
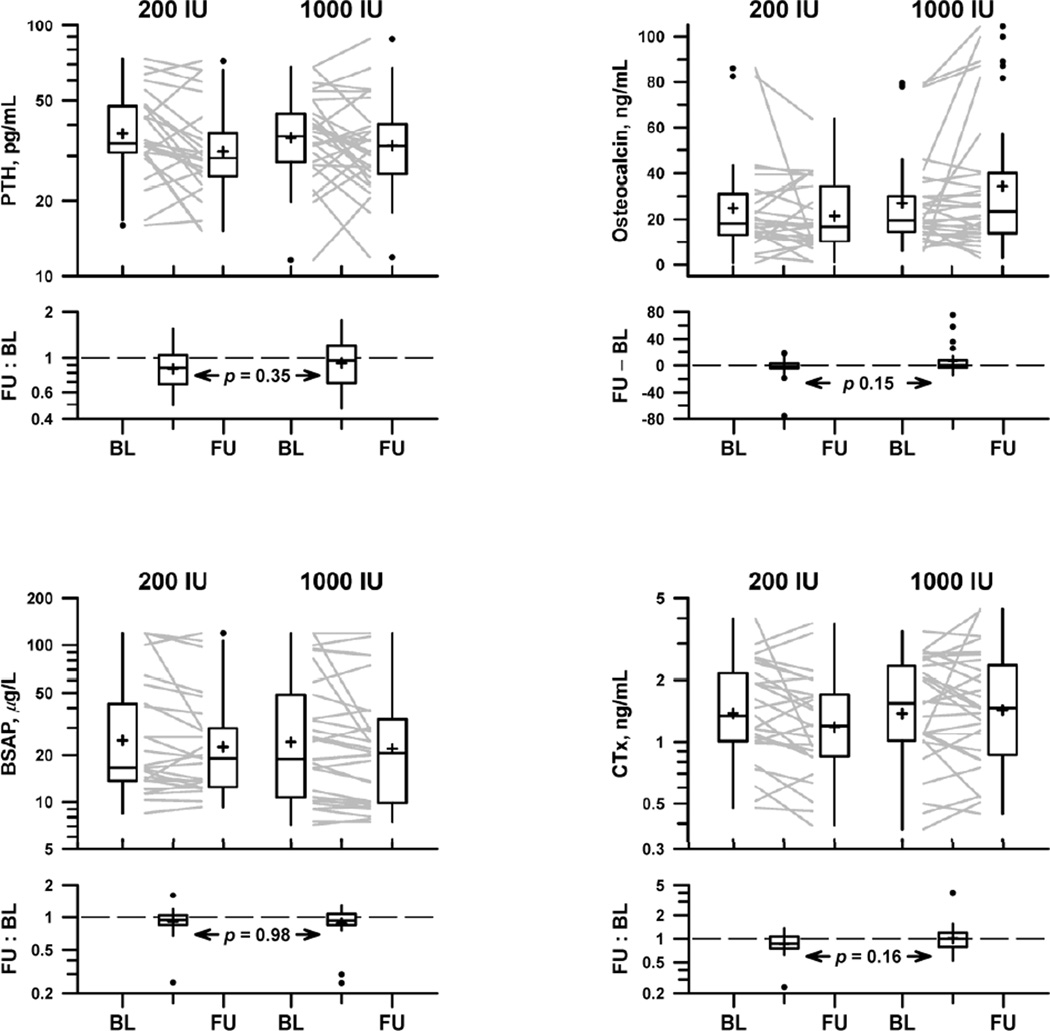
PTH levels were similar between groups at baseline and at follow-up (Figure 2). The mean change in PTH level from baseline to 3 months was not significantly different between treatment arms (p=0.36). (Table 2). No subjects had evidence of PTH suppression below 12 pg/mL over the course of the study. No significant correlation was found between PTH level and 25(OH)D level within each treatment group or with both groups combined. The change in bone turnover markers was similar between groups. (Figure 2, Table 2).
Figure 2.
Markers of bone metabolism in the 200 IU treatment arm and 1000 IU treatment arm: parathyroid hormone (upper left), osteocalcin (upper right), bone-specific alkaline phosphatase (lower left), C-telopeptides (lower right). Each subject’s marker levels are represented by a grey line connecting baseline (BL) with follow-up (FU). Box plots illustrate the distribution of baseline and follow-up levels (upper panel) and within-subject changes from baseline to follow-up (lower panel). Top and bottom of the box indicate quartile boundaries (25th and 75th percentiles); center belt indicates median; cross (+) indicates mean. Individual points (●) indicate outliers, falling outside the box by at least 1.5 times its height. Vertical lines extend to position of farthest non-outlier above and below the box. P-value in lower panel tests the hypothesis that the distribution of changes is equal in the two treatment arms.
Mean change in fasting glucose and fasting insulin levels did not vary significantly between treatment groups over the study period (Table 2). These levels did not correlate with 25(OH)D level in either group alone or in both groups combined. Calcium, magnesium, and phosphate levels remained stable in both treatment groups over the course of the study.
DISCUSSION
The goal of this double-blind randomized clinical trial was to evaluate the effects of short-term vitamin D3 supplementation dose of 200 vs. 1000 IU in healthy adolescents with baseline vitamin D sufficiency over the fall through spring months in New England. A supplementation dose of 200 IU daily corresponded to the IOM and AAP recommendations for vitamin D supplementation in this age group at the time of trial initiation,15,29 and many experts have recommended 1000IU daily as the optimal dose for bone health in children and adults.18–20 The study design is unique in that only subjects with serum 25(OH)D levels above 20 ng/mL were included and enrollment was limited to the fall and winter months, in order to minimize confounding by underlying vitamin D deficiency and sunlight exposure. This study showed that both of these vitamin D regimens resulted in no change in 25(OH)D levels over the course of 11 weeks, with no significant difference in 25(OH)D levels between treatment arms over time. Higher supplementation dose did not increase serum 25(OH)D to a greater degree than the lower dose; however, the lack of change in serum 25(OH)D during a time when levels tend to decline due to limited sun exposure is noteworthy. Signs of vitamin D intoxication or PTH suppression did not occur with either dose.
Professional medical societies have disagreed as to the preferred vitamin D supplementation regimen for healthy adolescents. The American Academy of Pediatrics recommends a vitamin D supplementation dose of 400 IU daily in healthy adolescents based on 2008 published guidelines.17 In November 2010, the Institute of Medicine published new recommendations for calcium and vitamin D supplementation in the healthy population. In the adolescent age group, the daily recommended dose of vitamin D was increased from 200 to 600 IU, and the safe upper limit was increased to 4000 IU daily.16 In contrast, the Endocrine Society published a Clinical Practice Guideline recommending daily vitamin D supplementation with 600–1000 IU in this age group.30 Of note, the Endocrine Society Guideline was aimed at individuals at risk for vitamin D deficiency or low bone density, while the IOM recommendations were directed toward the healthy US/Canadian general population. Both the IOM and the Endocrine Society acknowledged that studies in children and adolescents were limited and called for additional clinical trials evaluating vitamin D supplementation in this age group.
Studies have yielded conflicting data with regard to the optimal dose of vitamin D supplementation for healthy adolescents and the effects of vitamin D supplementation on bone turnover markers and PTH levels in this age group. The differing results may be related to multiple potential confounding factors, such as sunlight exposure leading to cutaneous vitamin D synthesis, difficulty ensuring compliance in adolescent subjects, and differences in dietary vitamin D intake. In adults, baseline vitamin D deficiency has been shown to alter response to supplementation,31 and the same may be true in adolescents. In addition, a wide variety of supplemental vitamin D regimens have been utilized by clinicians, ranging from daily to weekly, monthly, or annual doses of vitamin D.
Previous studies in adolescents have tested the effects of higher vitamin D supplementation doses and included teenagers with vitamin D deficiency. In a recent study by Dong et al., 49 African American adolescents ages 14–18 years old were randomized to vitamin D 400 IU daily or 2000 IU daily for 16 weeks. 32 Serum 25(OH)D levels increased by a mean of 21 ng/mL (from 13.3 ng/mL to 34.3 ng/mL) in the higher dose group compared to an increase of 10.3 ng/mL (from 13.6 to 20.5 ng/mL) in the lower dose group. This difference in change in 25(OH)D was statistically significant between treatment groups. After supplementation with 2000 IU daily, 4.4% of these subjects remained vitamin D deficient (25(OH)D<20), compared to 61% who remained deficient in the 400 IU daily group. Two different studies compared weekly doses of 1400 IU (equivalent to 200 IU daily), 14,000 IU (equivalent to 2000 IU daily), or placebo over the course of a year in healthy children and adolescents.14,33 Both of these studies showed a significant difference in mean change in serum 25(OH)D levels between treatment groups, with an increase in serum 25(OH)D over 12 months of 3–4 ng/mL with low dose supplementation (similar to placebo) and 21–24 ng/mL with the higher dose.
In contrast to these studies, our study showed no significant difference in change in serum 25(OH)D between a vitamin D dose of 1000 IU daily compared to 200 IU daily over 11 weeks in winter. Stable serum 25(OH)D levels were achieved using both regimens. One key difference between these trials is that adolescents in our study began with baseline vitamin D sufficiency with 25(OH)D levels greater than 20 ng/mL. The response to supplementation may be different in adolescents who already have sufficient serum concentrations of vitamin D, such that higher doses would be required to elicit a greater rise in 25(OH)D levels beyond 20 ng/mL. Our study adds important information to that contributed by the above trials in that 1000 IU daily may not be sufficient to increase serum 25(OH)D beyond that achieved with a lower supplemental dose in subjects with baseline vitamin D sufficiency or that a longer treatment course than 11 weeks is required.
In addition, in our group of vitamin D sufficient subjects, the effects of vitamin D supplementation on PTH did not vary by supplementation dose, similar to findings in other vitamin D supplementation trials of adolescents. 32,34,35 No significant correlation between PTH and 25(OH)D levels were noted. In addition, change in markers of bone formation and bone resorption did not differ between treatment groups. Previous studies evaluating the effect of vitamin D supplementation on markers of bone turnover in children and adolescents have been varied, reporting a decline in bone resorption markers,35 an increase in bone formation markers,36 or no change at all.34
Studies in adults and children have postulated an effect of vitamin D on metabolic parameters including insulin resistance and diabetes.37–39 Obese adolescents have a high prevalence of vitamin D deficiency and may require higher doses of vitamin D supplementation in order to achieve adequate 25(OH)D levels.40 In our study of vitamin D sufficient non-obese adolescents, a higher dose of supplemental vitamin D did not elicit a significant difference in fasting insulin and glucose levels between supplementation groups.
Strengths of this study include the community-based, racially and ethnically diverse subject sample, making the results directly applicable to the general population. In addition, potential sources of bias were carefully minimized. Contribution of dietary intake of vitamin D was evaluated by a bionutritionist with 24 hour recall as well as 3- day food diaries. Sunlight exposure was accounted for and minimized in the design of the study. Groups were well matched in terms of known influences on vitamin D status, including race and BMI. Compliance was carefully assessed using the state-of-the-art MEMS Trackcaps system. Lastly, examining the effects of vitamin D supplementation in a group of vitamin D replete adolescents represents a novel study question and design.
Weaknesses of the study include the small sample size. The large variance in the mean change of both treatment groups reflects the significant variability in response among subjects, suggesting that a larger sample may have detected more subtle changes in serum 25(OH)D. In addition, a subset of subjects with initial vitamin D deficiency were treated with high dose ergocalciferol prior to study enrollment to attain vitamin D sufficiency without a washout period. Although we attempted to account for this in our multivariate adjustment and by repeating the analysis after excluding these subjects, these subjects may have affected the results, causing a transiently elevated 25OHD level that gradually fell over the course of the study.
In conclusion, we found that two different regimens of vitamin D supplementation, 200 IU vs. 1000 IU, resulted in no change in serum 25(OH)D levels over 11 weeks in a racially and ethnically diverse group of healthy adolescent boys and girls with baseline vitamin D sufficiency. No subjects exhibited adverse effects of supplementation at either dose, and 96% of subjects remained vitamin D sufficient over the fall through spring months in New England. Additional studies are required to determine longterm effects of vitamin D supplementation on bone turnover markers and bone health in adolescents.
IMPLICATIONS AND CONTRIBUTION SUMMARY STATEMENT.
Two different regimens of vitamin D supplementation resulted in no change in 25(OH)D levels over 11 weeks during the fall through spring months in a diverse group of healthy adolescents with baseline vitamin D sufficiency.
Acknowledgments
This study was supported by Boston Children’s Hospital Young Investigator Award; the Mary A. and John M. McCarthy Foundation; the Clinical and Translational Research Executive Committee Matching Funds Program; and the Harvard Catalyst, The Harvard Clinical and Translational Science Center (National Center for Research Resources and the National Center for Advancing Translational Sciences, National Institutes of Health Award #UL1 RR 05758 and financial contributions from Harvard University and its affiliated academic health centers). This work was also supported in part by the Leadership Education in Adolescent Health Training grant #T71MC00009 from the Maternal and Child Health Bureau, Health Resources and Services Administration, as well as T32 DK007699-29 NRSA Institutional Training Grant. The content is solely the responsibility of the authors and does not necessarily represent the official views of Harvard Catalyst, Harvard University and its affiliated academic health care centers, or the National Institutes of Health. Vitamin D3 was donated by Tishcon.
Abbreviations
- 25[OH]D
25-hydroxyvitamin D
- IU
international units
- PTH
parathyroid hormone
- OC
osteocalcin
- CTX
c-telopeptide
- BSAP
bone specific alkaline phosphatase
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosures: The authors have no conflicts of interest to disclose.
REFERENCES
- 1.Gordon CM, DePeter K, Feldman HA, et al. Prevalence of Vitamin D Deficiency among Healthy Adolescents. Arch Ped Adol Med. 2004;158:531–537. doi: 10.1001/archpedi.158.6.531. [DOI] [PubMed] [Google Scholar]
- 2.Looker AC, Dawson-Hughes B, Calvo MS, et al. Serum 25-hydroxyvitamin D Status of Adolescents and Adults in Two Seasonal Subpopulations from NHANES III. Bone. 2002;30:771–777. doi: 10.1016/s8756-3282(02)00692-0. [DOI] [PubMed] [Google Scholar]
- 3.Harkness LS, Cromer BA. Vitamin D Deficiency in Adolescent Females. J Adolesc Health. 2005;37:75. doi: 10.1016/j.jadohealth.2004.07.015. [DOI] [PubMed] [Google Scholar]
- 4.Aloia JF, Patel M, DiMaano R, et al. Vitamin D Intake to Attain a Desired Serum 25-Hydroxyvitamin D Concentration. Am J Clin Nutr. 2008;87:1952–1958. doi: 10.1093/ajcn/87.6.1952. [DOI] [PubMed] [Google Scholar]
- 5.Weng FL, Shults J, Leonard MB, et al. Risk Factors for Low Serum 25-hydroxyvitamin D Concentrations in Otherwise Healthy Children and Adolescents. Am J Clin Nutr. 2007;86:150–158. doi: 10.1093/ajcn/86.1.150. [DOI] [PubMed] [Google Scholar]
- 6.Rovner AJ, O'Brien KO. Hypovitaminosis D among Healthy Children in the United States: A Review of the Current Evidence. Arch Pediatr Adolesc Med. 2008;162:513–519. doi: 10.1001/archpedi.162.6.513. [DOI] [PubMed] [Google Scholar]
- 7.Rutstein R, Downes A, Zemel B, et al. Vitamin D Status in Children and Young Adults with Perinatally Acquired HIV Infection. Clin Nutr. 2011;30:624–628. doi: 10.1016/j.clnu.2011.02.005. [DOI] [PubMed] [Google Scholar]
- 8.Hickey LB, Gordon CM. Vitamin D Deficiency: New Perspectives on an Old Disease. Curr Opin Endocrinol Diabetes. 2004;11:18–25. [Google Scholar]
- 9.Zamora SA, Rizzoli R, Belli DC, et al. Vitamin D Supplementation during Infancy is associated with Higher Bone Mineral Mass in Prepubertal Girls. J Clin Endocrinol Metab. 1999;84:4541–4544. doi: 10.1210/jcem.84.12.6183. [DOI] [PubMed] [Google Scholar]
- 10.Gordon CM, Bachrach LK, Carpenter TO, et al. Bone Health in Children and Adolescents: a Symposium at the Annual Meeting of the Pediatric Academic Societies/Lawson Wilkins Pediatric Endocrine Society, May 2003. Curr Prob Ped Adol Health Care. 2004;34:221–248. doi: 10.1016/j.cppeds.2004.03.001. [DOI] [PubMed] [Google Scholar]
- 11.Bischoff-Ferrari H, Willett WC, Wong JB, et al. Fracture Prevention with Vitamin D Supplementation: a Meta-analysis of Randomized Controlled Trials. JAMA. 2005;293:2257–2264. doi: 10.1001/jama.293.18.2257. [DOI] [PubMed] [Google Scholar]
- 12.Cheng S, Tylavsky F, Kroger H, et al. Association of Low 25-hydroxyvitamin D Concentrations with Elevated Parathyroid Hormone Concentrations and Low Cortical Bone Density in Early Pubertal and Prepubertal Finnish Girls. Am J Clin Nutr. 2003;78:485–492. doi: 10.1093/ajcn/78.3.485. [DOI] [PubMed] [Google Scholar]
- 13.Cashman KD, Hill TR, Cotter AA, et al. Low Vitamin D Status Adversely Affects Bone Health Parameters in Adolescents. Am J Clin Nutr. 2008;87:1039–1044. doi: 10.1093/ajcn/87.4.1039. [DOI] [PubMed] [Google Scholar]
- 14.El-Hajj Fuleihan G, Nabulsi M, Tamim H, et al. Effect of Vitamin D Replacement on Musculoskeletal Parameters in School Children: a Randomized Controlled Trial. J Clin Endocrinol Metab. 2006;91:405–412. doi: 10.1210/jc.2005-1436. [DOI] [PubMed] [Google Scholar]
- 15.Institute of Medicine. Dietary Reference Intakes for Calcium, Phosphorus, Magnesium, Vitamin D, and Fluoride. Washington, DC: The National Academic Press; 1997. [PubMed] [Google Scholar]
- 16.Institute of Medicine. Dietary Reference Intakes for Calcium and Vitamin, D. Washington DC: The National Academic Press; 2011. [Google Scholar]
- 17.Wagner CL, Greer FR. Prevention of Rickets and Vitamin D Deficiency in Infants, Children, and Adolescents. Pediatrics. 2008;122:1142–1152. doi: 10.1542/peds.2008-1862. [DOI] [PubMed] [Google Scholar]
- 18.Vieth R. What is the Optimal Vitamin D Status for Health? Prog Biophys Mol Biol. 2006;92:26–32. doi: 10.1016/j.pbiomolbio.2006.02.003. [DOI] [PubMed] [Google Scholar]
- 19.Heaney RP. Vitamin D: Criteria for Safety and Efficacy. Nutr Rev. 2008;66(Suppl 2):S178–S181. doi: 10.1111/j.1753-4887.2008.00102.x. [DOI] [PubMed] [Google Scholar]
- 20.Holick MF. Vitamin D Deficiency. N Engl J Med. 2007;357:266–281. doi: 10.1056/NEJMra070553. [DOI] [PubMed] [Google Scholar]
- 21.Heaney RP, Davies KM, Chen TC, et al. Human Serum 25-Hydroxycholecalciferol Response to Extended Oral Dosing with Cholecalciferol. Am J Clin Nutr. 2003;77:204–210. doi: 10.1093/ajcn/77.1.204. [DOI] [PubMed] [Google Scholar]
- 22.Biancuzzo RM, Young A, Bibuld D, et al. Fortification of Orange Juice with Vitamin D2 or Vitamin D3 is as Effective as an Oral Supplement in Maintaining Vitamin D Status in Adults. Am J Clin Nutr. 2010;91:1621–1626. doi: 10.3945/ajcn.2009.27972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Misra M, Pacaud D, Petryk A, et al. Vitamin D Deficiency in Children and Its Management: Review of Current Knowledge and Recommendations. Pediatrics. 2008;122:398–417. doi: 10.1542/peds.2007-1894. [DOI] [PubMed] [Google Scholar]
- 24.Kulasingam V, Jung BP, Blasutig IM, et al. Pediatric Reference Intervals for 28 Chemistries and Immunoassays on the Roche Cobas 6000 Analyzer - A CALIPER Pilot Study. Clin Biochem. 2010;43:1045–1050. doi: 10.1016/j.clinbiochem.2010.05.008. [DOI] [PubMed] [Google Scholar]
- 25.Pathak MA, Jimbow K, Szabo G, et al. Sunlight and Melanin Pigmentation. In: Goldsmith K, editor. Photochemical and photobiological reviews. New York: Plenum Press; 1976. [Google Scholar]
- 26.Jimbow K, Fitzpatrick B, Wick MM. Biochemistry and Physiology of Melanin Pigmentation. In: Goldsmith LA, editor. Physiology, Biochemistry, and Molecular Biology of the Skin. New York: Oxford University Press; 1991. [Google Scholar]
- 27.Averbuch M, Weintraub M, Pollack DJ. Compliance Assessment in Clinical Trials: the MEMS Device. J Clin Res Pharmacoepidemiol. 1990;4:199–204. [Google Scholar]
- 28.Olivieri NF, Matsui D, Hermann C, et al. Compliance Assessed by the Medication Event Monitoring System. Arch Dis Child. 1991;66:1399–1402. doi: 10.1136/adc.66.12.1399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gartner LM, Greer FR, et al. Prevention of Rickets and Vitamin D Deficiency: New Guidelines for Vitamin D Intake. Pediatrics. 2003;111:908–910. doi: 10.1542/peds.111.4.908. [DOI] [PubMed] [Google Scholar]
- 30.Holick MF, Binkley NC, Bischoff-Ferrari HA, et al. Evaluation, Treatment, and Prevention of Vitamin D Deficiency: An Endocrine Society Clinical Practice Guideline. J Clin Endocrinol Metab. 2011;96:1911–1930. doi: 10.1210/jc.2011-0385. [DOI] [PubMed] [Google Scholar]
- 31.Holick MF and Chen TC. Vitamin D Deficiency: A Worldwide Problem with Health Consequences. Am J Clin Nutr. 2008;87(suppl):1080S–1086S. doi: 10.1093/ajcn/87.4.1080S. [DOI] [PubMed] [Google Scholar]
- 32.Dong Y, Stallman-Jorgensen IS, Pollock NK, et al. A 16-week Randomized Clinical Trial of 2000 International Units Daily Vitamin D3 Supplementation in Black Youth: 25-Hydroxyvitamin D, Adiposity, and Arterial stiffness. J Clin Endocrinol Metab. 2010;95:4584–4591. doi: 10.1210/jc.2010-0606. [DOI] [PubMed] [Google Scholar]
- 33.Maalouf J, Nabulsi M, Vieth R, et al. Short- and Long-term Safety of Weekly High Dose Vitamin D3 Supplementation in School Children. J Clin Endocrinol Metab. 2008;93:2693–2701. doi: 10.1210/jc.2007-2530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Molgaard C, Larnkjaer A, Cashman KD, et al. Does Vitamin D Supplementation of Healthy Danish Caucasian Girls Affect Bone Turnover and Bone Mineralization? Bone. 2010;46:432–439. doi: 10.1016/j.bone.2009.08.056. [DOI] [PubMed] [Google Scholar]
- 35.Viljakainen HT, Natri AM, Kärkkäinen M, et al. A Positive Dose–Response Effect of Vitamin D Supplementation on Site-Specific Bone Mineral Augmentation in Adolescent Girls: A Double-Blinded Randomized Placebo-Controlled 1-Year Intervention. J Bone Miner Res. 2006;21:836–844. doi: 10.1359/jbmr.060302. [DOI] [PubMed] [Google Scholar]
- 36.Ghazi AA, Hosseinpanah F, M Ardakani E, et al. Effects of Different Doses of Oral Cholecalciferol on Serum 25(OH)D, PTH, Calcium and Bone Markers during Fall and Winter in Schoolchildren. Eur J Clin Nutr. 2010;64:1415–1422. doi: 10.1038/ejcn.2010.169. [DOI] [PubMed] [Google Scholar]
- 37.Forouhi NG, Luan J, Cooper A, et al. Baseline Serum 25-hydroxyvitamin D is Predictive of Future Glycemic Status and Insulin Resistance: the Medical Research Council Ely Prospective Study 1990–2000. Diabetes. 2008;57:2619–2625. doi: 10.2337/db08-0593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Olson ML, Maalouf NM, Oden JD, et al. Vitamin D Deficiency in Obese Children and its Relationship to Glucose Homeostasis. J Clin Endocrinol Metab. 2012;97:279–285. doi: 10.1210/jc.2011-1507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Chiu KC, Chu A, Go VLW, et al. Hypovitaminosis D is associated with Insulin Resistance and β Cell Dysfunction. Am J Clin Nutr. 2004;79:820–825. doi: 10.1093/ajcn/79.5.820. [DOI] [PubMed] [Google Scholar]
- 40.Harel Z, Flanagan P, Forcier M, et al. Low Vitamin D Status among Obese Adolescents: Prevalence and Response to Treatment. J Adol Health. 2011;48:448–452. doi: 10.1016/j.jadohealth.2011.01.011. [DOI] [PubMed] [Google Scholar]