Abstract
Objective
Homebound older adults may be vulnerable to the deleterious impact of untreated depression. Yet because these elders are difficult to reach, there is little data on the rates of depressive symptoms and suicidal ideation among this group. The objective of this study is to document the rates of depression and correlates among a population of homebound elders.
Methods
Using a community based participatory research partnership, we implemented a routine screening for depressive symptoms and suicidal ideation among older recipients of Westchester County’s home meal program. Older adults enrolled in the home delivered meal program were administered the Physician Health Questionnaire–9 item (PHQ-9), and questions to assess pain, recent falls, alcohol abuse and perceived emotional distress.
Results
In our sample of 403 meal recipients, 12.2% of older adults reported clinically significant depression (PHQ-9>9) and 13.4% reported passive or active suicidal thoughts. One third of recipients with significant depressive symptoms were currently taking an antidepressant. Almost a third of older adults who endorsed suicide ideation did not report clinically significant depressive symptoms. Among men, suicidal thoughts were associated with chronic pain and greater depression severity, whereas pain was not a predictor of suicidal thoughts among women.
Conclusion
More than 1 in 9 elders suffer from depression; most are untreated with one third on antidepressants but still symptomatic. Through partnerships between public agencies that provide age related services and academic investigators there is an opportunity for improved detection of unmet mental health needs. Future research should explore innovative models to improve access to mental health services once unmet need is detected.
Keywords: Geriatric depression, suicide ideation, homebound, home delivered meals
Depressive symptoms are common and depression is expected to be the second to heart disease [1]}). Among the elderly, depressive symptoms usually occur in the context of multiple medical illnesses and disabilities [2]. In primary care settings 6–8% of patients have major depression [3, 4]. One quarter of patients in rehabilitation centers for respiratory diseases have major depression [5, 6]. Using a SCID diagnostic interview, over 14% of older medical patients have major depression and another 20% have less severe forms of depression [7]. These rates are consistent with data from other studies documenting a quarter to a third of elders receiving home services suffer from depression [8] [9] [10]). Depression among community elders has an unremitting course and is associated with greater disability, inappropriate service use and mortality ([9, 11].
Despite improvements in routine screening and detection of depression in mental health and primary care settings, significant sub-pockets of high-risk older adults are not reached (Bruce et al., 2005, Choi et al., 2007). These elders tend to be ‘hidden’ from view of traditional care providers and face transportation, stigma and financial barriers to care (Bruce et al., 2005, Druss, 2006). As a consequence, their depressive symptoms often go untreated. For those reasons, alternative strategies are needed to integrate screening into other routine services provided to homebound elders to ensure access to quality mental health care for those in need.
To improve the detection of depression among homebound elders we developed a community-based research partnership using the Evidence-Based Community/Partnership Model proposed by Wells, Alegria, Bruce, et al (Wells et al., 2004). This model relies on a partnership between communities and researchers, blending techniques of community participatory research and evidence-based quality improvement programs. Its goal is to identify problems with both agency and public health significance, and to address them by tailoring evidence-based strategies to fit the constraints, needs, and life circumstances of the targeted community setting and developing alternative approaches that are sustainable.
The partnership developed an easily integrated depression screening protocol to evaluate seniors who receive home delivered meals. The sociodemographic and clinical characteristics of this population put them at high risk for depression while their homebound status limits access to routine depression screening and treatment. The Administration on Aging’s (AOA’s) Elderly Nutrition Program (ENP) serves about 3.1 million community dwelling older adults (age ≥ 60) annually. Compared to the elderly US population, older adults receiving meals tend to be older, poorer, minority and live alone; they have greater difficulty caring for themselves and have increased health and nutrition risks (Sharkey, 2005, Ponza et al., 1996, [12]).
In this paper we describe the rates of clinically significant depressive symptoms and endorsement of passive and active suicidal ideation among seniors receiving home delivered meals. We hypothesized that the rates of depressive symptoms among this group of homebound elders would be comparable to the rates documented in other populations of elders with complex medical illnesses and disabilities, such as homecare and assisted living [7, 13], Gruber-Baldini et al., 2004). Additionally we hypothesized that the rates of depressive symptoms and suicidal thoughts would be comparable across racial groups and gender, and associated with chronic pain.
Methods
The study was supported by an NIH grant-funded collaboration between the Westchester County Department of Senior Programs & Services (DSPS), an AoA agency, and the Weill Cornell Institute for Geriatric Psychiatry (P30 MH68638). The partnership developed procedures that were consistent with DSPS’s system and utilized standardized methods brought by the academic research group.
Sample
A senior is eligible for the home meal program if that individual has a condition, due to illness or injury, that restricts the individual’s ability to leave the home except with the assistance of another individual or the aid of a supportive device (such as a cane or a wheelchair), or if the individual has a condition such that leaving his or her home is contraindicated. Elders receiving home meals who were eligible for a certification interview from December 2004–June 2006 were eligible for the screening protocol. We contacted 523 elders consecutively for this wave of our project.
Measures
Standardized questions to assess depressive symptoms, cognitive status, alcohol abuse and the presence of chronic pain were added to the meal certification interview. The Physician Health Questionnaire (PHQ-9) was added to assess depressive symptoms. The PHQ-9 assesses the symptoms used to assess DSM-IV criteria for Major Depressive Disorder (Kroenke et al., 2002). The frequency of each symptom is rated on a 4-point scale (“from not at all” to “nearly every day”). The scale is easy to administer and has been used reliably by non-psychiatric interviewers in primary care (Lowe et al., 2004, Oxman et al., 2002, Ell et al., 2005), home healthcare settings (Ell, et al., 2005) and in community samples (Martin et al., 2006). Suicidal thoughts are assessed with a single item on the PHQ-9 (e.g., “How often have you been bothered by thoughts that you would be better off dead or of hurting yourself in some way”). The PHQ-9 is widely used because it offers a measure of symptom severity, rates the pervasiveness of each symptom used as criteria to establish DSM IV Major Depressive Disorder, and has established treatment planning guidelines. Clinically significant, moderate depressive symptoms (PHQ-9>9) warrant the development of a treatment plan (Kroenke, et al., 2002)[14].
In addition to the PHQ-9, interviewees were asked whether they were experiencing depression or emotional distress. This measure of perceived distress complements the formal assessment of depressive symptoms. Current antidepressant treatment was determined as part of the standard review of current medications.
Cognitive functioning was assessed using the Blessed Orientation, Memory and Concentration (BOMC) scale (Katzman et al., 1983) where cognitive impairment was defined as a score greater than 15 (Bartels et al., 2004, Levkoff et al., 2004). Chronic pain was assessed using self-report questions to evaluate the presence of painful sensations for the preceding three months (Elliot et al., 1999). Finally, the assessors administered the 4-item CAGE to assess for alcohol problems (Ewing, 1984) and recorded whether the interviewee had sustained a fall in the last 6 months.
Training & supervision
Training and supervision on the protocol measures was provided by the academic collaborators. Monthly supervision was provided to review administration and scoring. Older adults with clinically significant symptoms (PHQ-9>9) were offered a referral for mental health services. Elders who endorsed suicidal thoughts were administered our standardized risk protocol (Raue et al., 2006).
Data Analysis
Interviews were conducted from December 2004–June 2006 with all consecutive and willing elders eligible for a meal certification interview. Chi-square analyses and ANOVA comparisons were conducted to examine the relation of depressive symptoms (e.g., none, mild and moderate to severe) with sociodemographic factors, clinical characteristics (e.g. pain, alcohol use), and a recent fall.
To identify a model of factors associated with suicidal thoughts, we conducted a forward logistic regression analysis with the endorsement of suicidal thoughts as the dependent variable. Analyses controlled for other depressive symptoms (the sum of the remaining PHQ-9 items). Interaction terms were created to capture potential differences between men and women in the relation of pain to suicidal thoughts. This approach was taken based on the literature supporting gender differences in both the experience and impact of chronic pain across the lifespan (Unruh, 1996).
Results
Data were available on 403 older adults receiving home meals. The analytic sample represents 77% of total eligible meal recipients during the study period (N=523). Seniors were excluded due to inability to understand the purpose of the interview due to severe cognitive impairment (6%), being too medically ill (9%), or having a language barrier (1%). A small number of older adults (7%) refused to be interviewed. There was no difference in the gender, race or age of seniors who were and were not interviewed. The demographics for the sample are presented in Table 1.
Table 1.
Demographic, Clinical and Service Needs for Sample (N=403)
| N | % | Mean (SD) Range | |
|---|---|---|---|
| Demographics | |||
| Female | 290 | 72% | |
| Race | |||
| Black | 84 | 20% | |
| White | 322 | 80% | |
| Asian | 0 | 0% | |
| Age | 403 | 83.3 (9.1) 60–101 | |
| Years of schooling | 403 | 13.0 (3.2) 6–22 | |
| Of Hispanic origin | 7 | 1.7% | |
| Clinical characteristics | |||
| Cognitively impaired (BOMC ≥16) | 41 | 10.2% | |
| Depression status | |||
| PHQ-9 score ≥10 | 49 | 12.2% | |
| Depression severity (PHQ-9 range) | |||
| No depression (0–4) | 287 | 71.2% | |
| Mild depression(5–9) | 67 | 16.6% | |
| Moderate (10–14) | 31 | 7.7% | |
| Moderately Severe (15–19) | 12 | 3.0% | |
| Severe (20–27) | 6 | 1.5% | |
| Suicidal ideation (active or passive) | 54 | 13.4% | |
| Pain | |||
| Experiences chronic pain | 188 | 46.5% | |
| Duration of pain (in months) | 26.5 (74.4) 0–672 | ||
| Additional service needs | |||
| Referred for nutritional services | 27 | 6.7% | |
| Referred for case management services | 73 | 18% | |
Almost half (47%) of the elders endorsed chronic pain with an average duration of 5 years. In the sample, almost one quarter (24%) sustained a fall within the last six months. Only one in five seniors (20%) reported having had an alcoholic drink in the last month.
Depressive symptoms were common; more than a third (36%) of the sample reported being “bothered by feeling down, depressed or hopeless” in the prior two weeks; 12% reported moderate to severe depression symptoms (Kroenke et al., 2002). An additional 17% had mild symptoms (PHQ-9 scores 5–9). In sum, 29% of this sample of homebound seniors reported at least mild symptoms of depression.
Correlates of depression
There were no differences in the prevalence of clinically significant depressive symptoms associated with race, gender, age or years of education. There was a significant relationship between chronic pain and depression severity levels (χ2 = 16.25, df=2, p<.001) among the entire sample. The prevalence of chronic pain was higher (69% versus 40%) among seniors reporting moderate to severe depression as compared to those elders without any depressive symptoms.
Almost 1 in five (19%) elders in this sample were taking an antidepressant. Among the elders with moderate to severe symptoms, one third (33%) were taking an antidepressant and still reported significant depression. The remaining elders on antidepressants had mild to no symptoms. Among the depressed seniors with significant symptoms, only half (51%) viewed themselves as suffering from emotional difficulties or depression. There was no relation between depressive symptoms and cognitive status alcohol use, or a recent fall.
Suicidal ideation
Suicidal thoughts (thoughts of being “better off dead, or of hurting yourself in some way” on several days in the prior two weeks) were reported by 13% of respondents. The proportion of respondents reporting suicidal thoughts increased significantly with the severity of depression. A small fraction (4%) of older adults with no symptoms or nominal depressive symptoms (PHQ-9 scores 0–4) reported suicidal ideation. By contrast, one quarter (25%) of adults with mild symptoms, one third (32%) with moderate symptoms, and 83% of older adults with moderately severe to severe depression (PHQ-9 scores 15–27) had suicidal ideation (χ2 = 86.71, df=3, p=<. 001; see Figure 1).
Figure 1.
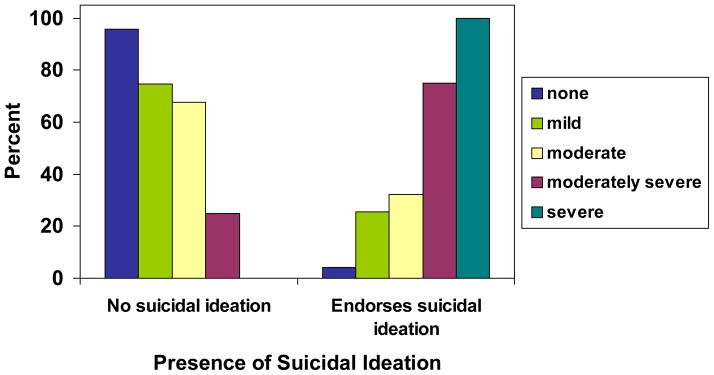
Endorsement of suicidal ideation by depression severity
There were no differences in rates of suicide associated with age, race, marital status or gender. In analyses comparing the relation of suicidal thoughts and pain for each gender, pain was not associated with suicide ideation among women. In contrast, pain was strongly associated with suicide ideation in men (χ2 =3.95, df=1, p<.05), such that men with chronic pain reported the highest levels of suicidal ideation (17.8%) whereas men without chronic pain had the lowest rate (5.9%). In a logistic regression analysis of the entire sample, an interaction term was created to examine the relation of gender and duration of pain with the presence of suicidal thoughts. The interaction of pain and gender was significant in predicting the presence of suicidal ideation controlling for depression severity. This model accounted for 38% of the variance in reported suicidal ideation (Table 2).
Table 2.
Depression severity, duration of pain, gender and interaction of gender by pain duration as predictors of the presence of suicidal ideation
| Variables in the Equation
| |||||||
|---|---|---|---|---|---|---|---|
| B | S.E. | Wald | df | Sig. | Exp(B) | ||
|
| |||||||
| Step 1(a) | PHQ9 total | .282 | .036 | 62.153 | 1 | .000 | 1.326 |
| Gender (1) | −.535 | .452 | 1.399 | 1 | .237 | .586 | |
| Pain duration (in months) | .015 | .006 | 5.406 | 1 | .020 | 1.015 | |
| Pain duration X gender | −.010 | .005 | 5.121 | 1 | .024 | .990 | |
| Constant | −3.268 | .313 | 109.295 | 1 | .000 | .038 | |
Nagelkerke R Square = .385
Discussion
Among seniors who receive home meals clinically significant depressive symptoms and suicidal thoughts are reported at high rates. Most of those elders with significant symptoms report no treatment. One third of the depressed sample was currently on a medication for depression but endorsed significant symptoms on the PHQ-9.
The rates of depressive symptoms in this sample are consistent with findings by other studies assessing depression in frail, medically compromised older adults (Bruce et al., 2002, Gruber-Baldini et al., 2004, Anstey et al., 2007). Interestingly, over half of these seniors with depression do not view their symptoms as psychological or psychiatric. Beyond detection, interventions that dispel ageist myths and disentangle medical symptoms from depression may improve access to mental health services. Asking about chronic pain may help identify older men who are known to have the highest rates of completed suicide. This association of pain and suicidal thoughts may reflect the relation of medical illness and suicide [15] or the impact of untreated pain [16].
This study demonstrated the feasibility of integrating mental health screening into routine services provided to community dwelling homebound elders. The collaborative program paved the way for depression screening of all elders participating in home delivered meals program in Westchester County. Given the high levels of depression detected, meal programs and other in home services may partner with mental health programs to improve access to treatment for homebound seniors. We recognize that a limitation of this study is that it is a single point of assessment that does not provide information about the history of depression, adequacy of prior treatments and the course of symptoms.
Building partnerships between aging service providers and mental health programs offer innovative opportunities to improve detection of mental health problems that would jeopardize independence [17]. In home service providers can be the first step in facilitating access to treatment for older adults who would not be seen in outpatient mental health settings.
Acknowledgments
This study was supported by the National Institute of Mental Health grants P30 MH68638 (PI: GS Alexopoulos) and K23 MH6681 (J Sirey).
References
- 1.Chapman DP, Perry GS. Depression as a major component of public health for older adults. Prev Chronic Dis. 2008;5(1):A22. [PMC free article] [PubMed] [Google Scholar]
- 2.Alexopoulos GS. Depression in the elderly. Lancet. 2005;365(9475):1961–70. doi: 10.1016/S0140-6736(05)66665-2. [DOI] [PubMed] [Google Scholar]
- 3.Schulberg HC, et al. Characteristics and course of major depression in older primary care patients. Int J Psychiatry Med. 1998;28(4):421–36. doi: 10.2190/G23R-NGGN-K1P1-MQ8N. [DOI] [PubMed] [Google Scholar]
- 4.Unutzer J, et al. Care for depression in HMO patients aged 65 and older. J Am Geriatr Soc. 2000;48(8):871–8. doi: 10.1111/j.1532-5415.2000.tb06882.x. [DOI] [PubMed] [Google Scholar]
- 5.Borson S, Claypoole K, McDonald GJ. Depression and Chronic Obstructive Pulmonary Disease: Treatment Trials. Semin Clin Neuropsychiatry. 1998;3(2):115–130. [PubMed] [Google Scholar]
- 6.Koenig HG, Johnson JL, Peterson BL. Major depression and physical illness trajectories in heart failure and pulmonary disease. J Nerv Ment Dis. 2006;194(12):909–16. doi: 10.1097/01.nmd.0000249107.26884.72. [DOI] [PubMed] [Google Scholar]
- 7.Bruce ML, et al. Major depression in elderly home health care patients. Am J Psychiatry. 2002;159(8):1367–74. doi: 10.1176/appi.ajp.159.8.1367. [DOI] [PubMed] [Google Scholar]
- 8.Banerjee S, Macdonald A. Mental disorder in an elderly home care population: associations with health and social service use. Br J Psychiatry. 1996;168(6):750–6. doi: 10.1192/bjp.168.6.750. [DOI] [PubMed] [Google Scholar]
- 9.Beekman AT, et al. The natural history of late-life depression: a 6-year prospective study in the community The impact of depression on the well-being, disability and use of services in older adults: a longitudinal perspective. Arch Gen Psychiatry. 2002;59(7):605–11. doi: 10.1001/archpsyc.59.7.605. [DOI] [PubMed] [Google Scholar]
- 10.Buys L, et al. Prevalence and predictors of depressive symptoms among rural older Australians and Americans. Aust J Rural Health. 2008;16(1):33–9. doi: 10.1111/j.1440-1584.2007.00948.x. [DOI] [PubMed] [Google Scholar]
- 11.Andreescu C, et al. Twelve-year depressive symptom trajectories and their predictors in a community sample of older adults. Int Psychogeriatr. 2008;20(2):221–36. doi: 10.1017/S1041610207006667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Admininistration A. Elderly Nutrition Program. 2003. [Google Scholar]
- 13.Gruber-Baldini AL, et al. Behavioral Symptoms in Residential Care/Assisted Living Facilities: Prevalence, Risk Factors, and Medication Management. Journal of the American Geriatrics Society. 2004;52(10):1610–1617. doi: 10.1111/j.1532-5415.2004.52451.x. [DOI] [PubMed] [Google Scholar]
- 14.Kroenke K, Spitzer RL. The PHQ-9: A New Depression Diagnostic and Severity Measure. Psychiatric Annals. 2002;32:509–15. [Google Scholar]
- 15.Voaklander DC, et al. Medical illness, medication use and suicide in seniors: a population-based case control study. J Epidemiol Community Health. 2008;62(2):138–46. doi: 10.1136/jech.2006.055533. [DOI] [PubMed] [Google Scholar]
- 16.Edwards RR, et al. Acute pain at discharge from hospitalization is a prospective predictor of long-term suicidal ideation after burn injury. Arch Phys Med Rehabil. 2007;88(12 Suppl 2):S36–42. doi: 10.1016/j.apmr.2007.05.031. [DOI] [PubMed] [Google Scholar]
- 17.Snowden M, Steinman L, Frederick J. Treating depression in older adults: challenges to implementing the recommendations of an expert panel. Prev Chronic Dis. 2008;5(1):A26. [PMC free article] [PubMed] [Google Scholar]


