Figure 2. Effects of immunosuppression on allograft success, as assessed by tissue morphology.
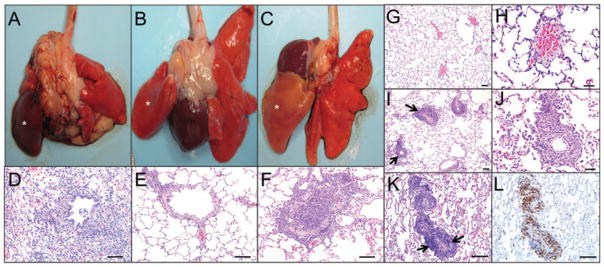
(A) Left lung allograft (indicated by asterisk) from a recipient that was not treated with immunosuppressive drugs; donor lung is dark red (10 days posttransplantation). (B) Left lung allograft (indicated by asterisk) from a recipient that received high dose of immunosuppressive drugs (45 days posttransplantation); donor lung is normal at the gross level. (C) Left lung allograft (indicated by asterisk) in a recipient that received tapered immunosuppression (45 days posttransplantation); donor lung appears pale. (D–F) Histology of the allografts from the panels above. (D) Severe acute rejection with necrosis and inflammatory cell infiltration (neutrophils and macrophages) in allograft. (E) Allograft with no rejection. (F) Allograft with airway occlusion by lymphocyte infiltration and collagen deposition. Lymphocytes extend into the adjacent alveolar septa and alveoli. (G–L) Acute vascular rejection in allografts. (G and H) Histology of the allograft from a control animal maintained on high dose suppression with no signs of rejection and lack of perivascular cuffing. (I–L) At 4 weeks posttransplant, azathioprine and methyl prednisone dosing was reduced by 50% and the animal developed an abnormal CT 4 weeks later at which time the animal was sacrificed. (I) Histology of an allograft from an animal with tapered immunosuppressive drugs demonstrating perivascular lymphocytic cuffs (arrows) characteristic of acute vascular rejection. (J) Higher magnification of the perivascular cuffs. (K and L) Serial sections of allograft with H&E stain and CD3-stain, demonstrating the predominance of T lymphocytes in the perivascular cuffs (arrows) (D–F bars, 100 μm; G, I, K, L bars, 100 μm; H, J bars, 50 μm).
