Abstract
Background:
The health-related quality of life (HRQOL) measures serve as valuable indicators of survival in patients with newly diagnosed primary brain tumors (PBTs). HRQOL outcomes may benefit clinical decision-making by individualizing patient treatment and improving communications between the doctor, patient, and families. Exploring the individual items of the European Organization and Research and Treatment of Cancer Quality of Life Questionnaire (EORTC QOL) measures may be predictive of prognosis.
Methods:
We prospectively collected the validated HRQOL and standard clinical and radiological measures from 48 patients with newly diagnosed PBT. The patients were followed every 3 months over 2 years. No proxies were allowed. Questionnaire responses were compared between two groups: Patients with recurrence and/or death (n = 26) and patients without a recurrence (n = 22). A total of 17 patients succumbed to a tumor-related death. Statistical analysis utilizing nonparametric t-tests and Wilcoxon sign tests assessed QOL responses.
Results:
Significant group differences were noted in the QOL measures with more negative responses in the recurrence group. EORTC QLQ-C30 questions revealed a poor global HRQOL scale (P < 0.005) and pain interfering with daily activities (P < 0.05). EORTC QLQ-BN20 questions revealed weakness of the legs (P < 0.05), coordination difficulties (P < 0.005), and unsteady gait (P < 0.05). Hospital Anxiety and Depression Scale (HADS) questions reflected a patient who is slowed down (P < 0.01) and “frightened” (P < 0.05).
Conclusion:
Our analysis of longitudinal HRQOL measures may shed light on the prognostic significance of HRQOL measures in patients with newly diagnosed PBT. Further research is warranted to determine which selected individual measures of the EORTC QOL measures may be predictive of a patient's progression-free and overall survival and to test their validity and reliability in clinical trials.
Keywords: Brain tumor, malignant, prognostic factor, quality of life
INTRODUCTION
Approximately 18,000 patients are diagnosed with malignant primary brain tumors (PBTs) annually in the United States.[24] Glioblastoma multiforme (GBM) represents the most common malignant brain tumor in adults.[24] Patients with GBM have a poor median survival of one year despite surgical resection followed by radiation with or without concurrent chemotherapy.[29,42]
Maintaining a good QOL becomes an important outcome priority in patients with malignant brain tumors whose survival is limited by tumor resistance to treatment. In addition to standard prognostic indicators such as histology and clinical stage, health-related quality of life (HRQOL) information plays a valuable role in predicting survival or survival duration.[3,8,34] Collecting QOL data could be a feasible method for evaluating the impact of care on a patient's QOL.[17] Intuitively treating a patient's disease over time while addressing his/her QOL should result in maintained or improved functioning and enhanced symptom relief. There is a need to identify practical approaches that are useful and efficient to encourage and maintain clinicians’ and patients’ participation in selecting successful models of integrating QOL assessment into the clinical setting.[22]
HRQOL outcomes may aid in clinical decision-making by providing prognostic data and individualizing patient treatment as well as enhancing communication between doctor, patient, and families.[34,44] HRQOL prognostic factors may also be utilized to assign patients into randomized controlled trials and to better assess study outcome.[34] It has been suggested that patient-reported outcomes (PROs) may be better predictors of survival than performance status and that interventions, which improve PROs, may have the potential to increase survival.[23]
The terms “QOL” and, more specifically, “HRQOL” refer to emotional, physical, cognitive, and social functioning as well as spiritual well-being, which are distinct areas influenced by a person's experience, beliefs, expectations, and perceptions.[45] There is a general consensus that the QOL measures should be completed by the patient due to the subjective nature of the questions that reflect the patient's well-being.
The components of the HRQOL may represent independent predictors of survival and may be beneficial when used clinically to make treatment decisions.[7] Several studies in the literature on PBT have focused on the role of specific facets that may serve as significant prognostic factors of survival such as gender, cognitive and social functioning, depression, tumor location, and histological classification.[16,19,33,36] We have designed a study to attempt to determine which items of the EORTC QOL measures may be significant predictors of tumor progression on magnetic resonance imaging (MRI).
The current manuscript describes a feasibility and exploratory study of quality of life (QOL) measures in patients who were diagnosed with PBTs. We conducted a prospective longitudinal study of collecting QOL measures using the European Organization and Research and Treatment of Cancer Quality of Life Questionnaire Core 30 (EORTC QLQ-C30), the associated EORTC Brain Cancer module BN20 (EORTC QLQ-BN20), and Hospital Anxiety and Depression Scale [HADS]) coupled with clinical standards of care (brain MRI, clinical history, and physical examinations) in patients with newly diagnosed PBT. Questionnaire responses were compared between two groups: Patients with tumor recurrence and/or tumor-related death and patients without a recurrence. We determined the questions in the three measures that were significant between the two groups at each questionnaire time point and over all questionnaire times. We also examined the QOL measures over time as related to tumor progression, whether the QOL measures were predictive of the outcome, and explored which items of the QOL measures may be predictive of radiological progression by comparing the questionnaire responses from patients who experienced a brain tumor recurrence to those who did not.
MATERIALS AND METHODS
Under an institutional review board (IRB)-approved protocol, we prospectively collected the validated HRQOL measures and standard clinical measures from 48 patients with newly diagnosed PBT. This was a single center study performed by the neuro-oncology service. All patients were evaluated by the same neuro-oncologist. The standard of care following surgical resection of the PBT was determined by the tumor type. The tumor types were divided into three categories: Low-grade glioma (LGG), Grade III glioma, and GBM. A single patient was diagnosed with a medulloblastoma. Patients who were diagnosed with a GBM underwent standard treatment of surgery followed by radiation and temozolomide. Patients with a LGG were observed following surgery, and those with a grade III glioma underwent surgery followed by radiation. Tumor progression was defined as radiological progression on MRI scan.
The patients underwent clinical evaluations and brain MRIs every 3 months over 2 years. No proxies were used. In this respect, the patient completed all the survey questions without introducing proxy bias in the responses. All patients provided informed consent before starting the study. Patients answered the surveys prior to each office visit.
A checklist was devised that ensured the completion of each aspect of patient care: MRI, blood work, study questionnaires, and an appointment with the neuro-oncologist. Through this diligence, the present study was able to attain a 95% response rate for the surveys that significantly minimized the serious problem of missing data points that is common to QOL studies in this patient population.
We performed a prospective longitudinal collection of HRQOL measures (EORTC QLQ-C30, EORTC QLQ-BN20, and HADS) along with standard clinical information (brain MRI, clinical history, and physical examinations) used for the care of patients with newly diagnosed PBT. A database was developed to collect patient data.
EORTC QLQ-C30, EORTC QLQ-BN20, and HADS measures
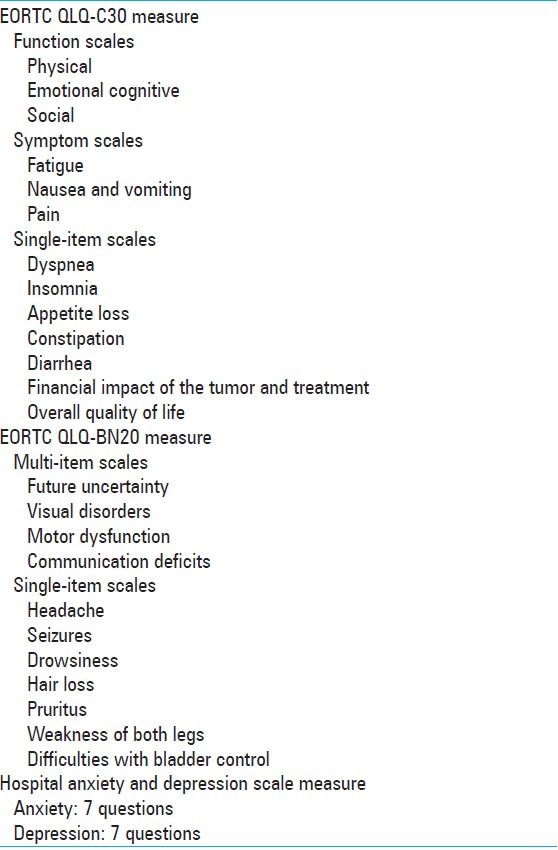
A baseline QOL measurement was gathered for each patient, which was comprised of three measures. The QLQ-C30 is a 30-item, self-reported questionnaire [Table 1].[12,16] The EORTC QLQ-BN20 was developed for patients with brain cancer and includes 20 questions [Table 1].[12,16,43] The QLQ-BN20 demonstrates sufficient psychometric properties and is used in conjunction with the QLQ-C30 for assessing the HRQOL of brain cancer patients in international studies.[43] The HADS is a self-assessment scale that has been proven to be a reliable instrument to detect symptom severity of depression and anxiety in patients undergoing treatment in medical and surgical fields and in the general population.[6,28,46] It is sensitive to changes during the course of diseases and in response to psychotherapeutic and psychopharmacological treatment.[26] HADS scores have been shown to predict psychosocial behavior and physical outcome.[26] The specific questions and scoring systems of the three measures may be found on the EORTC QOL website: http://groups.eortc.be/qol[2]
Table 1.
Description of EORTC QLQ-C30, EORTC QLQ-BN20, and Hospital Anxiety and Depression Scale [HADS] Measures
Analysis
Questionnaire responses were compared between the two tumor groups of patients: Patients with tumor recurrence and/or died (n = 26) and patients without a recurrence (n = 22). Using nonparametric t-tests (Mann-Whitney U test), the ranks of the scores were compared between the groups at each time point.[41] To determine whether there was a similar pattern in the responses over all questionnaire times between the two tumor groups, a Wilcoxon Sign test was performed.[41] Age and gender demographics among the patients groups were compared using independent t-tests for means with equal or unequal variances, as appropriate.[25] Data were analyzed using the statistical software program IBM SPSS, Version 19, 2012.[1] All values are expressed as mean ± SD.
The data in this study was categorical due to the range of patient questionnaire responses only from 1 to 4. Nonparametric analysis procedures are used with small-range categorical data instead of parametric analysis of means and standard deviations. We present the data in a table form rather than as a graph of means and standard deviations. Means and standard deviations were not compared in the analyses. Additionally, there was high variability in the patients’ responses, and the sample sizes decreased when patients were divided into groups.
The data analysis was 2-fold. The responses of the three measures were compared between the two groups of patients. The initial analysis involved the determination of the questions, which showed significant group differences at each assessment time point. Subsequently, the questions on the three measures with significant group differences at each time point underwent further analysis to determine whether there was a similar pattern in the responses overall assessment time points between the two tumor groups. In this study, we have focused our statistical analysis on individual items within each of the QOL measures (EORTC QLQ-C30, EORTC QLQ-BN20, and HADS) and not scale scores.
RESULTS
Age and gender demographics
Between January 2003 and December 2004, 48 patients were enrolled in our study following the diagnosis and surgical resection of a PBT. A total of 17 patients succumbed to a tumor-related death. The patients were divided into two groups: Patients with tumor recurrence and/or died (n = 26) and patients without a recurrence (n = 22).
Table 2 highlights the age and gender demographics of the 48 patients enrolled in this study. The age and gender are presented as a (1) composite tabulation, (2) for patients with a recurrence and/or died, and (3) for patients with no recurrence. The latter two categories are divided by tissue type of the PBTs: GBM, Grade III glioma, and LGG. The mean age in the group of patients with a recurrence and/or died was substantially greater for patients with a GBM compared with LGG. In addition, the mean age of patients with no recurrence was lower for patients with a LGG compared with GBM.
Table 2.
Age and gender demographics with tumor tissue type in patients with a primary brain tumor
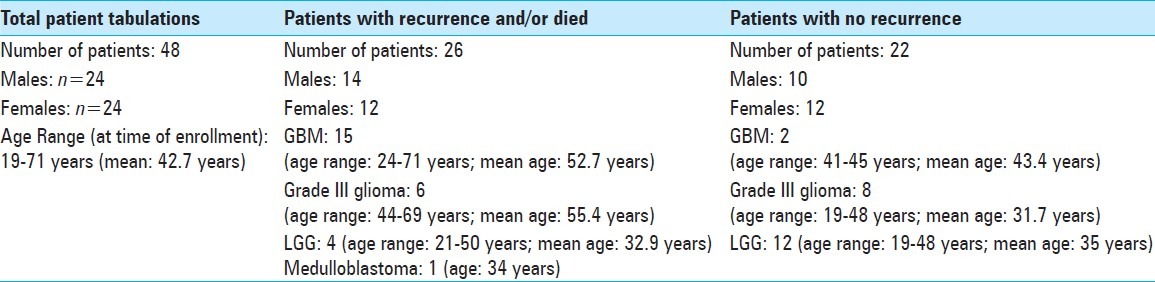
Tissue type of primary brain tumors
Table 2 also reflects the tissue types of the PBTs for the 48 patients in this study. The group of patients who experienced a recurrence and/or death had a significantly greater number of HGG compared with the group that did not have a recurrence. In addition, a higher number of LGG were noted in the group without a recurrence compared with the group with recurrence and/or death.
The EORTC QLQ-C30 measure
The responses of the EORTC QLQ-C30 measure were compared between the two groups. The questions with significant group differences at specific questionnaire time points are displayed in Table 3. More negative responses were noted in the tumor recurrence and/or died group compared with the patient group without a recurrence. The majority of significant differences were observed in the earlier time points when there were more respondents. The questions with significant or near-significant group differences over all questionnaire times are shown in Table 4.
Table 3.
Significant group differences (Recurrence vs Non-Recurrence) at each time point on the EORTC QLQ-C30 and QLQ-BN20 measures and the Hospital Anxiety and Depression Scale (HADS) in patients with a primary brain tumor
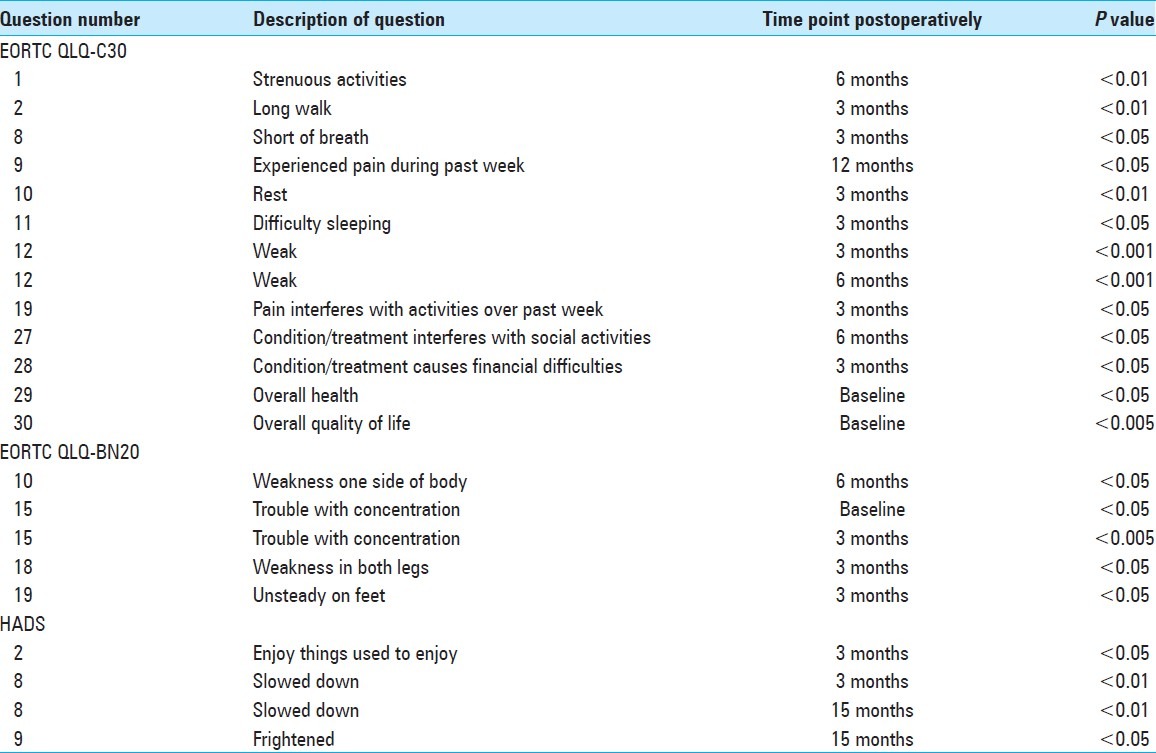
Table 4.
Significant group differences (Recurrence vs. Non-Recurrence) over all questionnaire times on the EORTC QLQ-C30 and QLQ-BN20 measures and the Hospital Anxiety and Depression Scale (HADS) in patients with a primary brain tumor
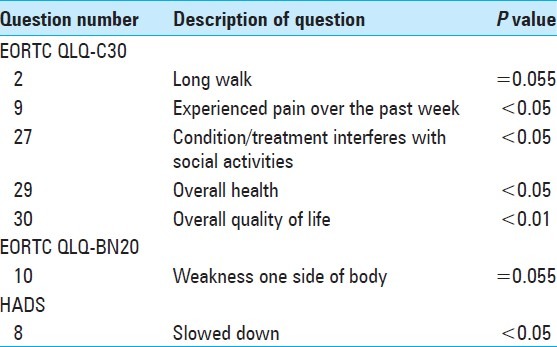
Of the 26 patients who experienced a recurrence and/or death, the duration of time between the first assessment at the postoperative baseline and either recurrence and/or death was 29 weeks for a GBM, 53 weeks for a Grade III glioma, 66 weeks for a medulloblastoma, 75 weeks for a LGG, with a total mean duration of 43.1 weeks (approximately 10 months).
The EORTC QLQ-BN20 measure
The responses of the EORTC QLQ-BN20 measure were compared between the two groups of patients. The questions with significant group differences at specific questionnaire time points are highlighted in Table 3. The question with near-significant group differences over all questionnaire times is shown in Table 4.
The Hospital Anxiety and Depression [HADS] scale
The questions with significant group differences at specific questionnaire time points are shown in Table 3. The question with significant group differences over all questionnaire times is presented in Table 4.
DISCUSSION
Numerous studies have addressed a patient's QOL after undergoing resection for a PBT.[7,11,12,15,16,18,19,27,30,32,33,35–37,39,40,43,44] Corn et al. studied the QOL and cognitive status of patients with GBM who received escalating doses of radiation.[18,19] They reported that the baseline life quality, in particular a patient's sense of independence, was highly predictive of survival. They noted a continual decline in cognitive function in their population group. Bampoe et al. conducted a study of QOL measures as a component of a randomized clinical trial of brachytherapy as a boost in the initial treatment of patients with GBM.[4] They reported statistically significant deteriorations in overall Karnofsky Performance Scale (KPS) scores and in self care, speech, concentration, and cognitive functioning during the first year of follow-up compared with baseline values.[4]
Brown et al. conducted a prospective study of the baseline QOL in adults with newly diagnosed high-grade gliomas.[11] They concluded that fatigue was an independent predictor of overall survival, specifically, that increased fatigue predicted poorer overall survival. Based on their findings, they recommended implementing interventional therapies that may combat fatigue, which may subsequently enhance survival. Budrukkar et al. performed a comprehensive prospective study of QOL in adults with PBT replete with the EORTC questionnaires and patient and tumor factors.[12] Prior to initiating adjuvant therapy, patients with PBT had low baseline QOL scores, especially in lower economic and literacy groups. Furthermore, patients with malignant tumors and poor performance status (KPS < 70) had significantly lower QOL scores before starting adjuvant treatment.[12] Mainio et al. performed a long-term (1 and 5 years postoperatively) follow-up study of patients with LGGs.[33] They concluded that depression and decreased QOL among LGG patients are associated with shorter survival at long-term follow-up. Decreased QOL may represent an indicator for poor prognosis in LGG patients.
In their study of QOL of long-term high-grade glioma patients, Bosma et al. showed that there was no difference in QOL at baseline between short-term and long-term survivors.[7] However, the QOL of short-term survivors deteriorated between baseline and the 4-month follow-up while the physical functioning of long-term survivors improved to a level seen by healthy controls. We have shown in this exploratory study that individual QOL measures were predictive of recurrence not only in the patients with histological diagnosis of GBM but also in approximately half the patients with anaplastic grade III glioma.
This study provides a unique analysis of the specific questions of the universally accepted EORTC questionnaires and HADS measures in patients with PBT. By determining the time points postoperatively when significant differences in the daily activities of life between the recurrence and nonrecurrence groups occur, patient care may be individualized to address these issues. It may be valuable for the treating neurologist to be aware of the myriad time points when a patient with a tumor recurrence may experience a host of symptoms that may affect his/her HRQOL or activities of daily living where clinical progression may predict tumor recurrence prior to radiological progression. In their study of 565 patients with grade III or IV malignant glioma, Chang et al. reported that headaches were the initial symptom in 53% of patients with Grade III and 57% in Grade IV glioma.[14] In our study, there were significant group differences (recurrence vs nonrecurrence) with respect to headaches at the 3 and 12 month time points postoperatively. Furthermore, there were also significant group differences concerning weakness of the legs and unsteadiness on the feet at the 3 month time point postoperatively. The treating neurologist should be astute to these symptoms at these time points and recommend appropriate treatment, including interventional physical therapy.
Numerous complaints may be predictive of tumor recurrence such as dyspnea, pain that interferes with activities, and financial difficulties (reflected by the EORTC QLQ-C30); difficulty with concentration and weakness of the lower extremities (per the EORTC QLQ-BN20); and being slowed down (discerned by the HADS). It is interesting to note that a patient's perception of his/her overall QOL was a significant group difference (recurrence vs nonrecurrence) in the EORTC QLQ-C30 measure at baseline and over all questionnaire time points.
Our goal in this study was to explore whether QOL scores may predict tumor progression observed on MRI. In our study, the distribution of scores was too small to determine whether individual scores were predictive of recurrence. Due to the small sample size, we were unable to discern whether scales or individual items in the QOL measures were predictive of PFS or OS. Future studies with a larger patient population will prove more successful in elucidating these goals.
It has been noted that a brain cancer patient's QOL, after the diagnosis of cancer, represents an important aspect of an individual's care. In addition to surgery, chemotherapy and/or radiation, and imaging studies, the QOL represents a prognostic indicator in numerous types of cancer, including brain,[7,11,12,15,16,18,19,27,30,32,33,35–37,39,40,43,44] breast,[10,31] lung,[9,21,38] pancreatic,[5] and renal cell carcinoma.[13] A common theme permeates these various types of cancer, specifically, that self-reported HRQOL parameters serve as valuable and independent predictors for survival. Analysis of a patient's HRQOL is not only utilized in the management and care of cancer patients, it has also been incorporated into the medical evaluation of other life-altering conditions such as traumatic brain injury.[20]
While QOL measurements are simple to perform, reproducible, and efficacious, imaging studies are the gold standard in the postoperative care of PBTs. QOL testing has not reached the point of development where it may replace routine imaging studies postoperatively. Imaging studies should be performed following chemotherapy. We recommend that an overall assessment of a patient should not only include imaging studies but also QOL measures to determine adverse side effects of chemotherapy.
Our study has several limitations. The sample size is a limiting factor that can influence how our results may be generalized. In a future study with a larger sample size and longer duration, correlation between the predictive power of HRQOL measures and patients’ age and histology will be better explored. While the patients in the present study were recruited a decade ago, a host of factors have remained the same over the past decade, specifically, the histologic grading system. In addition, the treatment protocol has not changed drastically. This study was performed in an era of standard therapy of concurrent radiation and temozolomide for the treatment of GBM, which makes the results pertinent to the current environment.
The current manuscript describes a feasibility and exploratory study of QOL measures in patients who were diagnosed with PBTs. The design of a future study will include a balance of baseline features including residual disease, tumor location, steroid and antiepileptic use, a larger number of patients, and a longer follow-up. Future analysis will also closely monitor a patient's QOL in each tumor histologic subtype.
CONCLUSION
The Food and Drug Administration, American Society of Clinical Oncology, and the European Medicine Agency have designated QOL as a key outcome that should often be considered alongside survival data. QOL serves as an important outcome priority in patients with malignant brain tumors whose survival is limited by tumor resistance to treatment. The utilization of QOL in clinical practice could lead to improved patient–physician communication and relationship, patient's participation in decision-making, and patient satisfaction with care. The results of our sample suggest that patients with PBT may have many important impaired areas and that the clinician should be aware of these needs and aggressively treat these patients. Responses to QOL measures by patients with a PBT may elucidate the impact of cancer on a patient's QOL. More negative responses to the questions were noted in the tumor recurrence group compared with the patient group without a recurrence.
Additional research is warranted to integrate QOL measurements into the standard care of patients with a PBT. A future goal is to determine whether the change in the QOL questions may be predictive of PFS and/or OS.
ACKNOWLEDGMENTS
The authors acknowledge Norton Healthcare, Louisville, KY and Deseret Research Foundation, Intermountain Healthcare, Salt Lake City, UT. The authors also acknowledge Christopher B. Shields, M.D. and Andrew Bottomley, Ph.D. for their valuable contributions to this manuscript.
Footnotes
Available FREE in open access from: http://www.surgicalneurologyint.com/text.asp?2013/4/1/48/110143
Contributor Information
Lisa B. E Shields, Email: LBES@earthlink.net.
Aliisha Choucair, Email: aliishakc@gmail.com.
Ali K. Choucair, Email: ali.choucair@nortonhealthcare.org.
REFERENCES
- 1.Armstrong TS, Wefel JS, Wang M, Won M, Bottomley A, Mendoza TR, et al. Clinical utility of neurocognitive function (NCF), quality of life (QOL), and symptom assessment as prognostic factors for survival and measures of treatment effects on RTOG 0525. American Society of Clinical Oncology. 2011;29 Abstract. [Google Scholar]
- 2.Bampoe J, Laperriere N, Pintilie M, Glen J, Micallef J, Bernstein M. Quality of life in patients with glioblastoma multiforme participating in a randomized study of brachytherapy as a boost treatment. J Neurosurg. 2000;93:917–26. doi: 10.3171/jns.2000.93.6.0917. [DOI] [PubMed] [Google Scholar]
- 3.Bernhard J, Dietrich D, Glimelius B, Hess V, Bodoky G, Scheithauer W, et al. Estimating prognosis and palliation based on tumour marker CA 19-9 and quality of life indicators in patients with advanced pancreatic cancer receiving chemotherapy. Br J Cancer. 2010;103:1318–24. doi: 10.1038/sj.bjc.6605929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bjelland I, Dahl AA, Haug TT, Neckelmann D. The validity of the Hospital Anxiety and Depression Scale.An updated literature review. J Psychosom Res. 2002;52:69–77. doi: 10.1016/s0022-3999(01)00296-3. [DOI] [PubMed] [Google Scholar]
- 5.Bosma I, Reijneveld JC, Douw L, Vos MJ, Postma TJ, Aaronson NK, et al. Health-related quality of life of long-term high-grade glioma survivors. Neuro Oncol. 2009;11:51–8. doi: 10.1215/15228517-2008-049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bottomley A, Efficace F. Predicting survival in advanced cancer patients: Is it possible with patient-reported health status data? Ann Oncol. 2006;17:1037–8. doi: 10.1093/annonc/mdl123. [DOI] [PubMed] [Google Scholar]
- 7.Braun DP, Gupta D, Staren ED. Quality of life assessment as a predictor of survival in non-small cell lung cancer. BMC Cancer. 2011;11:353. doi: 10.1186/1471-2407-11-353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bredal IS, Sandvik L, Karesen R, Ekeberg O. Prognostic value of health-related quality-of-life parameters in early-stage breast cancer: An 8-year follow-up study. Psychooncology. 2011;20:1102–7. doi: 10.1002/pon.1822. [DOI] [PubMed] [Google Scholar]
- 9.Brown PD, Maurer MJ, Rummans TA, Pollock BE, Ballman KV, Sloan JA, et al. A prospective study of quality of life in adults with newly diagnosed high-grade gliomas: The impact of the extent of resection on quality of life and survival. Neurosurgery. 2005;57:495–504. doi: 10.1227/01.neu.0000170562.25335.c7. [DOI] [PubMed] [Google Scholar]
- 10.Budrukkar A, Jalali R, Dutta D, Sarin R, Devlekar R, Parab S, et al. Prospective assessment of quality of life in adult patients with primary brain tumors in routine neurooncology practice. J Neurooncol. 2009;95:413–9. doi: 10.1007/s11060-009-9939-8. [DOI] [PubMed] [Google Scholar]
- 11.Cella D. Beyond traditional outcomes: Improving quality of life in patients with renal cell carcinoma. Oncologist. 2011;23:31. doi: 10.1634/theoncologist.2011-S2-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chang SM, Parney IF, Huang W, Anderson FA, Jr, Asher Al, Bernstein M, et al. Patterns of care for adults with newly diagnosed malignant glioma. JAMA. 2005;293:557–64. doi: 10.1001/jama.293.5.557. [DOI] [PubMed] [Google Scholar]
- 13.Cheng JX, Liu BL, Zhang X, Lin W, Zhang YQ, Liu WP, et al. Health-related quality of life in glioma patients in China. BMC Cancer. 2010;10:305. doi: 10.1186/1471-2407-10-305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cheng JX, Zhang X, Liu BL. Health-related quality of life in patients with high-grade glioma. Neuro Oncol. 2009;11:41–50. doi: 10.1215/15228517-2008-050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Choucair AK, Scott C, Urtasun R, Nelson D, Mousas B, Curran W. Quality of life and neuropsychological evaluation for patients with malignant astrocytomas: RTOG 91-14.Radiation Therapy Oncology Group. Int J Radiat Oncol Biol Phys. 1997;38:9–20. doi: 10.1016/s0360-3016(97)00223-x. [DOI] [PubMed] [Google Scholar]
- 16.Corn BW, Moughan J, Knisely JP, Fox SW, Chakravarti A, Yung WK, et al. Prospective evaluation of quality of life and neurocognitive effects in patients with multiple brain metastases receiving whole-brain radiotherapy with or without thalidomide on Radiation Therapy Oncology Group (RTOG) trial 0118. Int J Radiat Oncol Biol Phys. 2008;71:71–8. doi: 10.1016/j.ijrobp.2007.09.015. [DOI] [PubMed] [Google Scholar]
- 17.Corn BW, Wang M, Fox S, Michalski J, Purdy J, Simpson J, et al. Health related quality of life and cognitive status in patients with glioblastoma multiforme receiving escalating doses of conformal three dimensional radiation on RTOG 98-03. J Neurooncol. 2009;95:247–57. doi: 10.1007/s11060-009-9923-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Diaz AP, Schwarzbold ML, Thais ME, Hohl A, Bertotti MM, Schmoeller R, et al. Psychiatric disorders and health-related quality of life after severe traumatic brain injury: A prospective study. J Neurotrauma. 2012;29:1029–37. doi: 10.1089/neu.2011.2089. [DOI] [PubMed] [Google Scholar]
- 19.Efficace F, Bottomley A, Smit EF, Lianes P, Legrand C, Debruyne C, et al. Is a patient's self-reported health-related quality of life a prognostic factor for survival in non-small-cell lung cancer patients? A multivariate analysis of prognostic factors of EORTC study 08975. Ann Oncol. 2006;17:1698–704. doi: 10.1093/annonc/mdl183. [DOI] [PubMed] [Google Scholar]
- 20.EORTC Quality of Life. Electronic Citation. [Accessed: February 21, 2013].
- 21.Frost MH, Bonomi AE, Cappelleri JC, Schunemann HJ, Moynihan TJ, Aaronson NK. Applying quality-of-life data formally and systematically into clinical practice. Mayo Clin Proc. 2007;82:1214–28. doi: 10.4065/82.10.1214. [DOI] [PubMed] [Google Scholar]
- 22.Gotay CC, Kawamoto CT, Bottomley A, Efficace F. The prognostic significance of patient-reported outcomes in cancer clinical trials. J Clin Oncol. 2008;26:1355–63. doi: 10.1200/JCO.2007.13.3439. [DOI] [PubMed] [Google Scholar]
- 23.Grossman SA, Batara JF. Current management of glioblastoma multiforme. Semin Oncol. 2004;31:635–44. doi: 10.1053/j.seminoncol.2004.07.005. [DOI] [PubMed] [Google Scholar]
- 24.Hays W. Statistics. New York: Holt, Rinehart and Winston; 1981. [Google Scholar]
- 25.Herrmann C. International experiences with the Hospital Anxiety and Depression Scale: A review of validation data and clinical results. J Psychosom Res. 1997;42:17–41. doi: 10.1016/s0022-3999(96)00216-4. [DOI] [PubMed] [Google Scholar]
- 26.IBM SPSS. Version 19. 2012. Computer Program [Google Scholar]
- 27.Jakola AS, Unsgard G, Solheim O. Quality of life in patients with intracranial gliomas: The impact of modern image-guided surgery. J Neurosurg. 2011;114:1622–30. doi: 10.3171/2011.1.JNS101657. [DOI] [PubMed] [Google Scholar]
- 28.Kandasamy A, Chaturvedi SK, Desai G. Spirituality, distress, depression, anxiety, and quality of life in patients with advanced cancer. Indian J Cancer. 2011;48:55–9. doi: 10.4103/0019-509X.75828. [DOI] [PubMed] [Google Scholar]
- 29.Lacroix M, Abi-Said D, Fourney DR, Gokaslan ZL, Shi W, DeMonte F, et al. A multivariate analysis of 416 patients with glioblastoma multiforme: Prognosis, extent of resection, and survival. J Neurosurg. 2001;95:190–8. doi: 10.3171/jns.2001.95.2.0190. [DOI] [PubMed] [Google Scholar]
- 30.Lakicevic G, Splavski B, Brekalo Z. The value of stereotactic biopsy in improving survival and quality of life for malignant brain glioma patients. Coll Antropol. 2010:93–7. [PubMed] [Google Scholar]
- 31.Lee CK, Stockler MR, Coates AS, Gebski V, Lord SJ, Simes RJ. Self-reported health-related quality of life is an independent predictor of chemotherapy treatment benefit and toxicity in women with advanced breast cancer. Br J Cancer. 2010;102:1341–7. doi: 10.1038/sj.bjc.6605649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Liu R, Solheim K, Polley MY, Lamborn KR, Page M, Fedoroff A, et al. Quality of life in low-grade glioma patients receiving temozolomide. Neuro Oncol. 2009;11:59–68. doi: 10.1215/15228517-2008-063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mainio A, Tuunanen S, Hakko H, Niemela A, Koivukangas J, Rasanen P. Decreased quality of life and depression as predictors for shorter survival among patients with low-grade gliomas: A follow-up from 1990 to 2003. Eur Arch Psychiatry Clin Neurosci. 2006;256:516–21. doi: 10.1007/s00406-006-0674-2. [DOI] [PubMed] [Google Scholar]
- 34.Mauer M, Bottomley A, Coens C, Gotay C. Prognostic factor analysis of health-related quality of life data in cancer: A statistical methodological evaluation. Expert Rev Pharmacoecon Outcomes Res. 2008;8:179–96. doi: 10.1586/14737167.8.2.179. [DOI] [PubMed] [Google Scholar]
- 35.Mauer M, Stupp R, Taphoorn MJ, Coens C, Osoba D, Marosi C, et al. The prognostic value of health-related quality-of-life data in predicting survival in glioblastoma cancer patients: Results from an international randomised phase III EORTC Brain Tumour and Radiation Oncology Groups, and NCIC Clinical Trials Group study. Br J Cancer. 2007;97:302–7. doi: 10.1038/sj.bjc.6603876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Mauer ME, Taphoorn MJ, Bottomley A, Coens C, Efficace F, Sanson M, et al. Prognostic value of health-related quality-of-life data in predicting survival in patients with anaplastic oligodendrogliomas, from a phase III EORTC brain cancer group study. J Clin Oncol. 2007;25:5731–7. doi: 10.1200/JCO.2007.11.1476. [DOI] [PubMed] [Google Scholar]
- 37.McCarter H, Furlong W, Whitton AC, Feeny D, DePauw S, Willan AR, et al. Health status measurements at diagnosis as predictors of survival among adults with brain tumors. J Clin Oncol. 2006;24:3636–43. doi: 10.1200/JCO.2006.06.0137. [DOI] [PubMed] [Google Scholar]
- 38.Movsas B, Moughan J, Sarna L, Langer C, Werner-Wasik M, Nicolaou N, et al. Quality of life supersedes the classic prognosticators for long-term survival in locally advanced non-small-cell lung cancer: An analysis of RTOG 9801. J Clin Oncol. 2009;27:5816–22. doi: 10.1200/JCO.2009.23.7420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Myers WC, Kemph JP. DSM-III-R classification of murderous youth: Help or hindrance? J Clin Psychiatry. 1990;51:239–42. [PubMed] [Google Scholar]
- 40.Ruge MI, Ilmberger J, Tonn JC, Kreth FW. Health-related quality of life and cognitive functioning in adult patients with supratentorial WHO grade II glioma: Status prior to therapy. J Neurooncol. 2011;103:129–36. doi: 10.1007/s11060-010-0364-9. [DOI] [PubMed] [Google Scholar]
- 41.Siegel S, Castellan NJ. Nonparametric statistics for the behavioral sciences. Boston: McGraw Hill; 1988. [Google Scholar]
- 42.Stupp R, Mason WP, van den Bent MJ, Weller M, Fisher B, Taphoorn MJ, et al. Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma. N Engl J Med. 2005;352:987–96. doi: 10.1056/NEJMoa043330. [DOI] [PubMed] [Google Scholar]
- 43.Taphoorn MJ, Claassens L, Aaronson NK, Coens C, Mauer M, Osoba D, et al. An international validation study of the EORTC brain cancer module (EORTC QLQ-BN20) for assessing health-related quality of life and symptoms in brain cancer patients. Eur J Cancer. 2010;46:1033–40. doi: 10.1016/j.ejca.2010.01.012. [DOI] [PubMed] [Google Scholar]
- 44.Taphoorn MJ, Sizoo EM, Bottomley A. Review on quality of life issues in patients with primary brain tumors. Oncologist. 2010;15:618–26. doi: 10.1634/theoncologist.2009-0291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Testa MA, Simonson DC. Assesment of quality-of-life outcomes. N Engl J Med. 1996;334:835–40. doi: 10.1056/NEJM199603283341306. [DOI] [PubMed] [Google Scholar]
- 46.Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67:361–70. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]


