Figure 3.
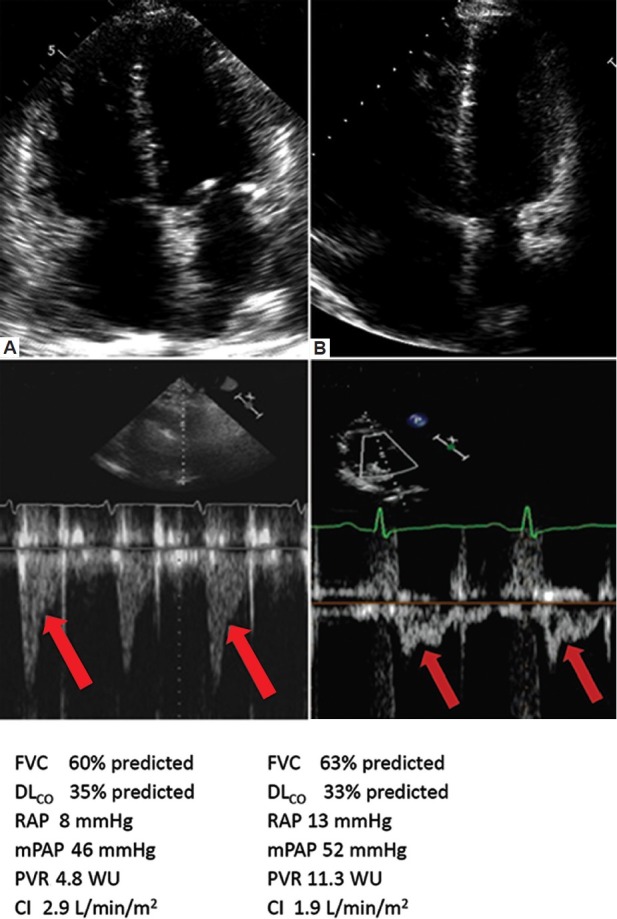
Representative apical four chamber view and Doppler flow velocity envelope (FVE) in right ventricular outflow tract (RVOT). Data were taken from two separate patients: (A) one with PHD I phenotype and (B) one with PHD II phenotype. Below each panel are representative pulmonary function tests and invasive hemodynamics for each patient. Note the greater degree of RVH, and lesser degree of RV dilatation and dysfunction in the patient in panel A vs. panel B. Similarly, the subject in panel A has a late-systolic notch pattern RV outflow tract Doppler pattern, which is consistent with a modest and comparatively lesser degree of RV afterload as compared to the mid-systolic notch pattern seen in the Doppler pattern of the subject in panel B. The subjects had a similar degree of respiratory disease. FVC = forced vital capacity; DLCO = carbon monoxide diffusing capacity; mPAP = mean pulmonary artery pressure; PVR = pulmonary vascular resistance; WU = Wood units; CI = cardiac index. Both patients in Figure 1 had COPD and both were treated with oral PH-specific therapy for 6 months. Patient A (PHD I phenotype) had a fall in 6 MW from 320 m to 300 m and a worsening in NYHA functional class from 3 to 4. RV function improved as evidenced by an increase in TAPSE from 2.0 cm to 2.4 cm and a 40% fall in the BNP level. Patient B (PHD II phenotype) had an increase in 6 MW from 238 m to 320 m with a fall in NYHA functional class from 4 to 3. RV function also improved, as evidenced by an increase in TAPSE from 1.4 cm to 1.9 cm and a 40% fall in the BNP level. Note that in both patients A and B, BNP fell and RV function improved, however only in patient B with the PHD II phenotype did the RV function improvement correlate with overall improvements in clinical status. The differences in clinical response likely relate to the fact the subject with the type II PHD phenotype had a greater degree of RV-PA uncoupling, and thus, a greater degree of functional impairment on the basis of a circulatory limitation. As such, direct PH treatment in this context translates into overall improved functional capacity, even though the background ventilatory limitation remains.
