Abstract
Background
In recent years, the number of acute hospital admissions has increased and this has imposed both organizational and financial strains on the health care system. Consequently, it is of crucial importance that we have valid data on admission types in the administrative databases in order to provide data for health care planning and research.
Objective
To examine the validity of registration of acute admissions among medical patients in the Danish National Patient Registry (DNPR) using medical record reviews as the reference standard.
Methods
We used the nationwide DNPR to identify a sample of 160 medical patients admitted to a hospital in the North Denmark Region during 2009. Data on admission type was obtained from the DNPR and confirmed by a medical record review. We computed positive predictive values, sensitivity, and specificity including 95% confidence intervals (CI) using the medical record review as the reference standard.
Results
Among the 160 medical inpatients identified in the DNPR, 128 were registered with an acute admission, and 32 were registered with a nonacute admission. Two medical records could not be located. Thus, the analyses included 158 medical patients. Among the 127 patients registered with acute admission, 124 were confirmed to be correctly classified. Correspondingly, 28 of the 31 patients with a registered nonacute admission were confirmed to be correctly classified. The overall positive predictive value of the acute admissions among medical patients was 97.6% (95% CI, 93.8%–99.3%). Sensitivity was 97.6% (95% CI, 93.8%–99.3%) and specificity was 90.3% (95% CI, 76.4%–97.2%).
Conclusion
The registration of acute admission among medical patients in the DNPR has high validity.
Keywords: medical patients, registries, epidemiology, positive predictive value, sensitivity, specificity
Introduction
According to Statistics Denmark, acute admissions constitute approximately 70% of all admissions to hospitals in Denmark.1 The total number of acute admissions has increased by 14% in a 5-year period from 2006 to 2010. A similar pattern is reported in many other parts of the world.2–4 The rise in the number of acute admissions imposes both a substantial organizational challenge to and a considerable financial strain on the health care system.
Stratification by admission type is used in studies of prognosis, in the surveillance of health care quality, and in the reimbursement of hospital costs between the hospitals and the state. Valid data on the admission type are therefore pertinent from both an administrative and a research perspective.
To our knowledge, only two national reports evaluating the admission type registered in the Danish National Patient Registry (DNPR) exist.5,6 One was based on a random sample of 1094 hospital admissions in 1990.5 The evaluation covered medical, surgical, gynecological, orthopedic, and pediatric departments at a national level. The acute admissions were correctly classified in 98.6% of the cases. More recently, a second report included a validation of the admission type across surgical and gynecology departments.6 This report estimated a 3% misclassification in admission type. No validation study has specifically examined the registration of admission type in medical patients.
The aim of the present study is to examine the validity of the registration of acute admissions among medical patients in the DNPR using medical record review as the reference standard.
Method
Study design and setting
We conducted this cross-sectional validation study in the North Denmark Region, covering 580,000 inhabitants (10% of the total Danish population). The Danish population has unrestricted and unfettered access to tax-supported health care, guaranteeing equal access to treatment and hospital admission. The six hospitals in the region report all admissions to the DNPR.
Study population
We used the DNPR to identify a sample of 160 medical patients admitted to hospital in the North Denmark Region during 2009. Medical patients were defined as patients with an admission to any of the medical departments in the study area. In the DNPR, admission type is only registered for inpatients. The admission type is assigned by a secretary upon admission and is either acute or nonacute. Each year, the National Board of Health provides a guideline for correct registration. For the purpose of this study, oncology departments were not included because both surgical and nonsurgical cancer patients are referred to this department. The identified medical patients were admitted to15 different medical departments, of which nine were highly specialized departments.
The Danish National Patient Registry
The DNPR contains information on all hospital admissions to nonpsychiatric hospitals since 1977 and all hospital contacts to emergency rooms and outpatient clinics since 1995.7 Information on the admission type has been included in the DNPR since 1987. Besides the admission type, other information includes dates of referral, admission, and discharge, data on the hospital and each department, diagnostic codes, and surgical procedures. Diagnostic codes include one principal diagnosis reflecting the main reason for hospital admission and up to 19 secondary discharge diagnoses coded according to the International Classification of Diseases (ICD), 8th revision until 1993 (ICD-8), and the 10th revision (ICD-10) thereafter. Diagnoses are assigned by the attending physician at the time of discharge. Each hospital electronically transfers administrative and clinical data from their patient administrative system to the DNPR. The DNPR is managed by the National Board of Health, and reporting to the DNPR is mandatory. Based on the Diagnosis Related Group system, information from the DNPR is extracted and used for the purpose of financial reimbursement between the hospitals and the state.
Medical record review
The unique personal identification number assigned to all Danish residents, as well as the hospital and department codes registered for the sampled medical inpatients, were used to retrieve the patients’ medical records for review. Each medical record review was initiated with a verification of the patient’s personal identification number and the date of hospital admission. All medical records were reviewed by the same physician (BVH). Through the review process, we confirmed the admissions to be acute if the attending physician used the word “acute” in the sentences concerning the type and reason for admission, or if it was stated that the admission was unscheduled. All scheduled admissions were considered nonacute admissions. Data on lifestyle factors are usually not available from administrative registries, but may be available from medical records. We therefore included data on smoking status, alcohol abuse (more than 14 or 21 standard drinks in 1 week for women and men, respectively), and weight and height in order to calculate body mass index (BMI) from the medical records to demonstrate availability of these variables. The misclassified acute and nonacute patients were described in terms of their specific characteristics.
Statistical analysis
We described the sample in terms of gender, age, smoking status, alcohol abuse, and BMI. Age was described with the median age and the associated interquartile range (IQR). The concordance between admission type in the DNPR and in the medical records was ascertained with estimates of the positive predictive value (PPV), sensitivity, and specificity with corresponding 95% confidence intervals (CI).8 We estimated 95% CIs using Jeffrey’s method for a binomial proportion.9 Data collected through the medical record review were used as the reference standard.
To estimate the PPV of the registration of acute admissions in the DNPR, we computed the proportion of patients registered in the DNPR with an acute admission which was confirmed by medical record review (ie, the numerator was the number of patients registered with an acute admission in both data sources, and the denominator was the number of patients registered with an acute admission in the DNPR). Sensitivity was estimated with the numerator being the number of patients registered with an acute admission in both data sources, and the denominator being the total number of patients confirmed by medical record review to have an acute admission. The specificity was estimated with the numerator being the number of patients registered with a nonacute admission in both data sources, and the denominator being the total number of patients confirmed by medical record review to have a nonacute admission. Furthermore, we estimated PPV, sensitivity, and specificity for each hospital. In a subsequent analysis, we restricted the analysis to the medical patients arriving through the emergency room to confirm whether the patients were registered with an acute admission when becoming an inpatient. Sensitivity analysis using a different approach was conducted; it included data from the DNPR on the date of referral and date of admission, as the dates are expected to be the same for acute admissions and different for nonacute admissions. Data were analyzed with the statistical software package STATA (version 11; Stata Corp, College Station, TX, USA). The study was approved by The Danish Data Protection Agency (record number 2006-53-1396).
Results
Characteristics
Table 1 displays information on age, smoking, alcohol abuse, and BMI of the patients confirmed by the medical record review to be correctly registered with an acute or nonacute admission in the DNPR. The acute patients were slightly younger (median age of 62 years [IQR 49–80]), on average, than the nonacute patients (median age of 63 years [IQR 52–69]). Among the acute patients, 49.6% were males, in contrast to 67.7% of the nonacute patients. The medical records lacked data on smoking status for only 13.4% of the acute patients and for 16.1% of the nonacute patients. Data on weight and height in order to compute BMI was missing for 47.2% of the acute patients and for 35.4% of the nonacute patients. Data on alcohol abuse were missing for 23.6% of the acute patients and for 51.6% of the nonacute patients (Table 1).
Table 1.
Characteristics of 158 medical hospital admissions in the North Denmark Region in 2009
| Characteristics*
|
Medical hospital admission
|
|
|---|---|---|
| N (% of group)
| ||
| Acute (n = 127) | Nonacute (n = 31) | |
| Sex | ||
| Women | 64 (50.4) | 10 (32.3) |
| Men | 63 (49.6) | 21 (67.7) |
| Age, years | ||
| Median | 62 | 63 |
| IQR | 49–80 | 52–69 |
| Smoking | ||
| Never | 46 (36.2) | 11 (35.5) |
| Current | 32 (25.2) | 6 (19.4) |
| Former | 32 (25.2) | 9 (29.0) |
| Unknown | 17 (13.4) | 5 (16.1) |
| Alcohol abuse | ||
| Never | 86 (67.7) | 14 (45.2) |
| Current | 9 (7.1) | 0 (0.0) |
| Former | 2 (1.6) | 1 (3.2) |
| Unknown | 30 (23.6) | 16 (51.6) |
| Body mass index | ||
| <18.5 | 3 (2.4) | 0 (0.0) |
| ≥18.5 and <25 | 25 (19.7) | 6 (19.4) |
| ≥25 and <30 | 16 (12.6) | 7 (22.6) |
| ≥30 | 23 (18.1) | 7 (22.5) |
| Unknown | 60 (47.2) | 11 (35.4) |
Note:
information collected through the DNPR and medical record review.
Abbreviations: N, number; IQR, interquartile range; DNPR, Danish National Patient Registry.
Medical record review process
All 160 sampled inpatients had a registration of either acute or nonacute admission in the DNPR. In total, 128 (80.0%) were registered as acute and 32 (20.0%) were registered as nonacute admissions in the DNPR. In the review process, two medical records could not be located and these admissions were therefore not included in the analysis. A flowchart of the medical record review process is outlined in Figure 1.
Figure 1.
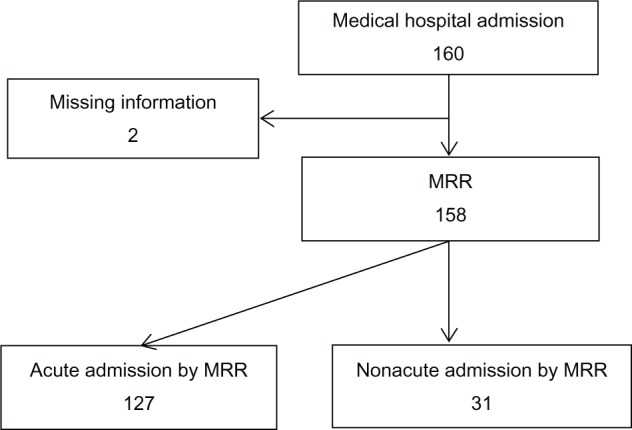
Flowchart of the medical record review (MMR) process.
PPV, sensitivity, and specificity
The final study population, on which the estimates were computed, included 158 medical inpatients, of which 127 were registered in the DNPR with an acute admission and 31 with a nonacute admission. Of the 127 medical patients registered with an acute admission, we confirmed 124 to be an acute admission based on our review of the medical records. Among the three nonconfirmed acute admissions, one was rescheduled for the following day and two were scheduled admissions. Of the 31 medical patients registered with a nonacute admission in the DNPR, three should have been registered with an acute admission. All three were referred for an acute admission by their general practitioner. The overall PPV of acute admissions was 97.6% (95% CI, 93.8%–99.3%) when using the medical record review as the reference standard. Sensitivity was 97.6% (95% CI, 93.8%–99.3%) and specificity was 90.3% (95% CI, 76.4%–97.2%) (Table 2). The analysis stratified by each hospital did not yield any major differences in results (data not shown). When restricting the analysis to the 21 patients who visited the emergency room before admission, we confirmed that all 21 patients were correctly registered with an acute admission in the DNPR.
Table 2.
Estimation of PPV, sensitivity, and specificity
| DNPRa | Medical record review
|
||
|---|---|---|---|
| Acute | Nonacute | In total | |
| Acute | 124 | 3 | 127 |
| Nonacute | 3 | 28 | 31 |
| In total | 127 | 31 | 158 |
| Results (95% confidence intervals) | |||
|
| |||
| PPV (TP/(TP+FP)) | 97.6% (93.8%–99.3%) | ||
| Sensitivity (TP/(TP+FN)) | 97.6% (93.8%–99.3%) | ||
| Specificity (TN/(TN+FP)) | 90.3% (76.4%–97.2%) | ||
Note:
The Danish National Patient Registry.
Abbreviations: PPV, positive predictive value; DNPR, Danish National Patient Registry; TP, true positive; FP, false positive; FN, false negative, TN; true negative.
Among the six misclassified patients, one patient was transferred from another department during the course of the acute disease, which might explain the misclassification as a nonacute patient. No obvious explanations for the registration error of the remaining five misclassified patients could be found. The median age was 71 years for the misclassified acute patients (ie, patients with a nonacute admission in the DNPR confirmed to be acute admissions through the medical record review) compared with a median age of 62 years of the correctly classified acute patients. All of the misclassified acute patients were women. The characteristics of the misclassified nonacute patients (ie, patients with an acute admission in the DNPR confirmed to be nonacute admissions through the medical record review) were not different from those of the correctly classified patients. A sensitivity analysis comparing referral date and admission date registered in the DNPR confirmed the results from the review of the medical records except in one patient. This one patient was registered with an acute admission in the DNPR, but the medical record review showed that the patient had a scheduled admission. In the sensitivity analysis, the referral date was the same as the admission date, which confirmed the acute admission.
Discussion
In this validation study, we found a high PPV, sensitivity, and specificity of the registration of acute medical admissions in the DNPR. The variable for acute admissions is widely used, but to our knowledge no validation studies have previously been published. Our study has several strengths, including the use of the large and virtually complete registry, the DNPR, which allows individual-level linkage to other databases.10–12 In addition, we were able to ascertain both sensitivity and specificity, because our sample of medical inpatients included both acute and nonacute admissions, and the sample size was sufficient to provide reasonable precision of the estimates.
Our study does, however, also have limitations. First, the medical record reviewer was not blinded to the admission type registered in the DNPR, which might have led to results that were more concordant than they truly are. Second, a medical record is not perfect or uniform. Nonetheless, consistency in phrasing was high regarding admission type since the admission type and reason for admission were often stated in the first sentence of the admission note. Third, no time trend in the reporting of acute and nonacute admissions is considered, as we only included data from 1 year. However, our results are quite similar to the findings in the previous report from 2004, which might indicate no major changes in the intervening 5-year period. Fourth, we included data from only one region in Denmark. This might limit generalizability to other regions or counties, although the region includes 15 different medical departments, which are likely representative of other medical departments in the country. All 15 medical departments received direct referrals from general practitioners.
Despite these limitations, our findings were confirmed by a sensitivity analysis showing that virtually all acute patients were admitted the same day as they were referred to hospital, and that all nonacute patients had a referral date prior to the admission date.
Our results are comparable to the previous results in terms of the correct classification of acute admissions in 97% and 98.6% of cases.5,6 The latest validation of administrative data dates back to 2004 and includes only data from surgical and gynecology departments.6 The first report from 1990 included data on medical patients, but the results are reported in an overall analysis and missing data on admission type are considered correctly classified, which may cause an overestimation of the data quality.5
The results of the present study show that the admission type registered in the DNPR is valid. Our study has important perspectives for future studies of acute medical admissions based on the DNPR.
Conclusion
In conclusion, we found that the registration of acute admission among medical patients in the DNPR has a high validity.
Acknowledgments
This study was made possible with the invaluable help from the secretaries at the medical departments. Especially, we would like to thank Elisabeth V Kristoffersen for her help with retrieving and organizing the medical records.
Financial support: The study was supported by the Clinical Epidemiological Research Foundation, Denmark, and Aarhus University.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Statistics Denmark Welcome to StatBank Denmark [webpage on the Internet] Copenhagen, Denmark: Statistics Denmark; 2012Available from: http://statistikbanken.dk/statbank5a/selecttable/omrade0.asp?PLanguage=0Accessed November 27, 2012 [Google Scholar]
- 2.Jayaprakash N, O’Sullivan R, Bey T, Ahmed SS, Lotfipour S. Crowding and delivery of healthcare in emergency departments: the European perspective. West J Emerg Med. 2009;10(4):233–239. [PMC free article] [PubMed] [Google Scholar]
- 3.Lowthian JA, Curtis AJ, Jolley DJ, Stoelwinder JU, McNeil JJ, Cameron PA. Demand at the emergency department front door: 10-year trends in presentations. Med J Aust. 2012;196:128–132. doi: 10.5694/mja11.10955. [DOI] [PubMed] [Google Scholar]
- 4.Xu KT, Nelson BK, Berk S. The changing profile of patients who used emergency department services in the United States: 1996 to 2005. Ann Emerg Med. 2009;54(6):805–810. e1–e7. doi: 10.1016/j.annemergmed.2009.08.004. [DOI] [PubMed] [Google Scholar]
- 5.The National Board of Health Evaluering af Landspatientregistret 1990. [Evaluation of the Danish National Patient Registry 1990] National Board of Health; Copenhagen, Denmark: 1993Available from: http://www.ssi.dk/Sundhedsdataogit/Registre/Landspatientregisteret/Kvalitet%20i%20landspatientregisteret/~/media/Indhold/DK%20-%20dansk/Sundhedsdata%20og%20it/NSF/Registre/Landspatientregisteret/Evaluering%20af%20landspatientregisteret.ashxAccessed December 10, 2012Danish [Google Scholar]
- 6.The National Board of Health Projekt Vedrørende Datakvalitet I Landspatientregistret. [Project for Data Quality in the Danish National Patient Registry] 2004Available from: http://www.ssi.dk/~/media/Indhold/DK%20-%20dansk/Sundhedsdata%20og%20it/NSF/Registre/Landspatientregisteret/Rapport.ashxPublished 2004Accessed December 10, 2012Danish
- 7.Andersen TF, Madsen M, Jørgensen J, Mellemkjoer L, Olsen JH. The Danish National Hospital Register. A valuable source of data for modern health sciences. Dan Med Bull. 1999;46(3):263–268. [PubMed] [Google Scholar]
- 8.Weiss NS. Clinical epidemiology. In: Rothman KJ, Greenland S, Lash TL, editors. Modern Epidemiology. 3rd ed. Philadelphia, PA: Wolters Kluwer; 2008. pp. 642–646. [Google Scholar]
- 9.Brown LD, Cai TT, DasGupta A. Interval estimation for a binomial proportion. Statistical Science. 2001;16(2):101–133. [Google Scholar]
- 10.Lynge E, Sandegaard JL, Rebolj M. The Danish National Patient Register. Scand J Public Health. 2011;39(Suppl 7):30–33. doi: 10.1177/1403494811401482. [DOI] [PubMed] [Google Scholar]
- 11.Nickelsen TN. Data validity and coverage in the Danish National Health Registry. A literature review. Ugeskr Laeger. 2001;164(1):33–37. [PubMed] [Google Scholar]
- 12.Sorensen HT, Sabroe S, Olsen J. A framework for evaluation of secondary data sources for epidemiological research. Int J Epidemiol. 1996;25(2):435–442. doi: 10.1093/ije/25.2.435. [DOI] [PubMed] [Google Scholar]


