Abstract
Objective
Since existing numeracy measures may not optimally assess ‘health numeracy’, we developed and validated the General Health Numeracy Test (GHNT).
Methods
An iterative pilot testing process produced 21 GHNT items that were administered to 205 patients along with validated measures of health literacy, objective numeracy, subjective numeracy, and medication understanding and medication adherence. We assessed the GHNT’s internal consistency reliability, construct validity, and explored its predictive validity.
Results
On average, participants were 55.0±13.8 years old, 64.9% female, 29.8% non-White, and 51.7% had incomes ≤$39K with 14.4±2.9 years of education. Psychometric testing produced a 6-item version (GHNT-6). The GHNT-21 and GHNT-6 had acceptable-good internal consistency reliability (KR-20 = 0.87 vs. 0.77, respectively). Both versions were positively associated with income, education, health literacy, objective numeracy, and subjective numeracy (all p<.001). Furthermore, both versions were associated with participants’ understanding of their medications and medication adherence in unadjusted analyses, but only the GHNT-21 was associated with medication understanding in adjusted analyses.
Conclusions
The GHNT-21 and GHNT-6 are reliable and valid tools for assessing health numeracy.
Practice implications
Brief, reliable, and valid assessments of health numeracy can assess a patient’s numeracy status, and may ultimately help providers and educators tailor education to patients.
Keywords: general health numeracy test, validation, measurement, numeracy, health literacy, medication understanding, medication adherence
1. Introduction
Literacy includes a host of skills including print literacy, oral literacy, and quantitative (numeracy) skills. Numeracy is an important component of literacy, and reflects one’s ability to understand and use numbers in daily life [1]. A growing body of evidence suggests individuals with limited literacy or numeracy skills are less likely to receive preventive health care services [2, 3], and are more likely to experience difficulty following medical instructions [4, 5] understanding health information [6], performing self-care activities [7, 8], and to have worse health outcomes [1, 9] compared to individuals with adequate literacy or numeracy skills. For example, among individuals with diabetes, those with limited numeracy skills report worse diabetes knowledge and self-management behaviors, and have worse glycemic control compared to individuals with adequate numeracy skills [10]. Finally, while literacy and numeracy are strongly correlated, some individuals may have adequate literacy but inadequate numeracy skills [4, 6], and there are instances when numeracy, but not literacy, has been related to outcomes [10–12].
Most studies addressing literacy in health care use the term health literacy to refer to “one’s ability to understand and act on health information” [13] and include health literacy-specific measures, some of which are brief and could be administered in clinical care [14–16]. In contrast, some numeracy assessments used in research have limited application to health care decision making, or are lengthy mathematical tests that cannot be feasibly administered in clinical care [17, 18]. Furthermore, there are a few health-related numeracy measures available, but these measures either assess a narrow range of mathematical skills [19, 20] or are disease-specific [21, 22], which limits our understanding of the cross-situational and cross-conditional impact of limited ‘health numeracy’ on health outcomes. Thus, new measures to better estimate ‘health numeracy’ or “one’s understanding and capacity to act on numerical health information” are needed [1].
Provision of preventative, diagnostic, and therapeutic recommendations to patients often includes understanding and use of applied quantitative skills such as executing a medication schedule, or dietary recommendations and understanding results of laboratory assessments. In addition, numeracy is fundamental for the delivery of patient-centered care where options in management, including potential risks and benefits of these choices may be discussed [23]. Identification of patient’s with lower health numeracy may be important to trigger targeted resources to ensure a valuable experience for both patients and providers. Of particular interest would be tools with application in a variety of health care contexts that are brief, well-received by patients, and have practical, clinical and scientific utility for providers and researchers.
Our study objective was to develop an assessment of health numeracy, referred to as the General Health Numeracy Test (GHNT) and evaluate its psychometric properties, including internal consistency reliability and construct validity. Given recent evidence suggesting numeracy skills are strongly associated with one’s capacity to manage medications, and even explain gender and racial disparities on this outcome [24, 25], we also explored the GHNT’s predictive validity with patient’s understanding of their medications and medication adherence.
2. Methods
2.1 Sample
From June 2009 to August 2010, trained research assistants (RAs) enrolled 205 primary care outpatients at the Vanderbilt Adult Primary Care Clinic in Nashville, TN. Eligible patients were between the ages of 18–80 years and English-speaking. RAs used the Rosenbaum Pocket screener [26] to assess visual acuity, and excluded patients whose visual acuity was worse than 20/50. Patients were also excluded if they were too ill to participate, or had a clinical diagnosis of blindness, dementia and/or psychosis.
2.2 Data and procedure
Trained RAs recruited eligible patients, consented patients who were interested in participation, and conducted individual, in-person interviews to collect demographic information, administer validated measures of health literacy, objective numeracy, subjective numeracy, medication understanding, and medication adherence, and administer the newly developed GHNT. In an effort to minimize the impact of patients’ health literacy status on their numeracy skills, RAs first verbally administered the Rapid Estimate of Adult Learning in Medicine (REALM) and if a patient scored ≤44 on this instrument (i.e., they were categorized as having low health literacy) the remaining measures were verbally administered. Otherwise, RAs offered patients the option of verbal administration or self-administration. All interviews were conducted in a private room immediately prior to or after a patient’s scheduled medical appointment.
2.2.1 Demographics
Self-reported socio-demographic information included patient age, gender, race, income, years of education, and health insurance status.
2.2.3 Health literacy
The REALM is a valid and reliable measure of health literacy [27–29]. Respondents are asked to read aloud 66 health-related words arranged in order of increasing difficulty [27]. The score assigns health literacy skills into four categories of grade-equivalent reading level. Correct pronunciation of 0–44 words represents a 6th grade reading level or below (low literacy), 45–60 words represents a 7th-8th grade reading level (marginal literacy), and 61–66 words represents a 9th grade reading level (adequate literacy).
2.2.4 Objective numeracy
The arithmetic section of the Wide Range Achievement Test, 3rd Edition (WRAT-3) is a validated instrument that evaluates the ability to compute solutions to math problems [17]. Part I requires counting, reading number symbols, and solving simple arithmetic problems that are verbally presented to the examinee. Part II consists of using paper and a pencil to calculate up to 40 arithmetic problems within 15 minutes. Points (1 for each correct answer) are summed across Parts I and II, combined into a single raw score, and then standardized by age.
2.2.5 Subjective numeracy
The Subjective Numeracy Scale (SNS) is a valid and reliable self-report measure of one’s perceived ability to perform various mathematical tasks and one’s preference for using numerical versus prose information [20, 30]. This 8-item scale requires no mathematical calculations. Instead, it consists of 4 items asking respondents to assess their numerical ability in different contexts and 4 items asking respondents to state their preference for the presentation of numerical and probabilistic information.
2.2.6 Medication understanding
The Medication Understanding Questionnaire (MUQ) is a valid and reliable measure of one’s knowledge of the purpose, dose, and frequency of the medication(s) in his regimen [31]. To administer the MUQ, RAs access a patient’s medication list from the medical record and use a random numbers table to select up to 5 prescription medications from this list. If a patient is taking ≤5 medications, all eligible medications are selected. In our study, eligible medications were those taking taken every day, excluding medications that were taken ‘as needed,’ were considered combination therapies, or were classified as lotions/creams, nasal sprays, eye drops, herbals, supplements, or vitamins. The RA provides the brand and generic name of medication, and then asks the patient for the medication’s purpose, strength per unit (e.g., 20 mg tablet), number of units taken at a time (e.g., 2 tablets), and dosing frequency (e.g., twice a day). Patients are instructed not to refer to their medication list or bottles when responding. Each medication is scored from 0–3, reflecting the medication’s indication (1 point), strength (0.5 point), units (0.5 point), and frequency (1 point). While a patient’s overall MUQ score is the average of the scores for each tested medication, we converted these scores to percent correct to be consistent with our measure of medication adherence.
2.2.7 Medication adherence
The Summary of Diabetes Self-Care Activities (SDSCA) medication adherence subscales (i.e., the 1 item and 2 item versions) are valid and reliable measures of self-reported medication adherence, and individual items have correlated with objective measures of medication adherence (e.g., medication possession ratio) [32]. We used a single item modified to make it applicable to patients without diabetes and thus any drug indication. In the current study, we presented patients with each medication in their regimen for up to 5 randomly selected, eligible medications. If a patient is taking ≤5 medications, all eligible medications are selected. In our study, eligible medications were those taking taken every day, excluding medications that were taken ‘as needed,’ were considered combination therapies, or were classified as lotions/creams, nasal sprays, eye drops, herbals, supplements, or vitamins. We then asked the patient, “Please tell me how many days in the last week you took your (insert one medication name).” We then calculated each patient’s percent adherence score (i.e., [(number of medications queried up to 5)(7 days)−(total days any medication was missed)] ÷ [(number of medications queried up to 5)(7 days)] = % adherence) [33]. This was treated as a non-parametric continuous variable [32, 34] and also categorized as adherent (100%) [32, 35, 36] or not (< 100%).
2.2.8 General health numeracy test
Six experts in health literacy, numeracy, health psychology, scale development, and clinical medicine developed a novel set of 63 health numeracy items after reviewing previously developed assessment tools. These items assessed a wide range of numerical skills often used in the context of making health decisions; for example, understanding number hierarchy, performing calculations and correctly estimating probability when making decisions about disease prevention, nutrition management, medication adherence, and assessing one’s risk of a negative health outcome. The expert panel reviewed all items, omitting those items assessing the same numerical skill with the same level of difficulty. This resulted in a set of 44 items that were divided into 4 forms with 11 items per form. We administered each form to 6 patients (n = 24), and performed cognitive interviews with these patients to further identify those items assessing the same numerical skill with the same level of difficulty. Findings allowed us to reduce the set to 33 items. We then performed a second round of testing, administering all 33 items to a sample of patients (n = 35) and using a combination of cognitive interviews with these patients and expert panel review to further reduce the set to 21 items (GHNT-21). During each iterative, pilot testing phase, we omitted items that were unclear to patients, too difficult to answer, or were redundant with other items, while purposefully retaining items that covered a broad range of numerical skills described above.
2.3 Data analyses
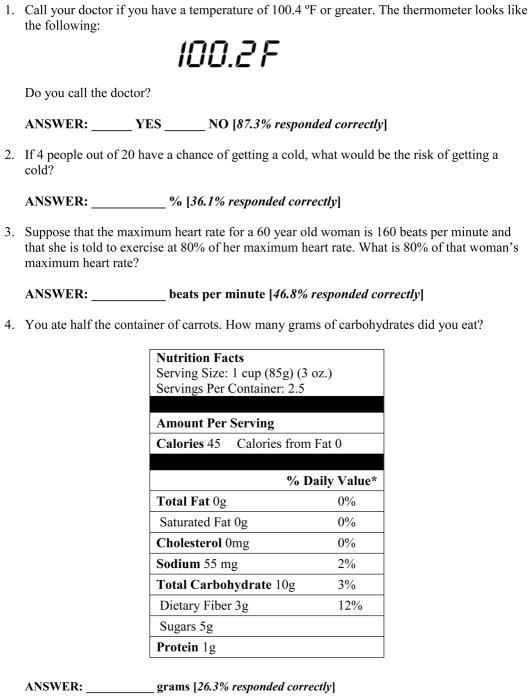
All analyses were performed using SPSS version 21.0. In an effort to further reduce the number of items on the GHNT-21, we first performed multiple rounds of psychometric testing (i.e., calculating internal consistency reliabilities if items were deleted and subsequent test of construct validity and predictive validity). These analyses resulted in a 6-item version of the GHNT (GHNT-6) shown in Figure 1.
Figure 1.
The 6-item General Health Numeracy Test (GHNT-6)
The Kuder-Richardson (KR-20) coefficient was used to examine the GHNT-21’s and GHNT-6’s internal consistency reliabilities. Values range from 0–1, with a higher KR-20 (e.g., >0.90) indicating a homogenous test.
A series of Spearman’s rho correlation coefficients tested our a priori hypothetical model for construct validity. This model predicted that health numeracy measured with the GHNT-21 or GHNT-6 would be positively associated with patients’ income, years of education, health literacy, objective numeracy, and subjective numeracy.
To explore the GHNT-21’s and GHNT-6’s predictive validity, we postulated that higher GHNT scores would correspond with greater medication understanding and medication adherence. To test these hypothesis, we performed a series of multivariate linear regression models to test the unadjusted and adjusted relationships between the GHNT-21 or the GHNT-6 and medication understanding and medication adherence as continuous variables. We then performed multivariate logistic regression models to test the unadjusted and adjusted relationship between the GHNT-21 or the GHNT-6 and medication adherence as a dichotomized variable (i.e., coded as 0 = perfect adherence and 1 = less than perfect adherence). In all adjusted models, we adjusted for age, gender, racial status, and income. We did not adjust for education, insurance status, or employment status due to these variables being collinear with numeracy.
3. Results
3.1 Sample characteristics
Sample characteristics are presented in Table 1. On average, participants (N = 205) were 55 years old (SD = 13.8 years), 64.9% were female, 29.8% were non-White, and 69.8% reported having private health insurance. Sixty-seven percent reported at least some college education, while 51.7% reported a total annual household income ≤39K. Eighteen percent of the sample had <9th grade reading level (or limited health literacy skills) according to the REALM, but 61.8% of the sample had <9th grade numeracy skills according to the WRAT-3. Finally, on average, participants understood their medication regimen 81.7% of the time and were adherent to their regimen 90.7% of the time (i.e., medication adherence as a continuous variable), with 67.5% of the sample reporting perfect adherence (i.e., medication adherence as a categorical variable, 100% adherence vs. < 100% adherence).
Table 1.
Participant characteristics.
| N = 205 | M ± SD or n (%) |
|---|---|
| Age | 55.0 ± 13.8 |
| Gender | |
| Female | 133 (64.9) |
| Race | |
| Caucasian/White | 144 (70.2) |
| African American/Black | 53 (25.8) |
| Other | 7 (4.0) |
| Education, years | 14.4 ± 2.9 |
| < High School | 13 (6.4) |
| High School | 54 (26.6) |
| > High School | 136 (67.0) |
| Income | |
| ≤39K | 104 (51.7) |
| ≥40K | 97 (48.3) |
| Insurance status | |
| Public/None | 60 (29.3) |
| Private | 143 (69.8) |
| Self-reported Medical History, range 0–3 | 1.1 ± 0.9 |
| Diabetes Mellitus | 60 (29.4) |
| Hypertension | 133 (65.2) |
| Heart Disease | 43 (21.1) |
| Health Literacy (REALM) | |
| < 9th grade | 37 (18.0) |
| ≥9th grade | 168 (82.0) |
| Objective Numeracy (WRAT-3) | |
| < 9th grade | 126 (61.8) |
| ≥9th grade | 78 (38.2) |
| Subjective Numeracy (SNS), range 1–6 | 3.8 ± 1.2 |
| Medication Understanding (MUQ), % correct | 81.7 ± 17.4 |
| Medication Adherence (SDSCA), % adherent | 90.7 ± 20.5 |
| perfectly adherent | 133 (67.5) |
| not perfectly adherent | 64 (32.5) |
Notes: REALM = Rapid Estimate of Adult Learning in Medicine; WRAT-3= Wide Range Achievement Test, 3rd Edition; SNS = Subjective Numeracy Scale; MUQ = Medication Understanding Questionnaire; SDSCA = Summary of Diabetes Self-Care Activities.
3.2 Descriptive statistics, reliability, and construct validity
The mean percent correct score on the GHNT-21 was 56% (out of 100%) with a standard deviation of 23%, which was slightly higher than the neutral midpoint (50%). The distribution was near normal, with only a slight negative skew (skewness −0.19, SE of skewness 0.17) and slight platykurtic spread (kurtosis −0.74, SE of kurtosis 0.34). Internal consistency reliability was good according to the Kuder-Richardson coefficient (KR-20 = 0.87). As shown in Table 2, higher scores on the GHNT-21 were significantly associated with higher income, more years of education, higher health literacy scores, higher objective numeracy scores, and higher subjective numeracy scores (p < 0.001 for all comparisons).
Table 2.
Inter-correlations of study variables.
| Variables | GHNT-21 | GHNT-6 | Education | Income | REALM | WRAT-3 | SNS | MUQ | SDSCA |
|---|---|---|---|---|---|---|---|---|---|
| 1. GHNT-21 | 1.00 | ||||||||
| 2. GHNT-6 | 0.88*** | 1.00 | |||||||
| 3. Education | 0.45*** | 0.41*** | 1.00 | ||||||
| 4. Income | 0.34*** | 0.32*** | 0.39*** | 1.00 | |||||
| 5. REALM | 0.54*** | 0.45*** | 0.42*** | 0.31*** | 1.00 | ||||
| 6. WRAT-3 | 0.64*** | 0.65*** | 0.45*** | 0.23*** | 0.47*** | 1.00 | |||
| 7. SNS | 0.57*** | 0.58*** | 0.52*** | 0.33*** | 0.36*** | 0.60*** | 1.00 | ||
| 8. MUQ | 0.35*** | 0.25*** | 0.28*** | 0.15* | 0.36*** | 0.24*** | .08 | 1.00 | |
| 9. SDSCA | 0.18** | 0.16* | 0.04 | .08 | .12 | 0.14* | .07 | 0.22** | 1.00 |
Notes: Spearman’s rho assessed the inter-correlations of study variables located in the remaining cells. GHNT-21 = 21-item General Health Numeracy Test; GHNT-6 = 6-item General Health Numeracy Test; REALM = Rapid Estimate of Adult Learning in Medicine; WRAT-3= Wide Range Achievement Test, 3rd Edition; SNS = Subjective Numeracy Scale; MUQ = Medication Understanding Questionnaire; SDSCA = Summary of Diabetes Self-Care Activities (medication adherence subscale).
P<.001,
P<.01,
P<.05,
The mean percent correct score on the GHNT-6 (see Figure 1 for percent correct per item) was 42% (out of 100%) with a standard deviation of 30%, which was slightly lower than the neutral midpoint (50%). The distribution was near normal, with only a slight negative skew (skewness 0.43, SE of skewness 0.17) and slight platykurtic spread (kurtosis −1.01, SE of kurtosis 0.34). Internal consistency reliability was acceptable according to the Kuder-Richardson coefficient (KR-20 = 0.77). As shown in Table 2, higher scores on the 6-item GHNT were significantly associated with higher income, more years of education, higher health literacy scores, higher objective numeracy scores, and higher subjective numeracy scores (p < 0.001 for all comparisons).
3.3 Predictive validity
As shown in Table 3, higher scores on the GHNT-21 were significantly associated with medication understanding in both the unadjusted, F = 28.55, p < .001 (β = 0.36, p < .001), and adjusted models, F = 7.99, p < .001 (β = 0.29, p < .001). In unadjusted models, higher scores on the GHNT-21 were significantly associated with both medication adherence as a continuous variable, F = 5.42, p = .02 (β = 0.17, p = .02), and as a dichotomized variable (adherent vs. non-adherent; OR = 4.75, p = .02 [95% CI: 1.28–17.69]). However, in adjusted models, scores on the GHNT-21 were not associated with medication adherence as a continuous variable, F = 3.37, p < .01 (β = .13, p = .18), or as a dichotomized variable (adherent vs. non-adherent; AOR = 1.82, p = .50 [95% CI: 0.32–10.36]).
Table 3.
Multivariate linear regression model with the 21-item and 6-item General Health Numeracy Tests (GHNT-21 and GHNT-6, respectively) predicting medication understanding.
| Predictor | GHNT-21 | GHNT-6 | ||||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Unstandardized coefficient
|
β | P-value | Unstandardized coefficient
|
β | P-value | |||
| B | SE | B | SE | |||||
| Model 1: Dependent Variable = medication understanding | ||||||||
| GHNT | 26.78 | 5.01 | 0.36 | .000 | 14.10 | 4.04 | 0.25 | .001 |
| Model 2: Dependent Variable = medication understanding | ||||||||
| GHNT | 21.16 | 6.52 | 0.29 | .001 | 8.98 | 4.63 | 0.16 | .054 |
| Age | −0.22 | 0.09 | −0.17 | .015 | −0.28 | 0.09 | −0.22 | .001 |
| Gender (Male vs. Female) | 4.84 | 2.47 | 0.13 | .052 | 5.44 | 2.53 | 0.15 | .033 |
| Race (Caucasian/White vs. African American/Black) | −2.28 | 3.23 | −0.06 | .481 | −5.42 | 3.06 | −0.14 | .078 |
| Income (≤39K vs. ≥40K) | 1.12 | 2.58 | 0.03 | .664 | 2.67 | 2.56 | 0.08 | .299 |
Notes: GHNT = General Health Numeracy Test; B = unstandardized coefficient; SE = standard error; β = standardized coefficient.
As shown in Table 3, higher scores on the GHNT-6 were significantly associated with medication understanding in both the unadjusted, F = 12.15, p < .001 (β = 0.25, p < .001), and adjusted models, F = 6.43, p < .001 (β = 0.16, p = .05). In unadjusted models, higher scores on the GHNT-6 were marginally associated with medication adherence as a continuous variable, F = 3.58, p = .06 (β = 0.14, p = .06), and as a dichotomized variable (adherent vs. non-adherent; OR = 2.54, p = .08 [95% CI: 0.90–7.18]). However, in adjusted models, scores on the GHNT-6 were not associated with medication adherence as a continuous variable, F = 3.14, p < .01 (β = 0.07, p = .38), or as a dichotomized variable (adherent vs. non-adherent; AOR = 1.23, p = .74 [95% CI: 0.36–4.27]).
4. Discussion and Conclusion
4.1 Discussion
The GHNT-21 and GHNT-6 are reliable and valid measures of health numeracy. The GHNT-21 demonstrated better internal consistency reliability than the GHNT-6, but both measures were significantly associated with measures used to test for construct validity. While both measures were also associated with medication understanding and medication adherence, the 21-item version had better predictive validity with medication understanding and adherence than the 6-item version. However, the 6-item version may require less time and participant response burden, and thus may be an appropriate tool for identifying patients with limited health numeracy.
Our sample reported high rates of poor numeracy skills. While <20% of the sample had limited health literacy skills according to the REALM, approximately two thirds had limited numeracy skills according to the WRAT-3, and the average percent correct on the GHNT-21 and GHNT-6 were 56% and 42% (both out of 100%), respectively. On the GHNT-6, participants were more likely to answer correctly to questions requiring fewer calculations or an understanding of number hierarchy, and were least likely to respond correctly to questions requiring more calculations or an understanding of risk and probability. For example, only 26.3% of the sample could correctly calculate the number of carbohydrates on the Nutrition Facts label, and only 21.0% could correctly calculate the risk of having a heart attack in five years if taking cholesterol-lowering medications that reduces this risk by a certain amount.
In adjusted analyses, the GHNT-21 was associated with patients’ understanding of their medication regimen. Successful adherence to medications not only relies on the frequency of medication-taking across time, but also on accurate understanding and management of prescription instructions. This includes correct identification of pills, understanding the number of pills to be taken at each dose, the timing of doses, determination of missed doses, need for refills and comprehension of warnings and other ancillary instructions (e.g., “take on an empty stomach”) [37]. Widely used measures of health literacy have been consistently associated with both understanding one’s medication regimen [7, 31, 38] and medication adherence [16, 39–42]. However, no studies to our knowledge have explored the relationship between numeracy and patients’ understanding of their own medication regimen, and only one study has found support for a relationship between objective numeracy measured with a non-health-related assessment and medication management capacity [24, 25].
We recently tested the relationship between disease-specific numeracy (measured with the Diabetes Numeracy Test [21]) and medication adherence, and objective numeracy (measured with the WRAT-3 [18]) and medication adherence, and found no associations [39]. In contrast, the current study explored the relationship between numeracy measured with the new GHNT-21 or GHNT-6 and medication understanding and medication adherence, and found support for ‘health numeracy’ being associated with medication understanding and weaker support ‘health numeracy’ being associated with medication adherence, with both providing initial evidence of the GHNT’s predictive validity. Future research should continue to explore these relationships using multiple measures of medication understanding and adherence, and larger samples that are homogenous with respect to medical condition and drug indication.
There are study limitations to acknowledge. First, we assessed medication adherence via a single, self-report measure rather than more objective measures of adherence (e.g., pill counts, prescription refills, and electronic monitoring devices). While patients may under-report missed doses through questionnaires, a handful of studies suggest self-report measures are viable and accurate measures of medication adherence [43, 44].
Secondly, we do not know the administration time of the GHNT-6 since we administered the GHNT-21 in our main study. However, based on our experience administering numeracy instruments, we estimate this time to be approximately 5–8 minutes. The GHNT also focuses on computational skills and “verbatim” responses rather than on patients’ “number sense.” Reyna [45] has suggested that many patients understand numbers and make mathematical inferences based more on “gist” or “number sense” than on exact computations (or what Reyna refers to as “verbatim” representations of information). While there is often a correlation between a patient’s computational skill (and “verbatim” responses) and their “number sense,” there may be patients with good number sense, but poor computational skills and patients with good computational skills, but poor number sense. In addition, whether or not a patient can perform a set of computations to 100% accuracy may not be relevant to the task being tested or the communication being interpreted--as long as they have understood the “gist” of the situation and make appropriate actions in response.
Finally, our study sample was also small, predominately Caucasian/White race of higher socioeconomic status and from a single academic medical center. Thus, the findings may not generalize to low income, racially/ethnically diverse patient populations and/or those receiving care at non-academic facilities. Furthermore, as primary care patients, this sample was heterogeneous with respect to the number and type of medical conditions they had, the number of medications they were taking, and the indication of these drugs, potentially limiting our ability to detect a statistically significant association between the GHNT-6 and medication understanding and medication adherence in our adjusted analyses. Despite these limitations, our study is the first to report the psychometric properties and predictive validity of a measure of ‘health numeracy’ that represents a range of health topics.
4.2. Conclusion
While our findings suggest the GHNT-21 and GHNT-6 are valid and reliable measures of ‘health numeracy’, additional predictive validity evidence is needed to ascertain if the 6-item version is as robust as the 21-item version for research purposes. In general, future research should provide additional psychometric support as well as evidence of the utility of both instruments in intervention research and clinical care. Such evaluation might include establishing test-retest reliability, discriminant validity, scoring cutoffs to categorize individuals with limited versus adequate health numeracy, and providing evidence of the GHNT-21’s and GHNT-6’s predictive validity with a wide range of social-cognitive, behavioral, and physiological health outcomes. Finally, additional support for the instruments’ association with medication understanding and medication adherence along with evidence of the instruments’ sensitivity would allow for determining whether the GHNT is an applicable evaluative tool for interventions promoting these outcomes.
4.3 Practice implications
Our findings demonstrate that a relatively brief tool can assess a patient’s health numeracy status and highlight the importance of understanding how a patient’s numeracy might impact their understanding of issues related to their health care and self-management, such as understanding a medication regimen and adhering to it. Recent studies suggest there may be opportunities to improve how providers communicate to patients with low health numeracy about taking care of their health, especially about self-management behaviors requiring numeracy skills (e.g., correct timing and dosing of medications) [46, 47]. However, in order to be effective, we must first develop, test, and incorporate brief, reliable, and valid assessments of health numeracy [1]. Such measures may ultimately help health care providers and educators tailor educational messages to a patients’ level of understanding, with the goal of improving patient self-management behaviors and health outcomes.
Supplementary Material
Acknowledgments
Dr. Osborn is supported by NIDDK K01DK087894. Dr. Cavanaugh is supported by NIDDK K23DK80952.
Footnotes
Conflict of interest: Dr Kripalani is a consultant to and holds equity in PictureRx, LLC, which makes patient education tools to improve medication management. PictureRx did not provide materials or funding for this study.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Rothman RL, Montori VM, Cherrington A, Pignone MP. Perspective: the role of numeracy in health care. J Health Commun. 2008;13:583–95. doi: 10.1080/10810730802281791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ciampa PJ, Osborn CY, Peterson NB, Rothman RL. Patient numeracy, perceptions of provider communication, and colorectal cancer screening utilization. J Health Commun. 2010;15 (Suppl 3):157–68. doi: 10.1080/10810730.2010.522699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sudore RL, Mehta KM, Simonsick EM, Harris TB, Newman AB, Satterfield S, et al. Limited literacy in older people and disparities in health and healthcare access. J Am Geriatr Soc. 2006;54:770–6. doi: 10.1111/j.1532-5415.2006.00691.x. [DOI] [PubMed] [Google Scholar]
- 4.Kumar D, Sanders L, Perrin EM, Lokker N, Patterson B, Gunn V, et al. Parental understanding of infant health information: health literacy, numeracy, and the Parental Health Literacy Activities Test (PHLAT) Acad Pediatr. 2010;10:309–16. doi: 10.1016/j.acap.2010.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lindquist LA, Go L, Fleisher J, Jain N, Friesema E, Baker DW. Relationship of health literacy to intentional and unintentional non-adherence of hospital discharge medications. J Gen Intern Med. 2011 doi: 10.1007/s11606-011-1886-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rothman RL, Housam R, Weiss H, Davis D, Gregory R, Gebretsadik T, et al. Patient understanding of food labels: the role of literacy and numeracy. Am J Prev Med. 2006;31:391–8. doi: 10.1016/j.amepre.2006.07.025. [DOI] [PubMed] [Google Scholar]
- 7.Kripalani S, Henderson LE, Chiu EY, Robertson R, Kolm P, Jacobson TA. Predictors of medication self-management skill in a low-literacy population. J Gen Intern Med. 2006;21:852–6. doi: 10.1111/j.1525-1497.2006.00536.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Huizinga MM, Carlisle AJ, Cavanaugh KL, Davis DL, Gregory RP, Schlundt DG, et al. Literacy, numeracy, and portion-size estimation skills. Am J Prev Med. 2009;36:324–8. doi: 10.1016/j.amepre.2008.11.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wolf MS, Gazmararian JA, Baker DW. Health literacy and functional health status among older adults. Archives of internal medicine. 2005;165:1946–52. doi: 10.1001/archinte.165.17.1946. [DOI] [PubMed] [Google Scholar]
- 10.Cavanaugh K, Huizinga MM, Wallston KA, Gebretsadik T, Shintani A, Davis D, et al. Association of numeracy and diabetes control. Ann Intern Med. 2008;148:737–46. doi: 10.7326/0003-4819-148-10-200805200-00006. [DOI] [PubMed] [Google Scholar]
- 11.Huizinga MM, Beech BM, Cavanaugh KL, Elasy TA, Rothman RL. Low numeracy skills are associated with higher BMI. Obesity (Silver Spring) 2008;16:1966–8. doi: 10.1038/oby.2008.294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lokker N, Sanders L, Perrin EM, Kumar D, Finkle J, Franco V, et al. Parental misinterpretations of over-the-counter pediatric cough and cold medication labels. Pediatrics. 2009;123:1464–71. doi: 10.1542/peds.2008-0854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nielsen-Bohlman L, Panzer A, Kindig DA, editors. IOM. Health Literacy: A Prescription to End Confusion. Washington, DC: 2004. [PubMed] [Google Scholar]
- 14.Chew LD, Bradley KA, Boyko EJ. Brief questions to identify patients with inadequate health literacy. Fam Med. 2004;36:588–94. [PubMed] [Google Scholar]
- 15.Morris NS, MacLean CD, Chew LD, Littenberg B. The Single Item Literacy Screener: evaluation of a brief instrument to identify limited reading ability. BMC Fam Pract. 2006;7:21. doi: 10.1186/1471-2296-7-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Osborn CY, Davis TC, Bailey SC, Wolf MS. Health literacy in the context of HIV treatment: introducing the Brief Estimate of Health Knowledge and Action (BEHKA)-HIV version. AIDS Behav. 2010;14:181–8. doi: 10.1007/s10461-008-9484-z. [DOI] [PubMed] [Google Scholar]
- 17.Wilkinson GS. WRAT3: Wide Range Achievement Test Administration Manual. Wilmington, DE: Wide Range, Inc; 1993. [Google Scholar]
- 18.Woodcock R, McGrew K, Mather N, Woodcock Johnson . Tests of Achievement. Itasca, IL: Riverside Publishing; 2001. [Google Scholar]
- 19.Lipkus IM, Samsa G, Rimer BK. General performance on a numeracy scale among highly educated samples. Med Decis Making. 2001;21:37–44. doi: 10.1177/0272989X0102100105. [DOI] [PubMed] [Google Scholar]
- 20.Zikmund-Fisher BJ, Smith DM, Ubel PA, Fagerlin A. Validation of the Subjective Numeracy Scale: effects of low numeracy on comprehension of risk communications and utility elicitations. Med Decis Making. 2007;27:663–71. doi: 10.1177/0272989X07303824. [DOI] [PubMed] [Google Scholar]
- 21.Huizinga MM, Elasy TA, Wallston KA, Cavanaugh K, Davis D, Gregory RP, et al. Development and validation of the Diabetes Numeracy Test (DNT) BMC Health Serv Res. 2008;8:96. doi: 10.1186/1472-6963-8-96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Apter AJ, Cheng J, Small D, Bennett IM, Albert C, Fein DG, et al. Asthma numeracy skill and health literacy. J Asthma. 2006;43:705–10. doi: 10.1080/02770900600925585. [DOI] [PubMed] [Google Scholar]
- 23.Committee on Quality of Health Care in America. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: Institute of Medicine; 2001. [Google Scholar]
- 24.Waldrop-Valverde D, Jones DL, Jayaweera D, Gonzalez P, Romero J, Ownby RL. Gender differences in medication management capacity in HIV infection: The role of health literacy and numeracy. AIDS and Behav. 2009;13:46–52. doi: 10.1007/s10461-008-9425-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Waldrop-Valverde D, Osborn CY, Rodriguez A, Rothman RL, Kumar M, Jones DL. Numeracy skills explain racial differences in HIV medication management. AIDS Behav. 2010;14:799–806. doi: 10.1007/s10461-009-9604-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rosenbaum J. Rosenbaum Vision Pocket Screener. Quincy, MA: Grass Instruments; 1982. [Google Scholar]
- 27.Davis TC, Long SW, Jackson RH, Mayeaux EJ, George RB, Murphy PW, et al. Rapid estimate of adult literacy in medicine: A shortened screening instrument. Fam Med. 1993;25:391–5. [PubMed] [Google Scholar]
- 28.Parker RM, Baker DW, Williams MV, Nurss JR. The test of functional health literacy in adults: a new instrument for measuring patients’ literacy skills. J Gen Intern Med. 1995;10:537–41. doi: 10.1007/BF02640361. [DOI] [PubMed] [Google Scholar]
- 29.Davis TC, Michielutte R, Askov EN, Williams MV, Weiss BD. Practical assessment of adult literacy in health care. Health Educ Behav. 1998;25:613–24. doi: 10.1177/109019819802500508. [DOI] [PubMed] [Google Scholar]
- 30.Fagerlin A, Zikmund-Fisher BJ, Ubel PA, Jankovic A, Derry HA, Smith DM. Measuring numeracy without a math test: development of the Subjective Numeracy Scale. Med Decis Making. 2007;27:672–80. doi: 10.1177/0272989X07304449. [DOI] [PubMed] [Google Scholar]
- 31.Marvanova M, Roumie CL, Eden SK, Cawthon C, Schnipper JL, Kripalani S. Health literacy and medication understanding among hospitalized adults. J Hosp Med. 2011;6:487. doi: 10.1002/jhm.998. [DOI] [PubMed] [Google Scholar]
- 32.Cohen HW, Shmukler C, Ullman R, Rivera CM, Walker EA. Measurements of medication adherence in diabetic patients with poorly controlled HbA(1c) Diabet Med. 2010;27:210–6. doi: 10.1111/j.1464-5491.2009.02898.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cohen MJ, Shaykevich S, Cawthon C, Kripalani S, Paasche-Orlow MK, Schnipper JL. Predictors of medication adherence postdischarge: The impact of patient age, insurance status, and prior adherence. J Hosp Med. 2012;7:470–5. doi: 10.1002/jhm.1940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Toobert DJ, Hampson SE, Glasgow RE. The summary of diabetes self-care activities measure: results from 7 studies and a revised scale. Diabetes Care. 2000;23:943–50. doi: 10.2337/diacare.23.7.943. [DOI] [PubMed] [Google Scholar]
- 35.Gonzalez JS, Safren SA, Cagliero E, Wexler DJ, Delahanty L, Wittenberg E, et al. Depression, self-care, and medication adherence in type 2 diabetes: relationships across the full range of symptom severity. Diabetes Care. 2007;30:2222–7. doi: 10.2337/dc07-0158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Gonzalez JS, Safren SA, Delahanty LM, Cagliero E, Wexler DJ, Meigs JB, et al. Symptoms of depression prospectively predict poorer self-care in patients with Type 2 diabetes. Diabet Med. 2008;25:1102–7. doi: 10.1111/j.1464-5491.2008.02535.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.MacLaughlin EJ, Raehl CL, Treadway AK, Sterling TL, Zoller DP, Bond CA. Assessing medication adherence in the elderly: which tools to use in clinical practice? Drugs Aging. 2005;22:231–55. doi: 10.2165/00002512-200522030-00005. [DOI] [PubMed] [Google Scholar]
- 38.Wolf MS, Davis TC, Shrank W, Rapp DN, Bass PF, Connor UM, et al. To err is human: patient misinterpretations of prescription drug label instructions. Patient Educ Couns. 2007;67:293–300. doi: 10.1016/j.pec.2007.03.024. [DOI] [PubMed] [Google Scholar]
- 39.Osborn CY, Cavanaugh K, Wallston KA, Kripalani S, Elasy TA, Rothman RL, et al. Health literacy explains racial disparities in diabetes medication adherence. J Health Commun. 2011;16 (Suppl 3):268–78. doi: 10.1080/10810730.2011.604388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kalichman SC, Pope H, White D, Cherry C, Amaral CM, Swetzes C, et al. Association between health literacy and HIV treatment adherence: further evidence from objectively measured medication adherence. J Int Assoc Physicians AIDS Care (Chic) 2008;7:317–23. doi: 10.1177/1545109708328130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kripalani S, Gatti ME, Jacobson TA. Association of age, health literacy, and medication management strategies with cardiovascular medication adherence. Patient Educ Couns. 2010;81:177–81. doi: 10.1016/j.pec.2010.04.030. [DOI] [PubMed] [Google Scholar]
- 42.Gazmararian JA, Kripalani S, Miller MJ, Echt KV, Ren J, Rask K. Factors associated with medication refill adherence in cardiovascular-related diseases: a focus on health literacy. J Gen Intern Med. 2006;21:1215–21. doi: 10.1111/j.1525-1497.2006.00591.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Gehi AK, Ali S, Na B, Whooley MA. Self-reported medication adherence and cardiovascular events in patients with stable coronary heart disease: the heart and soul study. Arch Intern Med. 2007;167:1798–803. doi: 10.1001/archinte.167.16.1798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Schroeder K, Fahey T, Hay AD, Montgomery A, Peters TJ. Adherence to antihypertensive medication assessed by self-report was associated with electronic monitoring compliance. J Clin Epidemiol. 2006;59:650–1. doi: 10.1016/j.jclinepi.2005.10.013. [DOI] [PubMed] [Google Scholar]
- 45.Reyna VF, Nelson WL, Han PK, Dieckmann NF. How numeracy influences risk comprehension and medical decision making. Psychological Bulletin. 2009;135:943–73. doi: 10.1037/a0017327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Cavanaugh K, Wallston KA, Gebretsadik T, Shintani A, Huizinga MM, Davis D, et al. Addressing literacy and numeracy to improve diabetes care: two randomized controlled trials. Diabetes Care. 2009;32:2149–55. doi: 10.2337/dc09-0563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Cavanaugh K, Davis D, Gregory RP, Wolff K, Rothman RL. Addressing the role of nutrition education and health literacy in diabetes care; American Association of Diabetes Educators Annual Meeting; San Antonio, TX. 2010. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.