Abstract
Oral cavity consists of a small vestibule and a larger oral cavity proper. A wide number of dermatological conditions can affect the oral cavity. The clinical characteristics of the same were studied in patients attending departments of Dermatology/ENT Himalayan Institute of Medical Sciences, Dehradun. To delineate and identify the various patterns of oral dermatological conditions in this part of the country. One hundred and fifty patients were included in the study having oral lesions irrespective of age, sex and duration. Clinical examination including cutaneous examination and simple investigations like routine blood, urine, stool, blood sugar, KOH mount and scraping, Tzanck test, and on certain cases biopsy were carried out. Out of 11,840 patients attending Dermatology/ENT OPD, HIMS, Dehradun from April 2008 to March 2009, 150 patients were having various disorders with oral manifestations. The incidence of oral cavity dermatoses in this study was 1.26%, male to female ratio was 2:3. (Out of 150 patients, 60 were males and 90 were females). Aphthous ulcer (28.57%) and pemphigus vulgaris (26.60%) formed the major bulk of patients followed by SLE (17.02%), oral candidiasis (16.07%), DLE (13.83%), lichen planus (12.77%) and others.
Keywords: Oral lesions, Oral cavity, Dermatological, Pemphigus vulgaris
Introduction
This is a study of dermatological conditions involving oral cavity which has been carried out in this part of the country to know the types of various dermatological conditions. There are very few such studies from the entire country and no such study has been carried out from this region.
Very often the oral dermatological conditions involving oral cavity are misdiagnosed and proper attention and care is not given. This study is an attempt to sensitize the clinicians to the prevailing situation of oral dermatological conditions of this region.
Anatomy of the Oral Cavity
Oral or Buccal cavity derives from both ectodermal and endodermal regions. Rima oris is the opening between lips and oral cavity. The oral cavity is divided into two parts, the vestibule and oral cavity proper. The oral cavity proper includes the lips, floor of mouth, labial and buccal mucosa, tongue, hard and soft palates, gingiva, and teeth. Oral cavity consists of a smaller vestibule outside the teeth and an inner larger oral cavity proper. Vestibule is a slit like space bounded externally by lips and cheeks and internally by gums and teeth. Oral cavity proper is bounded anterolaterally by alveolar arches, teeth and gums, behind it communicates with pharynx at the oropharyngeal isthmus, between the palatoglossal folds. Roof is formed by the hard and soft palates, most of its floor by anterior region of tongue and the rest by reflexion of mucosa from the sides and inferior surface to the gum or internal mandibular surface.
Materials and Methods
A total of 150 cases were taken up for the study who had oral lesions irrespective of age, sex and duration of the lesions attending departments of Dermatology/ENT, Himalayan Institute of Medical Sciences, Dehradun during 1 year period.
The patients after taking consent were subjected to thorough history and clinical examination including cutaneous examination to see if there were any cutaneous lesions and systemic components to come to a clinical diagnosis. While studying the oral lesion the following areas were taken into consideration like site of the lesion, morphology and extent of lesion, discharge if any, margins, floor, base and regional lymph nodes if any. The required investigations like routine blood, urine, stool, blood sugar, scrapings and KOH mount, Tzanck test, gram stains and on certain cases biopsy for histopathological examinations were carried out. Special tests were done for systemic diseases if indicated.
Observations
Incidence of oral cavity dermatoses was 1.26%. It was observed that out of total 11,840 patients attending Dermatology & ENT OPD, from April 2008 to March 2009, 150 patients were having various diseases with oral manifestations.
Table 1 shows that maximum incidence was between 1st and 3rd decade. It shows most of the patients were between 11 and 40 years of age. This table also shows that out of 150 patients, 60 (40%) were males and 90 (60%) were females. Male to Female ratio being 2:3.
Table 1.
Age distribution
| Age (in years) | Number of patients | Total | Percentage out of 150 cases | |
|---|---|---|---|---|
| Male | Female | |||
| 0–10 | 4 | 4 | 8 | 5.33 |
| 11–20 | 12 | 20 | 32 | 21.33 |
| 21–30 | 13 | 22 | 35 | 23.34 |
| 31–40 | 13 | 24 | 37 | 24.67 |
| 41–50 | 9 | 14 | 23 | 15.33 |
| > 50 | 9 | 6 | 15 | 10.00 |
| Total | 60 | 90 | 150 | 100.00 |
From Table 2 it is clear that, aphthous ulcers (RAS) constitute the major bulk of patients (28.57%), followed by oral candidiasis (16.07%) and angular stomatitis (10.71%).
Table 2.
Diseases with oral manifestations (n = 56)
| Diseases | No. of patients | % out of 56 |
|---|---|---|
| Aphthous ulcer | 16 | 28.57 |
| Oral candidiasis | 9 | 16.07 |
| Angular cheilitis | 6 | 10.71 |
| Oral leukoplakia | 4 | 7.14 |
| Fixed drug eruption | 4 | 7.14 |
| Squamous cell carcinoma | 3 | 5.36 |
| Fordyce spot | 2 | 3.57 |
| Herpes simplex stomatitis | 2 | 3.57 |
| Oral submucous fibrosis | 6 | 10.71 |
| Mucocele | 2 | 3.57 |
| Leukemia | 1 | 1.79 |
| Warts | 1 | 1.79 |
| Scrotal tongue | 1 | 1.79 |
It was found that among the patients with diseases with oral and cutaneous manifestations pemphigus vulgaris formed the major bulk of patients (26.60%), followed by SLE (17.02%), DLE (13.83%) and LP (12.77%).
Discussion
Patients having diseases affecting oral mucosa presents with different types of oral signs and symptoms, viz, oral pain, soreness and burning, xerostomia, bleeding, swelling, change of colour, ulcers, erosions, crusting and fissuring. In the present study, out of 11,840 patients attending Dermatology/ENT OPD, 150 were having oral cavity manifestation, incidence being 1.26%. The present study had 40% males and 60% females. The females outnumbered males in this study. Age specific attendance rates in Dermatology/ENT OPD are more common in female patients [1]. Out of 150 patients, maximum number of patients were between age range of 11–40 years (69.33%).
Our study recorded 25 patients (16.66%) of Pemphigus vulgaris having both oral and cutaneous manifestations. Our study revealed that Pemphigus vulgaris is the commonest oral involvement in this part of the country. In India reported incidence is highest in Assam, followed by Gujarat as observed by Huda et al. [2].
In this study Buccal mucosa was the most commonly affected site 68% followed by Palates (56%), lips (44%), tongue (40%) and labial mucosa (16%). Scully et al. [3] also found in their study, that buccal mucosa was commonly affected site (71%) followed by palatal (44%), lingual (42%) and labial mucosa (35%).
Collagen diseases form the next common group comprising 23.34%. Present study recorded 16 patients (17.02%) of Systemic Lupus Erythematosus, comprising 13 females and 3 males. Burge [4] in their study of 53 patients with SLE found 48 females and 5 males. Most of the lesions confined to Palate (87.5%) in our study, whereas SM Burge (1989) reported that lips and palate are the commonest site of involvement.
Present study recorded 13 patients (13.83%) of Discoid Lupus Erythematosus constituting 3 males and 13 females. Lips were the commonest site involved. Burge SM (1989) found 42 females and 26 males in their study group of 68 patients with DLE. Buccal mucosa was the commonest site affected.
Among the specific Cutaneous disorders, 16 patients of Recurrent Aphthous Stomatitis (RAS) have been recorded, labial mucosa was the commonest involved site. Commonest sites of occurrence of RAS are labial and buccal mucosa [5]. Most common type was minor type in this study.
Twelve patients (12.77%) of Lichen planus (LP) were recorded in this study. Five (41.66%) out of 12 were between the ages of 20–40 years. Singh et al. [6] observed that LP is most common in this age group in an Indian study. Two (16.67%) patients of LP aged below 15 years were recorded in this study. Sharma and Maheshwari [7] observed 30% of OLP in children. Handa and Sahoo [8] recorded 13.8% of OLP in children. Lip and Cheek were the commonest sites involved (9 patients). Erosive lesions were observed in 8 patients (66.67%), and reticular pattern in 4 patients (33.33%) in this study. Silvermann et al. [9] in their study of OLP documented erosive lesion in 22%, reticular in 7%.
Infective disorders constitute 10% cases in this study. Among the infective diseases candidiasis forms the major bulk (16.07%). Nine patients (16.07%) of oral candidiasis were recorded, and dorsal surface of tongue was the commonest site involved. Hay RJ [10] observed dorsal tongue as the commonest site of oral candidiasis. Out of 9 cases of oral candidiasis, 3 had Diabetes Mellitus, 2 were on prolonged antibiotic therapy and 4 patients had poor oral hygiene. Present study recorded 6 patients (10.71%) of oral submucous fibrosis (6 out of 56). All the patients had fibrosis on cheeks (buccal mucosa), one had lesions on lips and labial mucous membrane with trismus. All the patients were addicted to ghutka, panmasala and tobacco chewing. Oral submucous fibrosis is a very common condition in South East Asia including state of Uttarakhand. Pindborg et al. [11] found cheeks, lips and palate as a commonest site of fibrosis.
Four patients of leukoplakia have been recorded in this study which constitutes 7.14%. Two (50%) out of 4 patients were having age more than 50 years. Dorey et al. [12] found that leukoplakia is seen most frequently in persons 50–70 years of age and slight predilection for men. 1 out of 4 patients (25%) had associated oral candidiasis in this study. Roed Peterson et al. [13] found candidiasis (31%) in association with leukoplakia. All the patients were addicted to smoking in this study and buccal mucosa was the commonest site of involvement, all the 4 patients had lesions on buccal mucosa. Silverman et al. [14] estimated that approximately 91% of leukoplakic lesions occur in buccal mucosa and angles of mouth. 1 out of 4 patients had lesion on hard palate also. Mehta et al. [15] found hard palate as the commonest site of most leukoplakia (71%) in Andhra Pradesh, India.
In this study 6 patients of angular stomatitis have been recorded which constitutes 10.71%. Among 6 patients 3 were males and 3 females. All the patients had lesions on lips and labial mucosa. All had fissures at the angles of mouth and all had a habit of regular betel and areca nut chewing. Labial mucous membrane is involved in almost all cases of angular stomatitis [16]. In the present study 2 (33.33%) out of 6 patients had candida albicans as a co-infective agent demonstrated by KOH preparation. Ohman et al. [17] found that staphylococci and candida albicans are common infective agents in angular cheilitis.
Other Conditions Encountered with Oral Lesions
Fixed drug eruptions (7.14%), Squamous cell carcinoma (5.36%), Fordyce spot (3.57%), Herpes simplex Stomatitis (3.57%), Mucocele (3.57%), Leukemia (1 patient) -1.79%, Viral warts (1.79%), Scrotal tongue (1.79%), Steven Johnson Syndrome (8.51%), Toxic epidermal necrolysis (4.26%), Erythema Multiforme (1.06%), Systemic Sclerosis (6.38%), Vitiligo (6 6.38%).
Conclusion
Oral cavity can be affected by a variety of disorders and many systemic disorders have wide range of manifestations in the oral cavity or mucosa. Any symptom or sign in the oral cavity should not be neglected because that can be an early predictor of any underlying disease. In the present study Pemphigus vulgaris forms the major bulk of patients substantiating the fact that Pemphigus vulgaris is the commonest disease in this part of the country.
Oral mucous membrane alone may be involved but very often missed by Dermatologist, Dental and ENT surgeons, and physicians. This can be taken care of by the primary health care providers without going through much sophisticated investigations and further delay and for early appropriate interventions for the benefit of the patients (Table 3; Figs. 1, 2, 3 and 4).
Table 3.
Diseases with oral and cutaneous manifestations (n = 94)
| Diseases | No. of patients | % out of 94 |
|---|---|---|
| Pemphigus vulgaris | 25 | 26.60 |
| Pemphigus vegetans | 02 | 2.13 |
| Stevens Johnson syndrome | 08 | 8.51 |
| Toxic epidermal necrolysis | 04 | 4.26 |
| Erythema multiforme | 01 | 1.06 |
| Discoid lupus erythematosus | 13 | 13.83 |
| Systemic lupus erythematosus | 16 | 17.02 |
| Systemic sclerosis | 06 | 6.38 |
| Lichen planus | 12 | 12.77 |
| Vitiligo | 06 | 6.38 |
Fig. 1.

Pemphigus vulgaris (oral and cutaneous)
Fig. 2.

Aphthous ulcer
Fig. 3.
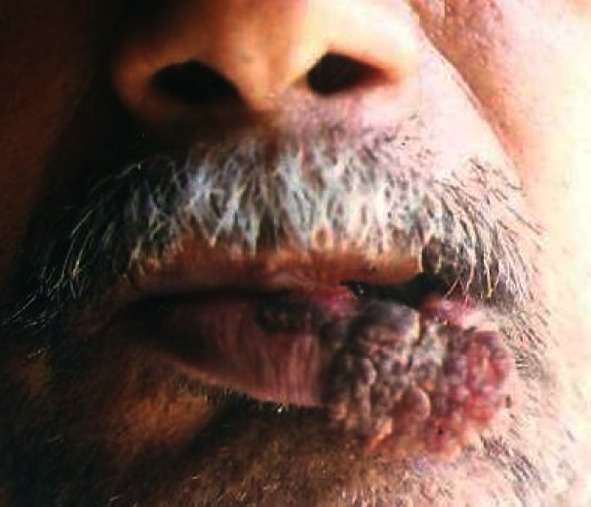
Squamous cell carcinoma (Lower lip)
Fig. 4.

Oral Candidiasis
Contributor Information
Samarjit Roy, Email: roy.samarjit@rediffmail.com.
Saurabh Varshney, Email: drsaurabh68@gmail.com.
References
- 1.Williams HC. Epidemiology of skin disease. In: Rook AJ, Wilkinson DS, Ebling FJG, editors. Text book of dermatology. 6. Oxford: Blackwell Scientific Oxford; 1998. pp. 139–157. [Google Scholar]
- 2.Huda MM, Afsar MI. A clinico pathological study of Pemphigus. Indian J Dermatol. 2001;46(2):75–79. [Google Scholar]
- 3.Scully C, De Paes Almeida O, Porter SR. Pemphigus vulgaris, the manifestations and long term management of 55 patients with oral lesions. British J Dermatol. 1999;140:84–89. doi: 10.1046/j.1365-2133.1999.02612.x. [DOI] [PubMed] [Google Scholar]
- 4.Burge SM, Frith PA, Juniper RP. Mucosal involvement in systemic and chronic cutaneous lupus erythematosus. Br J Dermatol. 1989;121:727–741. doi: 10.1111/j.1365-2133.1989.tb08215.x. [DOI] [PubMed] [Google Scholar]
- 5.GrayKowski EA, et al. Recurrent aphthous stomatitis, clinical, therapeutic, histopathological and hypersensitivity aspects. JAMA. 1966;196:637–644. doi: 10.1001/jama.1966.03100200077024. [DOI] [PubMed] [Google Scholar]
- 6.Singh OP, Kanwar AJ. Lichen planus in India. An appraisal of 441 cases. Int J Dermatol. 1976;15:752–756. doi: 10.1111/j.1365-4362.1976.tb00175.x. [DOI] [PubMed] [Google Scholar]
- 7.Sharma R, Maheswari V. Childhood lichen planus. A report of 50 cases. Pediatr Dermatol. 1999;16:345–348. doi: 10.1046/j.1525-1470.1999.00074.x. [DOI] [PubMed] [Google Scholar]
- 8.Handa S, Sahoo B. Childhood lichen planus. A study of 87 cases. Int J Dermatol. 2002;41:423–427. doi: 10.1046/j.1365-4362.2002.01522.x. [DOI] [PubMed] [Google Scholar]
- 9.Silverman SJ, Grosky M, Lozada Nur F, Gianottik A. A prospective study of findings and management in 214 patients with oral LP. Oral Surg Oral Med Oral Pathol. 1991;72:665–670. doi: 10.1016/0030-4220(91)90007-Y. [DOI] [PubMed] [Google Scholar]
- 10.Hay RJ, Roberts SOB, Mackenzie DWR. Mycology. In: Champion RH, Burton JL, Ebling FJG, editors. Book of dermatology. 5. Oxford: Oxford Blackwell Scientific Publication; 1992. p. 1127. [Google Scholar]
- 11.Pindborg JJ, Bhonsle RB, Murti PR, et al. Incidence and early forms of oral submucous fibrosis. Oral Surg. 1980;50:40–44. doi: 10.1016/0030-4220(80)90329-1. [DOI] [PubMed] [Google Scholar]
- 12.Dorey JL, Blasberg B, Conklin RJ, Carmichael RP. Oral leukoplakia current concept in diagnosis, management and malignant potential. Int J Dermatol. 1984;23(10):638–642. doi: 10.1111/j.1365-4362.1984.tb01221.x. [DOI] [PubMed] [Google Scholar]
- 13.Roed Peterson B, Renstrup G, Pindborg JJ. Candida in oral leukoplakia. A histologic and exfoliative cytologic study. Scand J Dent Res. 1970;78:323. doi: 10.1111/j.1600-0722.1970.tb02079.x. [DOI] [PubMed] [Google Scholar]
- 14.Silverman S, Jr, Bhargava K, Mani NJ, et al. Malignant transformation and natural history of oral leukoplakia in 57,518 industrial workers of Gujarat, India. Cancer. 1976;38(4):1790–1795. doi: 10.1002/1097-0142(197610)38:4<1790::AID-CNCR2820380456>3.0.CO;2-I. [DOI] [PubMed] [Google Scholar]
- 15.Mehta FS, Pindborg JJ, Gupta PC, et al. Epidemiologic histologic studies of oral cancer among 50,915 villagers in India. Cancer. 1969;24:832. doi: 10.1002/1097-0142(196910)24:4<832::AID-CNCR2820240427>3.0.CO;2-U. [DOI] [PubMed] [Google Scholar]
- 16.Schoenfeld RJ, Schoenfeld FI. Angular cheilitis. Cutis. 1977;19:213–216. [PubMed] [Google Scholar]
- 17.Ohman SC, Dahlen G, Moller A, et al. Angular cheilitis—a clinical and microbial study. J Oral Pathol. 1986;15:213–217. doi: 10.1111/j.1600-0714.1986.tb00610.x. [DOI] [PubMed] [Google Scholar]


