Abstract
Chronic conditions such as cancer, cardiovascular disease and mental illness are increasingly prevalent and associated with considerable psychosocial burden. There is a need to consider population health approaches to reducing this burden. Web-based interventions offer an alternative to traditional face-to-face interventions with several potential advantages. This systematic review explores the effectiveness, reach and adoption of web-based approaches for improving psychosocial outcomes in patients with common chronic conditions. A systematic review of published work examining web-based psychosocial interventions for patients with chronic conditions from 2001 to 2011. Seventy-four publications were identified. Thirty-six studies met the criteria for robust research design. A consistent significant effect in favour of the web-based intervention was identified in 20 studies, particularly those using cognitive behavioural therapy for depression. No positive effect was found in 11 studies, and mixed effects were found in 5 studies. The role of sociodemographic characteristics in relation to outcomes or issues of reach and adoption was explored in very few studies. Although it is possible to achieve positive effects on psychosocial outcomes using web-based approaches, effects are not consistent across conditions. Robust comparisons of the reach, adoption and cost-effectiveness of web-based support compared with other options such as face-to-face and print-based approaches are needed.
Introduction
Chronic conditions are defined as conditions that affect an individual over a prolonged period of time, do not tend to improve without treatment and often cannot be fully cured [1]. Examples of chronic conditions include cancer, cardiovascular disease and mental disorders, which are leading causes of morbidity in a number of developed countries [2, 3] and are becoming increasingly prevalent [4, 5]. These conditions are often associated with high levels of anxiety and depression [6, 7], suggesting that much of these populations may experience some level of psychosocial distress in their lifetime. For the purposes of this review, psychosocial health is defined as psychological and social well-being, as measured by tools such as those which assess depression, anxiety, stress, quality of life, self-efficacy and social support. Stress coping theory argues that an individual’s response to a potentially stressful event is based on his or her perception of the threat associated with the event and the resources available to them to cope [8]. Accordingly, attempts to minimize the negative effects of stress associated with chronic conditions are generally designed to assist the individual with cognitive and behavioural responses which will manage distress associated with their condition and any potential life-course implications. Chronic conditions such as Major Depressive Disorder adversely affect family relationships, social network and vocational roles [9, 10]. Up to 30% of cancer patients report depression or anxiety [11, 12], and diabetes is associated with high levels of distress and need for social support [13, 14]. Addressing psychosocial well-being has, therefore, become an expected part of delivering high-quality care to large and growing patient populations. Depression and anxiety are considered chronic health conditions in their own right, in addition to be considered psychosocial outcomes. Therefore, it is important to include these conditions in any comprehensive review of the effectiveness of web-based interventions for chronic health conditions.
Given the high combined prevalence of chronic conditions [15, 16], there is a need to consider population-level approaches to improving psychosocial health within available health care resources. Programs such as the Better Mental Health program in Australia [17] are designed to increase access to professional psychosocial support. Population-level effects of psychosocial interventions can be considered in terms of frameworks such as RE-AIM, including evaluation dimensions such as: (i) reach (the proportion of the target population that participates in the intervention); (ii) efficacy (success rate if implemented under ideal conditions) and (iii) adoption (proportion of settings or practices which will adopt the intervention) [18]. Each dimension is important for realizing the promise of any intervention across the relevant population. As a first step to achieving large-scale reductions in the psychosocial burden associated with chronic condition, it is crucial to identify interventions that are not only efficacious but also have high reach and adoption.
Interventions such as cognitive behavioural therapy have been shown to be effective for patients with mental health conditions when delivered face-to-face or by telephone [19–21]. However, from a population perspective, the reach and adoption of person-to-person approaches can be limited by geographical distance, cost and professional workforce capacity. This may be particularly so for rural patients and those with limited physical mobility and/or access to transport. Access to telephone-based support is also limited by the availability of qualified providers.
Reviews have suggested that web-based interventions may be effective for mental health conditions [22, 23]. The reach of web-based approaches is limited by whether an individual has access to the Internet. However, where Internet access is available, web-based approaches may reduce the geographical and resource constraints associated with face-to-face support [24–26]. Adoption of Internet-based interventions is less subject to the resourcing and timing constraints which can limit the uptake of telephone-based approaches. Web-based approaches can increase the reach of support, particularly for those with rarer conditions [26]. The anonymity of web-based interventions may also reduce the interpersonal discomfort some people may feel with respect to traditional forms of support such as support groups due to the anonymity they provide [27].
Web-based support options are proliferating as the Internet plays an increasingly important role in the way health resources and services are delivered [22, 28]. The web is often the first port of call for people seeking information, with US data showing that 48.6% of people referring to online resources and services before consulting a doctor [28]. Of those with Internet access, 64% [28] to 80% [29] searched for health information online. In several systematic reviews, it has been found that web-based information and support tools for chronic illnesses are effective in increasing patients’ knowledge and some health behavioural outcomes [30–32].
It is important to evaluate the potential of web-based interventions through the lens of equity. The most recent Australian data suggest that 72% of the population had home Internet access [33], whereas in the United States, up to 69% of people have home Internet access [34]. Differences in Internet access according to income, education, age and geographic location may reduce access to care for vulnerable or disadvantaged groups [35, 36]. Research into tobacco treatment programs, for example, suggested that web-based programs attract younger users but are also associated with lower success rates than other support modes such as telephone helplines [37]. Web-based programs can also be associated with high rates of drop-out [38], although a review by Melville et al. [39] suggested that drop-out rates for web-based interventions are similar to those seen in face-to-face treatment. Another review found that interventions that have no therapist input tended to report lower effect sizes than interventions that feature some level of therapist contact with participants [40].
To date little appears to be known about issues of effectiveness, reach and adoption of web-based health interventions across a range of chronic conditions. In some narrowly focused reviews, the effectiveness of web-based interventions for reducing psychosocial distress has been demonstrated [41, 42], yet none has looked more broadly at the effectiveness of web-based psychosocial interventions across a range of high-prevalence chronic conditions which have high prevalence across a number of developed countries such as cancer, cardiovascular disease, asthma, diabetes, depression, anxiety and obesity. In order to fully examine intervention reach and adoption, it is important to examine studies that cross topic- and population-boundaries. No review has provided such a perspective to date. The inclusion of studies with poor methodology is also a weakness of the available reviews [41, 42].
The study aims to identify:
whether methodologically robust studies of web-based psychosocial support for chronic conditions have demonstrated ‘effectiveness’ for improving psychosocial outcomes;
whether intervention effectiveness for robust studies was associated with sociodemographic and condition-related characteristics such as age, gender, income, education, ethnicity, time since diagnosis and condition severity;
whether ‘reach or adoption’ of web-based psychosocial support for robust studies was associated with sociodemographic and condition-related characteristics such as age, gender, income, education, ethnicity, time since diagnosis and condition severity.
These characteristics have been chosen due to the influence they have been shown to have in some studies on factors such drop-out rates [39].
Method
Search strategy
An online literature search of Medline, PubMed, PsycINFO and ProQuest was limited to articles published between January 2001 and December 2011 as the number of households with Internet access was low prior to 2000 and has since grown [33]. The search was restricted to English language articles on adult human subjects. The key search terms included: ‘information’; ‘psychosocial’; ‘social support’; ‘anxiety’; ‘depression’; ‘distress’; ‘disturbance’; ‘internet’; ‘web based’; ‘intervention’; ‘cancer’; ‘cardiovascular disease’; ‘asthma’; ‘diabetes’; ‘Major Depression’; ‘Anxiety’; ‘obesity’ and ‘Chronic Obstructive Pulmonary Disease’. Relevant databases (e.g. Cochrane library), contents of relevant journals and reference lists of identified papers were also searched for eligible studies. The chronic conditions selected were based on those which were consistently among the five most prevalent chronic conditions across a number of developed countries.
Inclusion and exclusion criteria
Publications that identified key terms in the title or abstract were retained. Studies that included web-based interventions designed to improve the psychological well-being or quality of life of patients with the following common chronic conditions were eligible for classification: cancer, cardiovascular disease, asthma, diabetes, chronic obstructive pulmonary disease, depression, anxiety or obesity. Psychosocial outcomes included were depression, anxiety, social support, quality of life, psychological well-being, emotional well-being, social well-being, self-efficacy, unmet needs, mood and daily functioning.
Web-based intervention studies were excluded if they: did not report the results of an intervention (e.g. research protocol and survey); used the web solely as a vehicle for gathering information rather than delivering interventions (e.g. web-based monitoring or surveys); did not have a psychosocial outcome measure or did not directly address the experience of a chronic illness (e.g. knowledge about cancer screening in a healthy population). Interventions aimed solely at health care providers or which did not directly deliver information or support (e.g. membership of a listserv, unmoderated discussion boards or providing contacts to potential peers) were excluded. Reviews, books, book chapters, letters, comments on publications and dissertations were also excluded.
Robust studies were selected for inclusion and were defined as those which met the Cochrane Collaboration criteria for appropriate design of research about Effective Practice and Organisation of Care (EPOC) [43] in terms of being one of the following study types:
randomized controlled trial;
controlled clinical trial;
controlled before and after trial;
interrupted time series.
The use of methodologically rigorous research design is an essential criterion for determining whether the research will contribute to evidence in the field [44].
Inter-rater reliability
Twenty percent of publications were randomly selected and independently coded by a second coder at each stage of the classification process (using a cross-section of publications from each year). Over 90% agreement was achieved between raters. Any discrepancies between raters were resolved by mutually agreed criteria, which were then applied to all studies.
When considering and reporting on sociodemographic variables that may influence the effectiveness of an intervention, we have used the term ‘gender’ to refer to biological sex or gender. However, the difference in these constructs is acknowledged.
Results
Publication sample
In total, 895 publications were identified; 821 (91.7%) were not relevant as they were duplicates (n = 372), contained non-chronic condition patient populations (n = 192, e.g. populations selected solely on the basis of age and gender, such as population-based cervical screening studies); were not intervention studies (n = 104); were not web-based (n = 29); did not have a psychosocial outcome measure (n = 32); included only participants < 18 years of age (n = 18); were aimed at health care providers (n = 11); were reviews (n = 53) or were book chapters (n = 3). Some publications were excluded on multiple criteria.
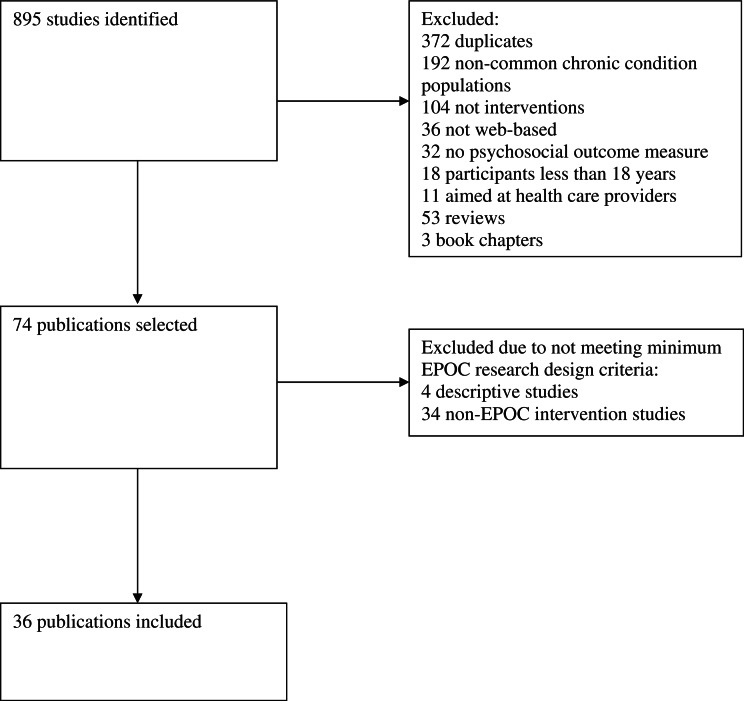
Seventy-four publications that examined the effectiveness of web-based interventions and support for patients with common chronic conditions were identified. Multiple publications on the same intervention study were ‘counted’ as one study, i.e. [45–47] and [48, 49]. The 74 publications included: descriptive studies (n = 4) or non-EPOC intervention studies (n = 34, e.g. no control group). Thirty-six studies met the minimum EPOC research design criteria (Fig. 1).
Fig. 1.
Flow diagram of studies selected for inclusion in review.
The main focus area for these studies was mental illness unrelated to other conditions, followed by diabetes and cancer. All studies used a randomized controlled trial design. The most common intervention approach was web-based self-guided cognitive-behavioural therapy. Interventions also often incorporated online discussion groups or forums, relevant information resources and techniques to develop coping strategies. Common outcome measures of intervention effectiveness included the Centre for Epidemiological Studies Depression Scale (CES-D), Beck Depression Inventory (BDI) and Patient Health Questionnaire (PHQ-8).
Findings
Effectiveness of robust studies
The findings of the robust studies are presented in Table I. In 20 of the 36 studies, a significant positive effect on psychosocial outcomes in favour of the web-based intervention was identified [45–67]. A mixture of positive and null findings for psychosocial outcomes was demonstrated in four studies [68–71]. In 11 studies, no positive effect on any psychosocial outcome was found [72–82]. In one study, although a significant treatment effect in favour of the web-based intervention was reported, a greater reduction in depression was associated with lesser web usage was identified [83].
Table I.
Effectiveness of web-based interventions for the provision of information and support
| Author, country | Participant group | Condition | Drop-out rates | Intervention | Control | Psychosocial outcome measures | Treatment effects | Predictors |
|---|---|---|---|---|---|---|---|---|
| Mental illness unrelated to other conditions (n = 19) | ||||||||
| Hedman et al. [81] Sweden | 126 patients aged 18–64 years | Social Anxiety Disorder (SAD) according to DSM-IV criteria | 13% at post-treatment, 22% at 6 months | Internet-based cognitive behavioural therapy (n = 64): 15 weeks of Internet-based self-help modules and access to a therapist via an online messaging system | Cognitive Behavioural Group Therapy (n = 62) | Liebowitz Social Anxiety Scale (LSAS), Beck Anxiety Inventory (BAI), Anxiety Sensitivity Index (ASI), Montgomery Asberg Depression Rating Scale-self report (MADRS-S) and Quality of Life Inventory (QOLI) | No treatment effect | N/A |
| Mailey et al. [79] USA | 51 university students aged 18–52 years | General Mental Health concerns: Students attending mental health counselling service and continued to attend counselling throughout the study | 8% (Estimate) | Internet-based physical activity program (n = 26): 10-week physical activity program including wearing a pedometer and keeping an activity log, access to a study website with information about exercise and overcoming barriers and meetings with physical activity counsellors | Usual care (n = 25) | State Trait Anxiety Scale (STAI); Beck Depression Inventory (BDI) | No treatment effect | N/A |
| Meglic, et al. [65] Slovenia | 46 patients Intervention mean age was 35.71 years (SD = 12.11) | Depression (ICD10 code F32), or mixed anxiety and depression disorder (ICD10 code F41.2) | 52% | Improvehealth.eu (n = 21): 24 weeks web-based information and communication program, as well as online and phone-based care management by psychologist | Usual care (n = 25) | Beck Depression Inventory II (BDI-II) | Significant treatment effect: Intervention group showed greater improvement in depression (BDI-II) at 6 months (ES = 1) | N/A |
| Control mean age was 40.04 years (SD = 17.07) | ||||||||
| Roy-Byrne, et al. [59] USA | 1004 primary care patients aged 18–75 years | Anxiety disorder (PD, GAD, SAD or PTSD) according to DSM-IV with an Overall Anxiety Severity and Impairment Scale (OASIS) score ≥8 | 13% at 6 months. 19% at 12 months, 20% at 18 months | CALM (n = 503): a cognitive-behavioural treatment program with newly develop anxiety content model on the Improving Mood-Promoting Access to Collaborative Treatment (IMPACT) Intervention. This was typically administered weekly for 6–8 weeks. Patients thought to benefit from more treatment were offered up to three more steps. This was followed by monthly follow-up calls to reinforce CBT skills, medication adherence or both for the remaining 18 months | Usual care (n = 501) | 12-Item Brief Symptom Inventory (BSI-12); Patient Health Questionnaire (PHQ-8) | Significant group * time interaction effect: BSI-12 scores significantly lower for intervention than control at 6 months (ES = 0.30), 12 months (ES = 0.31) and 18 months (ES = 0.18) | N/A |
| Berger et al. [72] Switzerland | 52 patients who were 19–43 years and were not receiving any other psychological treatment for the duration of the study. Participants had Internet access | Social phobia: met DSM-IV diagnostic criteria | 10% | Internet-based cognitive-behavioural therapy’ (n = 31): 10-week nternet-based program including an interactive self-help guide, a monitoring/feedback systems and group collaboration providing opportunity to share experiences | Waiting list (n = 21) | Beck Depression Inventory (BDI); Inventory of Interpersonal Problems (IIP) | No treatment effect | N/A |
| Clarke et al. [83] USA | (i) 109 individuals aged 18–24 years ; and (ii) 51 age-matched adults Participants had Internet access | (i) Diagnosed with depression or had received medical services for depression (psychotherapy or medication) (ii) Not diagnosed with depression and had not received depression-related health care, but displayed elevated health care utilisation | 37% at 32 weeks | Internet-based cognitive-behavioural therapy (n = 83): self-guided, interactive cognitive and behavioural therapy tutorials designed to overcome depression. Participants had access to the intervention throughout the study (32 weeks) and received reminder letters at 2, 8 and 13 weeks after recruitment | Usual care (n = 77) | Patient Health Questionnaire (PHQ-8) | Significant treatment effect: Decrease in PHQ-8 scores favouring treatment group at 32 weeks post-treatment (ES = 0.20) | Improved group * time interaction effect for female-only population (ES = 0.42) |
| Greater depression reduction associated with lower website usage in treatment arm (fewer minutes of usage and pages accessed) | ||||||||
| Kessler et al. [55] UK | 297 primary care patients aged 18–75 years | Depression (BDI score >14 and confirmed diagnosis through clinical interview) | 29% at 4 months | Online cognitive-behavioural therapy in addition to usual care (n = 149): 10 CBT session delivered by a therapist online in real time completed within 16 weeks of randomization when possible | Waiting list (n = 148) | Beck Depression Inventory (BDI); Short form mental score (SF-12); EuroQoL (EQ-5D) | Significant treatment effect: patients in the treatment group more likely to have recovered at 4 months post-treatment. Thirty-eight percent of the treatment group were in recovery (BDI < 10) whereas only 24% of the control were in recovery (Adjusted OR = 2.39, P = 0.011) | N/A |
| Meyer et al. [58] Germany | 396 adults. Intervention mean age was 34.58 years (SD = 11.53). Control mean age was 35.47 years (SD = 11.98). | Assumed depression: participants were recruited via advertisement posted on depression-related Internet forums | 45% at 9 weeks, 63% at 18 weeks and 75% at 6 months | Deprexis (n = 320): 9 weeks of online tailored psychotherapy including behavioural activation and cognition modification, mindfulness and acceptance, interpersonal skills, problem-solving and psycho-education | Waiting list (n = 76) | Beck Depression Inventory (BDI); Work and Social Adjustment Scale (WSA) | Significant treatment effect: decrease in depression severity favouring Deprexis condition (BDI scores, ES = 0.64) and significant improvements in social functioning (ES = 0.64). | N/A |
| Kiropoulos et al. [74] Australia | 86 Victorian residents aged 20–64 years | Panic Disorder according to DSM-IV criteria and assessed with the anxiety disorders interview schedule (ADIS-IV) | 8% | Panic Online (n = 46): Internet-based treatment program based on standard CBT for panic disorder | Face-to-face treatment (n = 40): 1 h weekly manualized CBT treatment sessions for 12 weeks | Depression, Anxiety, Stress Scales (DASS); World Health Organization Quality of Life (QOL) | No treatment effect or group * time interaction effect at the end of the 12-week intervention period | N/A |
| Mackinnon et al. [45]; Christensen et al. [46]; Christensen et al. [47] Australia | 525 individuals who were not receiving any other psychological treatment. Participants had Internet access | Psychologically distressed: Kessler psychological distress scales score >22 |
|
|
Attention placebo (n = 178): weekly contact with lay interviewer to discuss lifestyle factors | Centre for Epidemiological Studies Depression Scale (CES-D) | Significant group * time interaction effect: Reduced depression symptoms (using CES-D) favouring treatment groups at the end of the intervention period (ES = 0.38 for MoodGYM versus control and ES = 0.29 for BluePages versus control) and 6 (ES = 0.27 for MoodGYM versus Control, ES = 0.21 for BluePages versus Control) and 12 months post-treatment (ES = 0.27 for MoodGYM versus Control, ES = 0.29 for BluePages versus Control) | N/A |
| Note: participants in both treatment condition were contacted weekly over 6 weeks by lay interviewer to direct their use of the intervention websites | ||||||||
| Spek, et al. [48]; Spek, et al. [49] The Netherlands | 301 adults aged 50-75 years. Participants had access to the Internet and were able to use it | Subthreshold depression: Edinburgh Depression Scale (EDS) scores >12, but no DSM-IV diagnosis of depression. | 37% at 1 year post-test |
|
Waiting list (n = 100) | Beck Depression Inventory (BDI) | Significant treatment effect: There were significant improvements in depression symptoms (BDI scores) favouring Internet treatment group compared with waiting list (ES = 0.53), with no significant different between Internet treatment group and Coping with Depression group (p = .08) 12 months post-treatment | N/A |
| van Straten et al. [61] The Netherlands | 213 participants whose mean age was 45.2 years (SD = 10.6) | Participants expressed an interest in involvement by responding to advertisements about self-help treatments for depression, anxiety and work-related stress symptoms | 17% | Web-based problem-solving intervention (n = 107): 4-week online course focused on mastering problem-solving strategies | Waiting list (n = 106) | Centre for Epidemiological Studies Depression Scale (CES-D); Major Depression Inventory (MDI); Hospital Anxiety and Depression Scale (HADS); anxiety section of the Symptom Checklist (SCL-A); Maslach Burnout Inventory (MBI) | Significant treatment effect: improvement in depression and anxiety symptoms favouring Internet treatment group at the end of the 5-week intervention period (ES for CES-D = 0.50; MDI = 0.33; HADS = 0.33; and SCL-A = 0.42) | N/A |
| Warmerdam et al. [62] The Netherlands | 263 adults whose mean age was 45 years (SD = 12.1). Participants had access to the Internet and an email address | Depressive symptoms defined as CES-D scores >16 | 30% at 5 weeks, 34% at 8 weeks and 43% at 12 weeks |
|
Waiting list (n = 87) | Centre for Epidemiological Studies Depression Scale (CES-D); Hospital Anxiety and Depression Scale (HADS); EuroQoL Questionnaire (EQ5D) | Significant group * time interaction effect: improvements in depression (CES-D), anxiety (HADS) and quality of life (EQ5D) favouring both treatment groups at 8 weeks and 12 weeks following baseline measurement, with no significant different between CBT group and PST group. Effect sizes at 12 weeks follow-up for depression were 0.69 and 0.65; for anxiety were 0.52 and 0.50 and for QoL were 0.36 and 0.38, for CBT and PST, respectively, compared with the waitlist | N/A |
| Knaevelsrud, et al. [56] The Netherlands | 96 patients aged 18–68 years | Post-traumatic distress—Impact of Event Scale score ≥20 | 9% | Interplay (n = 49): 5-week Internet-based cognitive behavioural therapy | Waiting list (n = 47) | Brief Symptom Inventory (BSI) | Significant treatment effect: improvements in BSI depression (ES = 1.16) and BSI anxiety (ES = 1.08) favouring treatment group at post-treatment | N/A |
| Seligman et al. [60] USA | 240 university undergraduates | At risk of depression (BDI score between 9 and 24) | 5% | Workshop plus web-based supplement (n = 102): 8 weekly group workshop meetings plus web-based between-meeting homework | Usual care (n = 102) | Beck Depression Inventory (BDI); Beck Anxiety Inventory (BAI); Satisfaction with Life Scale (SLC); Fordyce Emotions Questionnaire | Significant group * time interaction effect: fewer depression and anxiety symptoms (BDI scores, post-treatment ES = 0.67, 6 months follow-up ES = 0.59), and greater happiness and life satisfaction (SLC scores) favouring treatment group at post-treatment (ES = 0.24) and 6 months post-treatment (ES = 0.30) | N/A |
| Carlbring et al. [64] Sweden | 60 patients aged 18–60 years. Participants had access to a computer with the Internet and printer | Participants met DSM-IV criteria for panic disorder and had suffered from this for at least 1 year | 5% | Multi-modal cognitive-behavioural therapy with minimal therapist contact (n = 30): 10-week 10-module interactive Internet-based program which included online discussion groups. Participants also received weekly telephone calls and emails from therapist | Waiting list (n = 30) | Beck Depression Inventory (BDI); Quality of Life Inventory | Significant group*time interaction effect: for BDI and Quality of Life Inventory favouring treatment group at post-treatment and 9 months post-treatment. | N/A |
| Significant post-treatment difference for groups: on BDI (ES = 0.61) favouring treatment group; gains were maintained at 9 months follow-up. | ||||||||
| Good compliance rates: 80% of participants finished all modules with 10-week treatment duration | ||||||||
| Clarke et al., [52] USA |
|
|
34% at 16 weeks |
|
Information-only (n = 100) | Centre for Epidemiological Studies Depression Scale (CES-D); Short-Form 12 (SF-12) | Significant treatment effect: improvements in self-reported depression (CES-D) favouring treatment groups at 5, 10 and 16 weeks post-enrolment (ES = 0.277). No difference between treatment groups and no effects on the physical or mental components subscales of the SF-12 | A more pronounced treatment effect was detected among participants with more severe baseline depression scores (ES = 0.537) |
| Patten [78] Canada | 786 individuals whose mean age was 45.2 years (SD = 11.9). | Major Depression diagnosed using the Composite Internal Diagnostic Interview(CIDI) | 3% | Interactive CBT program (n = 420) | Information-only (n = 366) | Centre for Epidemiological Studies Depression Scale (CES-D) | No treatment effect at 3 months post-treatment | N/A |
| Clarke et al. [73] USA |
|
Depression: recorded diagnosis of depression | 41% by 32 weeks | Internet-based cognitive therapy (n = 144): self-paced program for mild-to-moderate depression, or as an adjunct for more traditional services for more severe depression (available throughout the whole 32-week study) | Usual care (n = 155) | Centre for Epidemiological Studies Depression Scale (CES-D) | No treatment effect at 4, 8, 16 and 32 weeks post-enrolment | For participants with low baseline CES-D scores, treatment group was significantly less depressed than control group at 16 (ES = 0.17) and 32 weeks post-enrolment (ES = 0.48) |
| Diabetes (n = 7) | ||||||||
| van Bastelaar et al. [66] The Netherlands | 255 diabetic patients (mean age = 50 years, SD = 12) | Diabetes (both Type 1 and Type 2). Patients had elevated depressive symptoms defined as a score of ≥ 16 on the CES-D | 32% post-assessment; 35% at 1 month | Web-based cognitive behaviour therapy for depression symptoms (n = 125); eight consecutive lessons, health psychologists provide feedback on homework assignments | Waiting list (n = 130) | Centre for Epidemiological Studies Depression Scale (CES-D) | Intervention was effective in reducing depressive symptom (CES-D, ES = 0.29 at 1 month follow-up), reduced diabetes-specific emotional distress but no effect on glycaemic control | N/A |
| Quinn et al. [82] USA | 163 patients (mean age 52.8 years) | Type 2 diabetes | 11% | 12 months of: Patient coaching only (n = 38), online management of self-care data, with automated educational and motivational messaging; Patient coaching and clinical provider access (n = 33), clinical providers could access unanalysed patient self-care data; Patient-coaching system and provider clinical decision support (n = 80), clinical providers could access patients’ self-care data linked to guidelines and standards of care | Usual care (n = 62) | Patient Health Questionnaire-9 (PHQ); 17-item Diabetes Distress Scale | No differences observed between groups for diabetes distress and depression | N/A |
| Bond et al. [51] USA | 62 patients aged 60 years and older. Ensured participants had access to computer (provided a computer if necessary) | Diabetes (type not specified), who have been diagnosed for at least 1 year | Not reported | Web-based intervention plus usual care (n = 31): weekly online discussion sessions and monitoring tools aimed at improving patients’ self-management behaviours and well-being for a year | Usual care (n = 31) | Centre for Epidemiological Studies Depression Scale (CES-D); Problem Areas in Diabetes Scale (PAID; measure of QoL); Diabetes Support Scale (DSS); Diabetes Empowerment Scale (DES) | Significant treatment effect: improvements in depression (CES-D, ES = 0.7), self-efficacy (DES, ES = 0.7), Quality of Life (PAID, ES = 0.6) and social support (DSS, ES = 1.0) favouring treatment group at 6 months post-baseline | Significant main effect of mediation type (insulin use, oral glycaemic agent or no medication), with oral glycaemic agent category showing the greatest improvements. No significant main effect for number of years with diabetes or number of co-morbidities |
| Liebreich et al. [75] Canada | 49 patients with a mean age of 54.5 years (SD = 10.8). Participants had Internet and email access | Type 2 diabetes | 10% | Diabetes NetPLAY (n = 25): 12 weeks of online psycho-education including physical activity logbook, message board and email counselling | Usual care (n = 24) | Self-efficacy; Social support | No treatment effect at the end of the 12-week intervention period | N/A |
| Glasgow et al. [68] USA | 320 primary care patients with a mean age of 59 years (SD = 9.2) Participants have very little or no Internet experience prior to the study | Type 2 diabetes, diagnosed for at least 1 year | 82% | 10 months of: (i) Tailored self-management training plus information: online access to ‘coach’ who provided expert dietary advice, encouragement and tailored strategies to overcome problems/barriers | Information-only | Centre for Epidemiological Studies Depression Scale (CES-D); Diabetes Support Scale (DSS) | Mixed: No significant treatment effects except for DSS, for which the Peer Support group produced a significantly greater improvement at 10 months post-baseline compared with no peer support (P = 0.001) | N/A |
| (ii) Peer support plus information: Interactive form where participants were able to share diabetes-relation information, coping strategies and support | ||||||||
| Barrera et al., [50] USA | 120 patients aged 40–75 years. Participants were provided with computers and Internet access for the duration of the intervention | Type 2 diabetes, diagnosed for at least 1 year | 23% | 3 months of:
|
Information-only (n = 40) | Interpersonal Support Evaluation List (ISEL); Diabetes Support Scale (DSS) | Significant treatment effect: favouring treatment groups, with Social Support Only group experienced the greatest increases in perceived social support (DSS scores) at 3 months post-baseline (P < 0.01). Effect sizes not reported | Age was significantly related (P < 0.05) to change in DSS scores (perceived social support), significant condition effect was still present once age was accounted for |
| McKay et al. [76] USA | 78 adults aged ≥ 40 years | Type 2 diabetes | 13% | D-Net Active Lives (n = 38): an 8-week, tailored physical activity program | Information-only (n = 40) | Centre for Epidemiological Studies Depression Scale (CES-D) | No treatment effect at post-treatment | N/A |
| Cancer (n = 7) | ||||||||
| Hawkins et al. [67] USA | 434 women Usual care—mean age 52.3 years (SD = 10.2) | Breast Cancer | 5% | 6 months of:
|
Usual care (n = 112) | Quality of Life (WHOQOL-BREF) | Significant treatment effect | N/A |
| CHESS—mean age 50.9 years (SD = 9) | ||||||||
| Mentor—mean age 53.9 years (SD = 10.9) | Those in the CHESS plus mentor group scored higher on Quality of Life than all other groups (P < 0.05). The CHESS-alone group and the Mentor-alone group scored no better than the usual care group | |||||||
| CHESS + Mentor—mean age 52.7 years (SD = 9.4) | ||||||||
| Loiselle et al. [80] Canada | 250 patients with breast or prostate cancer. | Breast or Prostate Cancer | 7% | Provided with training to use IT (n = 148, 8 weeks): Given a list of reputable cancer websites to browse, as well as a tailored informational CD-ROM | Usual care (n = 102) | State-Trait Anxiety Inventory (STAI), Centre for Epidemiological Studies Depression Scale (CES-D), Short Form 36 (SF-36), Index of Wellbeing, Rosenberg Self-Esteem Scale | No significant treatment effect | N/A |
| Breast cancer treatment mean age = 53.5 years (SD = 10.7) | ||||||||
| Breast cancer control mean age = 57.3 years (SD = 12.6) | ||||||||
| Prostate cancer treatment mean age = 62.3 years (SD = 7.7) | ||||||||
| Prostate cancer control mean age = 67.7 years (SD = 9.6) | ||||||||
| Hoybye et al. [53] Denmark | 799 cancer survivors attending a rehabilitation course | Various types of cancer. | 15% at 12 months (estimate) | Internet-based peer support group plus rehabilitation program (n = 438). The Internet-based group was accessible via invitation and available to access 24 h a day for 13 months from the individuals starting date | Rehabilitation program (n = 366), a 6-day retreat | Short version of the Profile of Mood States (POMS); Mini-Mental Adjustment to Cancer (Mini-MAC) | Significant transient difference at 6-month follow-up, with treatment group reporting more anxious preoccupation (P = 0.04), helplessness (P = 0.002, Mini-MAC), and confusion/bewilderment (P = 0.001) and depression/dejection (P = 0.04, POMS). | Gender, marital status, employment or education did not impact intervention outcomes |
| Significant transient difference at 12-month follow-up, with treatment group reporting more vigour/activity (P = 0.001, POMS) | ||||||||
| Gustafson et al. [69] USA | 257 patients within 61 days of diagnosis. Participants were provided with computers and Internet access for the duration of the intervention | Breast cancer | 2% at 2 months, 4% at 4 months, 7% at 9 months | 5 months of:
|
Information-only (n = 83): books or audiotapes on breast cancer | Functional Assessment of Cancer Therapy-Breast (FACT-B); Social Support Scale (SSS) | Mixed: no significant between-group difference for Internet access and control condition at 2, 4 or 9 months. Significant between-group difference favouring CHESS at 9 months for both measures (FACT-B ES = 0.39, SSS ES = 0.38) and at 4 months for social support (ES = 0.46) | N/A |
| Owen et al. [77] USA | 62 women | Early stage Breast cancer | 15% | Self-guided coping-skills and support intervention (n = 32): consisting of an Internet-based discussion board coping group, 12 weeks of self-guided delivery of coping-skills training exercises and education on symptom management | Waiting list (n = 30) | Functional Assessment of Cancer Therapy-Breast Cancer Form (FACT-B); Impact of Events Scale (IES) | No treatment effect at post-treatment | N/A |
| Treatment mean age 52.5 years (SD = 8.6) | ||||||||
| Control mean age 51.3 years (SD = 10.5) | ||||||||
| Winzelberg et al. [63] USA | 72 women 30–69 years old. Participants were provided with computers and Internet access for the duration of the intervention | Early stage Breast cancer | 19% | Bosom Buddies (n = 36): 12-week structured, web-based support group mediated by a mental health professional | Waiting list (n = 36) | Centre for Epidemiological Studies Depression Scale (CES-D); PSTD Checklist-Civilian version (PCL-C); State-trait Anxiety Inventory-State Scale (STAI); Perceived Stress Scale (PSS) | Significant treatment effect favouring treatment groups was found for all measures except STAI at post-treatment (CES-D ES = 0.54, PCL-C ES = 0.45, PSS ES = 0.37) | Time since diagnosis was not significantly correlated with changes in outcome measures |
| Gustafson et al. [70] USA | 295 patients aged ≤ 60 years. If participants did not have a computer/Internet, they were provided with these for the duration of the study | Newly diagnosed Breast cancer | 17% | CHESS (n = 147): access to an online system of breast cancer resources including information, communication and decision services for 6 months | Information-only (n = 148) | Social Support; Functional Assessment of Cancer Therapy-Breast Cancer Form (FACT-B) | Mixed: No difference on FACT-B. | Benefits greater for disadvantaged groups |
| Higher level of social support at 5 months favouring CHESS group (P < 0.01). | ||||||||
| Other common chronic conditions (n = 3) | ||||||||
| Brennan et al. [71] USA | Six home care nursing agencies incorporating 282 patients aged 28–93 years. Agencies randomized to condition; however, the authors do not appear to have adjusted for clustering in results | Chronic Cardiac Disease | 19% by 8 weeks | Technology enhanced practice (TEP) (n = 146): web-based tools to assist with education, symptom monitoring and communication available for 24 weeks | Usual care (n = 136) | Clinical Status (SF-12); Multidimensional Index for Life Quality Questionnaire for Cardiovascular Disease (MILQ) | Mixed: No differences on MILQ, Higher mental health (SF-12) for TEP group at 1 and 8 weeks post-baseline. Effect sizes not reported | N/A |
| Kerr et al. [54] USA | 401 women aged 18–55 years | Overweight—BMI of 25–39 | 29% | Patient-centred Assessment and Counselling for Exercise and nutrition via the Internet (PACEi) (n = 206): 1-year stage-based action plan to improve physical activity and nutrition behaviours | Enhanced standard care (n = 196): usual care plus a standard material summarizing recommendation for diet and exercise | Short-form Centre for Epidemiological Studies Depression Scale (CES-D-SF) | Significant group * time interaction effect: improvements in depression favouring treatment group at post-treatment (P < 0.05). No effect sizes reported | N/A |
| Lorig et al. [57] USA | 958 adults aged 22–89 years. Participants had Internet and email access | Heart disease, chronic lung disease, or type 2 diabetes diagnosed by a physician | 19% | Internet chronic disease self-management program (n = 457): interactive web-based instruction, web-based bulletin board discussion groups and reference book Living a Health Life with Chronic Conditions spanning over 6 weeks | Usual care (n = 5 01) | Health Distress Scale; Perceived self-efficacy | Significant group * time interaction effect: for Health Distress Scale scores favouring treatment condition at 12 months post-enrolment (ES = 0.160). Self-efficacy showed a strong trend towards significance at 12 months post-enrolment (ES = 0.096) | N/A |
Note: ES, effect size.
Of the 19 studies focused on anxiety or depression, unrelated to other conditions such as diabetes, heart disease or cancer, positive effects in terms of reduced rates of depression or anxiety compared with controls were reported in 13 studies [45, 48, 52, 55, 56, 58–62, 64, 65, 83]. Of the six studies in this pool in which no effect was found, three had very small sample sizes [72, 74, 79] and a significant effect only for those with mild depression in one study [73]. In one well-powered study, it was found that participants with major depression did not benefit from the intervention compared with control group participant [78]. In another study, it was shown that Internet-based CBT was just as effective in reducing anxiety and depression as group-based CBT, which was designated as the control in this study [81]. The likelihood of finding a positive treatment effect did not seem to be related to the intensity of the course or the inclusion of additional non-web-based assistance such as telephone access to a therapist. This group of interventions was characterized by a structured, 6- to 12-week CBT-based approach, with five of the studies involving a ‘live’ therapist either online [55, 64, 65, 81] or in additional face-to-face groups [60]. Others included regular reminders or prompts to use the website [45, 52].
Of the seven studies with diabetes patients, positive effects on psychosocial outcomes including depression, social support and empowerment were found in three [50, 51, 66]. Positive effects on social support, but not depression were reported in one study [68]. These interventions were characterized by self-monitoring, encouragement and peer support, with varying levels of intensity and structure. Most studies in this group used the Diabetes Support Scale to measure social support outcomes and the CES-D to measure depression.
In the case of the seven studies with cancer patients, statistically significant positive effects were found in two studies on depression and stress [63] and quality of life [67] for a web-based support group mediated by a professional. A mixture of positive and negative effects on mental adjustment and mood was reported in one study [53]; and a mixture of positive and null effects regarding social support depending on the follow-up timeframe were found in two other studies [69, 70]. No effect on well-being was described in a further two studies [77, 80]. All but two [53, 80] of the seven cancer studies involved breast cancer patients exclusively, with Hoybye et al. [53] including patients with a range of tumour types and Loiselle et al. [80] including both breast and prostate cancer patients. Sample sizes for the seven cancer studies ranged from less than 100 per cell [63, 69, 77] to over 400 participants per cell [53]. Intervention content involved primarily information provision, discussion groups, decisional support, coping skills and peer support. While two studies involved a structured, multi-week course [63, 77], most involved unstructured Internet access.
Regarding the three interventions with other chronic conditions, statistically significant positive or mixed effects were reported on psychosocial variables including on depression in overweight women [54], on health distress for a group of patients with a mixed aetiology of chronic conditions (e.g. heart disease, lung disease or type 2 diabetes) [57] and on mental health for patients with chronic cardiac disease [71].
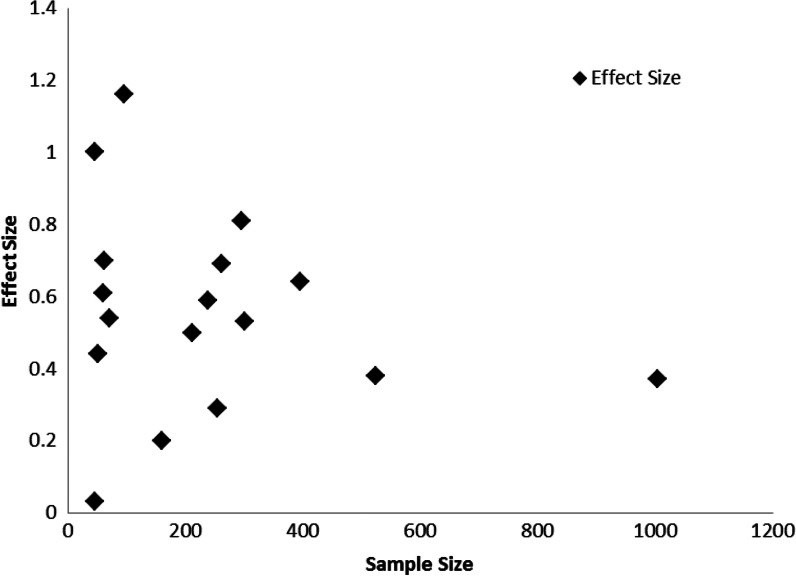
As can be seen in Fig. 2, effect size did not appear to be systematically related to sample size in the publications included in this review, suggesting publication bias was unlikely to be a concern for the reviewed studies. However, given that only 17 of the 36 papers included in the review reported an effect size as part of their results [45, 48, 51, 55, 56, 58–66, 72, 79, 83], it is difficult to draw more firm conclusions based on this finding.
Fig. 2.
Effect size as a function of sample size in included studies.
Differences in effectiveness according to sociodemographic and condition-related characteristics
Studies that explored whether participant factors mediated outcome effectiveness were focused on both condition-related variables [51, 52, 63, 73] and sociodemographic characteristics [50, 53, 70, 83]. Clarke et al. [83] found an improved treatment effect for female participants compared with male participants. For patients with diabetes, increasing age was significantly related to less improvement in perceived diabetes-related support [50]. Hoybye et al. [53] found that mood and adjustment outcomes for cancer patients were not related to gender, marital status, employment or education. Gustafson et al. [70] found a greater reduction in unmet information need and greater improvements in information competence for women of colour and women with lower levels of education.
For those with a mental illness unrelated to other conditions, a more pronounced treatment effect was found by Clarke et al. [52] for participants with more severe depression scores at baseline. Clarke et al. [73] who failed to identify an overall treatment effect found a significant treatment effect only for participants with low baseline depression scores (approximately 20% of participants). The lack of an overall treatment effect for the majority of participants in Clarke et al.’s (2002) study [73] may be attributable to the low usage rates of the intervention website. Usage rates were increased in their 2005 study by using postcard or telephone reminders. Bond et al. [51] found that compared with patients who did not take medication for their diabetes, patients who received insulin or an oral glycaemic agent showed the greatest improvements in psychosocial outcomes. The effects of time since diagnosis on psychosocial outcomes for cancer patients were not statistically significant [63].
Differences in reach and adoption according to sociodemographic and condition-related characteristics
Sociodemographic and/or condition-related characteristics associated with reach (those who were eligible and consented to participate) or adoption (those accessing or using the intervention) were examined in 11 studies [47, 49, 53, 54, 57–59, 61, 62, 66, 67] (Table II). The proportion of patients who were excluded on the basis of not having Internet access, or compared the characteristics of those with and without access to the Internet was not reported in any studies.
Table II.
Characteristics of intervention users versus non-users
| Author | Proportion using intervention | Characteristics studied | Differences between users and non-users |
|---|---|---|---|
| van Bastelaar et al. [66] | 70% completed at least one lesson and 42% completed all eight lessons | Age | Dropouts more often diagnosed with an anxiety disorder. Dropouts in control group had higher baseline depression scores. Attrition higher in non-completers of the course at 1-month |
| Gender | |||
| Education | |||
| Marital status | |||
| Condition status | |||
| Hawkins et al. [67] | NA | Age | Dropouts in CHESS + Mentor condition likely to be older, dropouts in usual care condition likely to be younger |
| Hoybye et al. [53] | NA | Age | Compared with users, non-users were more likely to be single, older males with a lower education, unemployed and not using the Internet at baseline |
| Gender | |||
| Education | |||
| Marital status | |||
| Employment | |||
| Experience with Internet | |||
| Roy-Byrne et al. [59] | 95% had at least one intervention contact | None | NA |
| Meyer et al. [58] | 78% completed at least one session of more than 10 min | Age | None |
| Gender | |||
| Condition status | |||
| Kerr et al. [54] | NA | Condition status | Level of depression was very similar between dropouts and study completers |
| van Straten et al. [61] | 91% completed at least one module and 55% completed all modules | Age | Users were significantly more likely to be married than non-users |
| Gender | |||
| Education | |||
| Marital status | |||
| Employment | |||
| Alcohol problems | |||
| Warmerdam et al. [62] | 88% completed at least one module and 38% completed all modulesCompletion of all modules associated with higher education | Condition status | Users with lower baseline levels of depression more likely to complete treatment than dropouts |
| Spek et al. [49] | NA | Age | None |
| Gender | |||
| Education | |||
| Income marital status | |||
| Employment | |||
| Condition status | |||
| Lorig et al. [57] | NA | Gender | Users were significantly more likely to females and less likely to be non-Hispanic or white than dropouts |
| Ethnicity | |||
| Christensen et al. [47] | NA | Treatment condition | Higher dropout rate from MoodGYM compared with BluePages |
| Condition status | Dropouts had higher rates of psychological distress at baseline |
NA, not assessed.
The proportion of participants who accessed the intervention was specifically explored in five studies [58, 59, 61, 62, 66]. It was found that uptake rates varied from 70% to 95% of potential users. This does not, however, suggest high rates of reach as participants had to have some form of Internet access in order to be included in the denominator of such calculations. Predictors of intervention use included: age (younger more likely to use intervention) [53, 67], gender (women more likely to use intervention) [53, 57], marital status (users more likely to be married) [53, 61], ethnicity (users more likely to be Caucasian) [57], lower baseline levels of depression [47, 62] and previous experience with the Internet [53].
No studies examined sociodemographic differences in comprehension of the resources, acceptability of the intervention approach or satisfaction with the intervention content.
Discussion
This exploration of the literature regarding web-based approaches for achieving improvements in psychosocial outcomes for people with chronic conditions has indicated that while effectiveness is achievable, it is not consistent across conditions and issues of reach and adoption are relatively unstudied.
Effectiveness
Mainly positive intervention effects were demonstrated in studies of web-based interventions for patients with a mental illness unrelated to other conditions. However, a major weakness of this research literature is the lack of generalizability due to self-selected volunteer samples. High participant drop-out rates are also evident, further limiting the generalizability of the data. When assessing the effectiveness of an intervention, we reported the results of ‘intention-to-treat’ analyses from the reviewed papers, in order to account for issues of adherence. Intention-to-treat analyses consider all recruited participants in the denominator, not just participants who complete the final follow-up. This approach minimizes the effect of non-random attrition on the results. Of the few available studies regarding conditions such as diabetes and cancer, the data did not suggest that web-based approaches were particularly effective in reducing psychological disturbance. Mixed findings for psychosocial outcomes have also been noted in relation to other intervention modalities for such groups [84, 85].
The apparent difference between the findings for those with mental illness only compared with those with diabetes or cancer may be related to a number of factors. First, the intervention content for the mentally ill populations focused on web-based application of CBT, an approach that has shown proven effectiveness for the treatment of anxiety and depression when delivered in a face-to-face setting [19, 86]. The diabetes and cancer pool of studies had less focused intervention content, possibly due to the need to address physical symptom management alongside psychosocial health. Perhaps such interventions should draw more heavily on the application of more focused and structured strategies, such as CBT. Second, the interventions for the mentally ill populations were relatively structured and intensive (e.g. 10 weekly sessions). The diabetes and cancer-related interventions were largely self-directed, although a significant positive intervention effect on several psychosocial outcomes was reported in one study that involved a 12-week structured web-based support group moderated by a health care professional found [63]. No significant treatment effect was found in another study with cancer patients, which utilized a 12-week program involving coping-skills exercises [77]. The lack of a treatment effect in this study may in part be attributable to the lack of involvement of a health care professional in the intervention delivery. Third, the mental health-focused interventions generally used robust outcome measures that corresponded closely to symptoms targeted by the intervention content. In contrast, the measures for the cancer studies were often measures of global well-being such as quality of life or social support. Such global indices may be influenced by many factors including treatment or disease stage which are beyond the realm of web-based intervention.
Mediators of effectiveness
Sociodemographic and condition-related mediators of treatment effect were largely ignored in the literature identified for this review. Given previous findings that patients of lower socioeconomic status were less likely to engage with web-based cancer support groups [87] and that high risk, lower educated groups were less likely to engage with Internet-delivered lifestyle advice [88], sociodemographic mediators of effectiveness are worthy of exploration. Although it is understandable that the primary concern of studies should be effectiveness for all participants, it is important in terms of Internal validity and equity to assess whether the intervention was equally effective across all study sub-groups. A number of studies appeared to have sufficient power to explore these issues but appeared not to do so [57, 59].
Variable effects have been identified in interventions for chronic conditions on condition-related outcomes according to sociodemographic characteristics, such as the effectiveness of smoking cessation support and cancer screening advice [89, 90]. It is quite likely that this may also occur in the delivery of psychosocial interventions. This important area deserves further consideration in order to assess whether effective interventions are equitable—i.e. appropriate and available for all who may require support.
Differential reach and adoption rates
The limited data on adoption suggested that use of web-based intervention was relatively high among enrolled study participants (70–95%) [58, 59, 61, 62, 66]. This compares favourably with adoption rates of less than 30% for many face-to-face psychosocial interventions [91, 92]. There was little evidence of a socioeconomic gradient in terms of intervention reach or adoption, primarily due to a lack of attention to these issues in the reviewed literature. However, one study [70] appeared to report somewhat lower recruitment rates at the hospitals that served disadvantaged populations. Therefore, issues of reach and adoption in relation to web-based approaches are a crucial area for further research. Web-based approaches increasingly have the capacity and flexibility to provide information in formats which incur lower literacy demands than do print-based media. Studies in which the relative reach, adoption, efficacy and cost-effectiveness of web-based interventions versus face-to-face or telephone intervention for vulnerable groups is explored, as noted by Tate et al. [93], are crucial in planning efficient and equitable approaches to providing psychosocial support to people with chronic illnesses.
Limitations
Although the review was based on a systematic search strategy, it is possible that not all publications addressing web-based interventions were identified. However, this seems unlikely based on the breadth and depth of literature identified in the current review. There was also substantial heterogeneity in the types of interventions and outcomes presented in the included studies, which meant that a meta-analysis could not be conducted. Although heterogeneity limits the ability to make specific comparative conclusions, a ‘broad brush’ review provides a useful overview of the range of web-based interventions available for common chronic conditions and insight into their general effectiveness. In order to determine which features of interventions are most effective, further methodologically rigorous studies are needed.
It should also be noted that only interventions conducted with adult participants were included in this review, limiting the ability to generalize the results of the review to children. Furthermore, studies in which peer support was the major intervention component were excluded, as peer support is thought to act via different mechanisms to professionally led and structured interventions [94]. Therefore, these results may not generalize to peer support-based studies.
Conclusion
This review highlights that the evidence for the effectiveness of web-based approaches is mixed. Although web-based interventions can be effective for reducing levels of psychological disturbance for some groups, there is insufficient evidence to conclude that a web-based approach is generally suitable for all patient groups and a variety of types of psychosocial support. Many of the included studies offered information-based interventions and low-intensity or unstructured support, which may have contributed to a lack of effectiveness in improving psychosocial outcomes. Further studies are needed to allow issues of intervention content to be compared in depth. Examining the effectiveness of web-based approaches for improving psychosocial health across a range of chronic illnesses is a particular strength of this review. If web-based approaches are to be offered en masse, head-to-head comparisons of reach, adoption and cost-effectiveness of web-based versus other options are required. These studies need to be sufficiently powered to make sub-group comparisons, particularly in relation to socioeconomically disadvantaged participants.
Funding
Infrastructure funding from the Hunter Medical Research Institute is gratefully acknowledged.
Conflict of interest statement
None declared.
References
- 1.Australian Institute of Health and Welfare. Risk Factors Contributing to Chronic Disease. Canberra: AIHW; 2012. [Google Scholar]
- 2.Australian Bureau of Statistics. Chronic Disease. 2010. Available at: http://www.abs.gov.au/AUSSTATS/abs@.nsf/Lookup/692C03405807CF0BCA25773700169C87. Accessed: 20 November 2012.
- 3.Centres for Disease Control and Prevention. Chronic Diseases and Health Promotion. 2009. Available at: http://www.cdc.gov/chronicdisease/overview/index.htm. Accessed: 20 November 2012.
- 4.Yach D, Hawkes C, Gould L, et al. The global burden of chronic diseases: overcoming impediments to prevention and control. JAMA. 2004;291:2616–22. doi: 10.1001/jama.291.21.2616. [DOI] [PubMed] [Google Scholar]
- 5.Daar AS, Singer PA, Leah Persad D, et al. Grand challenges in chronic non-communicable diseases. Nature. 2007;450:494–6. doi: 10.1038/450494a. [DOI] [PubMed] [Google Scholar]
- 6.Clarke D, Currie K. Depression, anxiety and their relationship with chronic diseases: a review of the epidemiology, risk and treatment evidence. Med J Aust. 2009;190:54–60. doi: 10.5694/j.1326-5377.2009.tb02471.x. [DOI] [PubMed] [Google Scholar]
- 7.Linden W, Vodermaier A, MacKenzie R, et al. Anxiety and depression after cancer diagnosis: prevalence rates by cancer type, gender, and age. J Affect Disord. 2012;141:343–51. doi: 10.1016/j.jad.2012.03.025. [DOI] [PubMed] [Google Scholar]
- 8.Lazarus RS, Folkman S. Stress, Appraisal, and Coping. New York: Springer Publishing Company; 1984. [Google Scholar]
- 9.Beyond Blue. Signs and Symptoms of Depression. 2011. Available at: http://www.beyondblue.org.au. Accessed: 23 May 2011.
- 10.Beyond Blue. Signs and Symptoms of Anxiety. 2011. Available at: http://www.beyondblue.org.au. Accessed: 23 May 2011.
- 11.Mitchell AJ, Chan M, Bhatti H, et al. Prevalence of depression, anxiety, and adjustment disorder in oncological, haematological, and palliative-care settings: a meta-analysis of 94 interview-based studies. Lancet Oncol. 2011;12:160–74. doi: 10.1016/S1470-2045(11)70002-X. [DOI] [PubMed] [Google Scholar]
- 12.Massie MJ. Prevalence of depression in patients with cancer. J Natl Cancer Inst Monogr. 2004;2004:57–71. doi: 10.1093/jncimonographs/lgh014. [DOI] [PubMed] [Google Scholar]
- 13.Li C, Ford E, Zhao G, et al. Association between diagnosed diabetes and serious psychological distress among U.S. adults: the Behavioral Risk Factor Surveillance System, 2007. Int J Public Health. 2009;54:43–51. doi: 10.1007/s00038-009-0006-1. [DOI] [PubMed] [Google Scholar]
- 14.Miller CK, Davis MS. The influential role of social support in diabetes management. Top Clin Nutr. 2005;20:157–65. [Google Scholar]
- 15.Australian Institute of Health and Welfare. Australia's Health 2010. Canberra: AIHW; 2010. [Google Scholar]
- 16.National Center for Health Statistics. Health, United States, 2010: With Special Feature on Death and Dying. Hyattsville, MD: National Center for Health Statistics; 2011. [PubMed] [Google Scholar]
- 17.Council of Australian Governments. National Action Plan on Mental Health 2006–2011. Canberra: Council of Australian Governments; 2006. [Google Scholar]
- 18.Glasgow RE, Vogt TM, Boles SM. Evaluating the public health impact of health promotion interventions: the RE-AIM framework. Am J Public Health. 1999;89:1322–7. doi: 10.2105/ajph.89.9.1322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Butler AC, Chapman JE, Forman EM, et al. The empirical status of cognitive-behavioral therapy: a review of meta-analyses. Clin Psychol Rev. 2006;26:17–31. doi: 10.1016/j.cpr.2005.07.003. [DOI] [PubMed] [Google Scholar]
- 20.Hunot V, Churchill R, Teixeira V, et al. Psychological therapies for generalised anxiety disorder. Cochrane Database Syst Rev. 2007:CD001848. doi: 10.1002/14651858.CD001848.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pfeiffer PN, Heisler M, Piette JD, et al. Efficacy of peer support interventions for depression: a meta-analysis. Gen Hosp Psychiatry. 2011;33:29–36. doi: 10.1016/j.genhosppsych.2010.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pull CB. Self-help Internet interventions for mental disorders. Curr Opin Psychiatry. 2006;19:50–3. doi: 10.1097/01.yco.0000198103.31155.73. [DOI] [PubMed] [Google Scholar]
- 23.Griffiths KM, Farrer L, Christensen H. The efficacy of Internet interventions for depression and anxiety disorders: a review of randomised controlled trials. Med J Aust. 2010;192:S4–11. doi: 10.5694/j.1326-5377.2010.tb03685.x. [DOI] [PubMed] [Google Scholar]
- 24.Klemm P, Bunnell D, Cullen M, et al. Online cancer support groups: a review of the research literature. Comput Inform Nurs. 2003;21:136–42. doi: 10.1097/00024665-200305000-00010. [DOI] [PubMed] [Google Scholar]
- 25.Finfgeld DL. Therapeutic groups online: the good, the bad, and the unknown. Issues Ment Health Nurs. 2000;21:241–55. doi: 10.1080/016128400248068. [DOI] [PubMed] [Google Scholar]
- 26.Anderson AS, Klemm P. The Internet: friend or foe when providing patient education? Clin J Oncol Nurs. 2008;12:55–63. doi: 10.1188/08.CJON.55-63. [DOI] [PubMed] [Google Scholar]
- 27.Griffiths F, Lindenmeyer A, Powell J, et al. Why are health care interventions delivered over the internet? A systematic review of the published literature. J Med Internet Res. 2006;8:e10. doi: 10.2196/jmir.8.2.e10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hesse BW, Nelson D, Kreps GL, et al. Trust and sources of health information: the impact of the Internet and its implications for health care providers: findings from the first health information national trends survey. Arch Intern Med. 2005;165:2618–24. doi: 10.1001/archinte.165.22.2618. [DOI] [PubMed] [Google Scholar]
- 29.Pew Internet & American Life Project. Health Topics. 2011. Available at: http://pewinternet.org/Reports/2011/HealthTopics/Part-1/59-of-adults.aspx. Accessed: 20 November 2012.
- 30.Murray E, Burns J, See Tai S, et al. Interactive health communication applications for people with chronic disease. Cochrane Database Syst Rev. 2005:CD004274. doi: 10.1002/14651858.CD004274.pub4. [DOI] [PubMed] [Google Scholar]
- 31.Wantland JD, Portillo JC, Holzemer LW, et al. The effectiveness of web-based vs. non-web-based interventions: a meta-analysis of behavioral change outcomes. J Med Internet Res. 2004;6:e40. doi: 10.2196/jmir.6.4.e40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Solomon MR. Information technology to support self-management in chronic care. Dis Manag Health Outcomes. 2008;16:391–401. [Google Scholar]
- 33.Australian Bureau of Statistics. 8146.0—Household Use of Information Technology, Australia, 2008–09. 2009. Available at: http://www.ausstats.abs.gov.au/Ausstats/subscriber.nsf/0/9B44779BD8AF6A9CCA25768D0021EEC3/$File/81460_2008-09.pdf. Accessed: 24 April 2013.
- 34.US Census Bureau. Current Population Survey (Appendix A) 2010. Available at: http://www.census.gov/population/www/socdemo/computer/2009.html. Accessed: 20 November 2012.
- 35.Curtin J. A Digital Divide in Rural and Regional AUSTRALIA? 2001. Available at: http://www.aph.gov.au/About_Parliament/Parliamentary_Departments/Parliamentary_Library/Publications_Archive/CIB/cib0102/02CIB01. Accessed: 20 November 2012.
- 36.Australian Bureau of Statistics. 8146.0.55.001—Patterns of Internet Access in Australia, 2006. 2007. Available at: http://www.abs.gov.au/AUSSTATS/abs@.nsf/ProductsbyCatalogue/3C0259A57BF969BFCA2573A10017B6BC. Accessed: 24 April 2013.
- 37.An LC, Betzner A, Schillo B, et al. The comparative effectiveness of clinic, work-site, phone, and Web-based tobacco treatment programs. Nicotine Tob Res. 2010;12:989–96. doi: 10.1093/ntr/ntq133. [DOI] [PubMed] [Google Scholar]
- 38.Richardson CR, Buis LR, Janney AW, et al. An online community improves adherence in an internet-mediated walking program. Part 1: results of a randomized controlled trial. J Med Internet Res. 2010;12:e71. doi: 10.2196/jmir.1338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Melville KM, Casey LM, Kavanagh DJ. Dropout from Internet-based treatment for psychological disorders. Br J Clin Psychol. 2010;49:455–71. doi: 10.1348/014466509X472138. [DOI] [PubMed] [Google Scholar]
- 40.Palmqvist B, Carlbring P, Andersson G. Internet-delivered treatments with or without therapist input: does the therapist factor have implications for efficacy and cost? Expert Rev Pharmacoecon Outcomes Res. 2007;7:291–7. doi: 10.1586/14737167.7.3.291. [DOI] [PubMed] [Google Scholar]
- 41.Griffiths KM, Christensen H. Review of randomised controlled trials of Internet interventions for mental disorders and related conditions. Clin Psychol. 2006;10:16–29. [Google Scholar]
- 42.Christensen H, Reynolds J, Griffiths KM. The use of e-health applications for anxiety and depression in young people: challenges and solutions. Early Interv Psychiatry. 2011;5:58–62. doi: 10.1111/j.1751-7893.2010.00242.x. [DOI] [PubMed] [Google Scholar]
- 43.Cochrane Effective Practice and Organisation of Care Review Group. Data Collection Checklist. Ottawa: Cochrane Effective Practice and Organisation of Care Group (EPOC); 2002. [Google Scholar]
- 44.Flay B, Biglan A, Boruch R, et al. Standards of evidence: criteria for efficacy, effectiveness and dissemination. Prev Sci. 2005;6:151–75. doi: 10.1007/s11121-005-5553-y. [DOI] [PubMed] [Google Scholar]
- 45.Mackinnon A, Griffiths KM, Christensen H, et al. Comparative randomised trial of online cognitive-behavioural therapy and an information website for depression: 12-month outcomes. Br J Psychiatry. 2008;192:130–4. doi: 10.1192/bjp.bp.106.032078. [DOI] [PubMed] [Google Scholar]
- 46.Christensen H, Leach LS, Barney L, et al. The effect of web based depression interventions on self reported help seeking: randomised controlled trial. BMC Psychiatry. 2006;6:13. doi: 10.1186/1471-244X-6-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Christensen H, Griffiths KM, Jorm AF. Delivering interventions for depression by using the internet: randomised controlled trial. Br Med J. 2004;328:265. doi: 10.1136/bmj.37945.566632.EE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Spek V, Cuijpers P, Nyklícek I, et al. One-year follow-up results of a randomized controlled clinical trial on internet-based cognitive behavioural therapy for subthreshold depression in people over 50 years. Psychol Med. 2008;38:635. doi: 10.1017/S0033291707002590. [DOI] [PubMed] [Google Scholar]
- 49.Spek V, Nyklicek I, Smits N, et al. Internet-based cognitive behavioural therapy for subthreshold depression in people over 50 years old: a randomized controlled clinical trial. Psychol Med. 2007;37:1797. doi: 10.1017/S0033291707000542. [DOI] [PubMed] [Google Scholar]
- 50.Barrera M, Jr, Glasgow RE, McKay HG, et al. Do Internet-based support interventions change perceptions of social support? an experimental trial of approaches for supporting diabetes self-management. Am J Community Psychol. 2002;30:637–54. doi: 10.1023/A:1016369114780. [DOI] [PubMed] [Google Scholar]
- 51.Bond G, Burr R, Wolf F, et al. The effects of a web-based intervention of psychosocial well-being among adults aged 60 and older with diabetes: a randomized trial. Diabetes Educ. 2010;36:446–56. doi: 10.1177/0145721710366758. [DOI] [PubMed] [Google Scholar]
- 52.Clarke G, Eubanks D, Reid E, et al. Overcoming depression on the Internet (ODIN) (2): a randomized trial of self-help depression skills program with reminders. J Med Internet Res. 2005;7:e16. doi: 10.2196/jmir.7.2.e16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Hoybye M, Dalton S, Deltour I, et al. Effect of Internet peer-support groups on psychosocial adjustment to cancer: a randomised study. Br J Cancer. 2010;102:1348–54. doi: 10.1038/sj.bjc.6605646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Kerr J, Patrick K, Norman G, et al. Randomized control trial of a behavioral intervention for overweight women: impact on depressive symptoms. Depress Anxiety. 2008;25:555–8. doi: 10.1002/da.20320. [DOI] [PubMed] [Google Scholar]
- 55.Kessler D, Lewis G, Kaur S, et al. Therapist-delivered Internet psychotherapy for depression in primary care: a randomised controlled trial. Lancet. 2009;374:628–34. doi: 10.1016/S0140-6736(09)61257-5. [DOI] [PubMed] [Google Scholar]
- 56.Knaevelsrud C, Maercker A. Internet-based treatment for PTSD reduces distress and facilitate the development of a strong therapeutic alliance: a randomised controlled clinical trial. BMC Psychiatry. 2007;7:13. doi: 10.1186/1471-244X-7-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Lorig KR, Ritter PL, Laurent DD, et al. Internet-based chronic disease self-management: a randomized trial. [Erratum appears in Med Care. 2007 Mar;45(3):276] Med Care. 2006;44:964–71. doi: 10.1097/01.mlr.0000233678.80203.c1. [DOI] [PubMed] [Google Scholar]
- 58.Meyer B, Berger T, Caspar F, et al. Effectiveness of a novel integrative online treatment for depression (Deprexis): randomized controlled trial. J Med Internet Res. 2009;11:e15. doi: 10.2196/jmir.1151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Roy-Byrne P, Craske M, Sullivan G. Delivery of evidence-based treatment for multiple anxiety disorders in primary care: a randomised controlled trial. J Am Med Assoc. 2010;303:1921–8. doi: 10.1001/jama.2010.608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Seligman ME, Schulman P, Tryon AM. Group prevention of depression and anxiety symptoms. Behav Res Ther. 2007;45:1111–26. doi: 10.1016/j.brat.2006.09.010. [DOI] [PubMed] [Google Scholar]
- 61.van Straten A, Cuijpers P, Smits N, et al. Effectiveness of a web-based self-help intervention for symptoms of depression, anxiety, and stress: randomized controlled trial. J Med Internet Res. 2008;10:e7. doi: 10.2196/jmir.954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Warmerdam L, van Straten A, Twisk J, et al. Internet-based treatment for adults with depressive symptoms: randomized controlled trial. J Med Internet Res. 2008;10:e44. doi: 10.2196/jmir.1094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Winzelberg AJ, Classen C, Alpers GW, et al. Evaluation of an internet support group for women with primary breast cancer. Cancer. 2003;97:1164–73. doi: 10.1002/cncr.11174. [DOI] [PubMed] [Google Scholar]
- 64.Carlbring P, Bohman S, Brunt S, et al. Remote treatment of panic disorder: a randomized trial of internet-based cognitive behavior therapy supplemented With telephone calls. Am J Psychiatry. 2006;163:2119–25. doi: 10.1176/ajp.2006.163.12.2119. [DOI] [PubMed] [Google Scholar]
- 65.Meglic M, Furlan M, Kuzmanic M, et al. Feasibility of an eHealth service to support collaborative depression care: results of a pilot study. J Med Internet Res. 2010;12:e63. doi: 10.2196/jmir.1510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.van Bastelaar KM, Pouwer F, Cuijpers P, et al. Web-based depression treatment for type 1 and type 2 diabetic patients: a randomized, controlled trial. Diabetes Care. 2011;34:320–5. doi: 10.2337/dc10-1248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Hawkins RP, Pingree S, Shaw B, et al. Mediating processes of two communication interventions for breast cancer patients. Patient Educ Couns. 2010;81(Suppl.):S48–53. doi: 10.1016/j.pec.2010.10.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Glasgow RE, Boles SM, McKay HG, et al. The D-Net diabetes self-management program: long-term implementation, outcomes, and generalization results. Prev Med. 2003;36:410–9. doi: 10.1016/s0091-7435(02)00056-7. [DOI] [PubMed] [Google Scholar]
- 69.Gustafson D, Hawkins R, McTavish F, et al. Internet-Based interactive support for cancer patients: are integrated systems better? J Commun. 2008;58:238. doi: 10.1111/j.1460-2466.2008.00383.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Gustafson D, Hawkins R, Pingree S, et al. Effect of computer support on younger women with breast cancer. J Gen Intern Med. 2001;16:435–45. doi: 10.1046/j.1525-1497.2001.016007435.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Brennan PF, Casper GR, Burke LJ, et al. Technology-enhanced practice for patients with chronic cardiac disease: home implementation and evaluation. Heart Lung. 2010;39:S34–46. doi: 10.1016/j.hrtlng.2010.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Berger T, Hohl E, Caspar F. Internet-based treatment for social phobia: a randomized controlled trial. J Clin Psychol. 2009;65:1021. doi: 10.1002/jclp.20603. [DOI] [PubMed] [Google Scholar]
- 73.Clarke G, Reid E, Eubanks D, et al. Overcoming depression on the Internet (ODIN): a randomized controlled trial of an Internet depression skills intervention program. J Med Internet Res. 2002;4:E14. doi: 10.2196/jmir.4.3.e14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Kiropoulos LA, Klein B, Austin DW, et al. Is internet-based CBT for panic disorder and agoraphobia as effective as face-to-face CBT? J Anxiety Disord. 2008;22:1273–84. doi: 10.1016/j.janxdis.2008.01.008. [DOI] [PubMed] [Google Scholar]
- 75.Liebreich T, Plotnikoff RC, Courneya KS, et al. Diabetes NetPLAY: a physical activity website and linked email counselling randomized intervention for individuals with type 2 diabetes. Int J Behav Nutr Phys Act. 2009;6:18. doi: 10.1186/1479-5868-6-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.McKay HG, King D, Eakin EG, et al. The diabetes network internet-based physical activity intervention: a randomized pilot study. Diabetes Care. 2001;24:1328–34. doi: 10.2337/diacare.24.8.1328. [DOI] [PubMed] [Google Scholar]
- 77.Owen JE, Klapow JC, Roth DL, et al. Randomized pilot of a self-guided internet coping group for women with early-stage breast cancer. Ann Behav Med. 2005;30:54–64. doi: 10.1207/s15324796abm3001_7. [DOI] [PubMed] [Google Scholar]
- 78.Patten SB. Prevention of depressive symptoms through the use of distance technologies. Psychiatr Serv. 2003;54:396–8. doi: 10.1176/appi.ps.54.3.396. [DOI] [PubMed] [Google Scholar]
- 79.Mailey EL, Wojcicki TR, Motl RW, et al. Internet-delivered physical activity intervention for college students with mental health disorders: a randomized pilot trial. Psychol Health Med. 2010;15:646–59. doi: 10.1080/13548506.2010.498894. [DOI] [PubMed] [Google Scholar]
- 80.Loiselle CG, Edgar L, Batist G, et al. The impact of a multimedia informational intervention on psychosocial adjustment among individuals with newly diagnosed breast or prostate cancer: a feasibility study. Patient Educ Couns. 2010;80:48–55. doi: 10.1016/j.pec.2009.09.026. [DOI] [PubMed] [Google Scholar]
- 81.Hedman E, Andersson G, Ljotsson B, et al. Internet-based cognitive behavior therapy vs. cognitive behavioral group therapy for social anxiety disorder: a randomized controlled non-inferiority trial. PLoS ONE. 2011;6:e18001. doi: 10.1371/journal.pone.0018001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Quinn CC, Shardell MD, Terrin ML, et al. Cluster-randomized trial of a mobile phone personalized behavioral intervention for blood glucose control. Diabetes Care. 2011;34:1934–42. doi: 10.2337/dc11-0366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Clarke G, Kelleher C, Hornbrook M, et al. Randomized effectiveness trial of an Internet, pure self-help, cognitive behavioral intervention for depressive symptoms in young adults. Cogn Behav Ther. 2009;38:222–34. doi: 10.1080/16506070802675353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Pok Ja O, Soo Hyun K. Effects of a brief psychosocial intervention in patients with cancer receiving adjuvant therapy. Oncol Nurs Forum. 2010;37:E98–104. doi: 10.1188/10.ONF.E98-E104. [DOI] [PubMed] [Google Scholar]
- 85.Boesen EH, Karlsen R, Christensen J, et al. Psychosocial group intervention for patients with primary breast cancer: a randomised trial. Eur J Cancer. 2011;47:1363–72. doi: 10.1016/j.ejca.2011.01.002. [DOI] [PubMed] [Google Scholar]
- 86.Hofmann SG, Smits JAJ. Cognitive-behavioral therapy for adult anxiety disorders: a meta-analysis of randomized placebo-controlled trials. J Clin Psychiatry. 2008;69:621. doi: 10.4088/jcp.v69n0415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Høybye M, Dalton S, Christensen J, et al. Social and psychological determinants of participation in internet-based cancer support groups. Support Care Cancer. 2010;18:553–60. doi: 10.1007/s00520-009-0683-6. [DOI] [PubMed] [Google Scholar]
- 88.Brouwer W, Oenema A, Raat H, et al. Characteristics of visitors and revisitors to an Internet-delivered computer-tailored lifestyle intervention implemented for use by the general public. Health Educ Res. 2010;25:585–95. doi: 10.1093/her/cyp063. [DOI] [PubMed] [Google Scholar]
- 89.Hiscock R, Judge K, Bauld L. Social inequalities in quitting smoking: what factors mediate the relationship between socioeconomic position and smoking cessation? J Public Health. 2011;33:39–47. doi: 10.1093/pubmed/fdq097. [DOI] [PubMed] [Google Scholar]
- 90.Kotz D, West R. Explaining the social gradient in smoking cessation: it's not in the trying, but in the succeeding. Tob Control. 2009;18:43–6. doi: 10.1136/tc.2008.025981. [DOI] [PubMed] [Google Scholar]
- 91.Eakin EG, Strycker LA. Awareness and barriers to use of cancer support and information resources by HMO patients with breast, prostate, or colon cancer: patient and provider perspectives. Psychooncology. 2001;10:103–13. doi: 10.1002/pon.500. [DOI] [PubMed] [Google Scholar]
- 92.Pascoe S, Edelman S, Kidman A. Prevalence of psychological distress and use of support services by cancer patients at Sydney hospitals. Aust N Z J Psychiatry. 2000;34:785–91. doi: 10.1080/j.1440-1614.2000.00817.x. [DOI] [PubMed] [Google Scholar]
- 93.Tate D, Finkelstein E, Khavjou O, et al. Cost effectiveness of internet interventions: review and recommendations. Ann Behav Med. 2009;38:40–5. doi: 10.1007/s12160-009-9131-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Campbell HS, Phaneuf MR, Deane K. Cancer peer support programs—do they work? Patient Educ Couns. 2004;55:3–15. doi: 10.1016/j.pec.2003.10.001. [DOI] [PubMed] [Google Scholar]