Abstract
Intestinal Entamoeba Histolytica infection in the UK is rare but it can lead to colitis, abscess formation, colonic perforation and rarely amoeboma. Although most patients are asymptomatic, it can present with a wide range of gastrointestinal symptoms depending on the phase of the infection. We present a case of amoebic colitis that caused diagnostic uncertainty by mimicking a colonic carcinoma.
INTRODUCTION
Amoebiasis is an infectious disease caused by Entamoeba Histolytica, and is the second leading cause of death from parasitic disease worldwide (1). It is commonly acquired by ingestion of contaminated food or water and is therefore endemic in developing countries with poor sanitation. Ten percent of the world’s population become infected, 90% of which are asymptomatic (2). Symptomatic patients present with fever, abdominal pain and bloody diarrhoea. We present a case of amoebic colitis that caused diagnostic confusion by mimicking a colonic carcinoma.
CASE REPORT
A 63 year-old woman presented to hospital with a 5 weeks’ history of colicky right upper quadrant abdominal pain, abdominal distension and constipation. She also reported fever and night sweats. There was no history of recent foreign travel, but she had travelled to the Middle East 6 months prior to admission. She had had a normal colonoscopy performed for a change in bowel habit 2 years previously, and an abdominal ultrasound scan performed at the onset of her symptoms was also normal, apart from a 1.5cm cyst in the liver.
On examination she was dehydrated and was tender in the right iliac fossa and right upper quadrant. Her temperature was 38.4°C. She had a raised white blood cell count (13.4 10*9/L) and CRP (310mg/L), but all other blood tests were within normal limits.
Her chest x-ray showed blunting of the left costophrenic angle and her abdominal x-ray showed multiple dilated small bowel loops with faecal loading in the descending colon. She was started on intravenous Tazobactam and Piperacillin and a CT scan of her abdomen and pelvis was performed. This showed a low attenuation lesion in the left lobe of the liver with surrounding inflammation consistent with a liver abscess (Figure 1), as well as wall thickening in the ascending colon that extended into the caecum and terminal ileum (Figure 2).
Figure 1.
CT image demonstrating low attenuation lesion in the left lobe of the liver with surrounding inflammation consistent with a liver abscess
Figure 2.
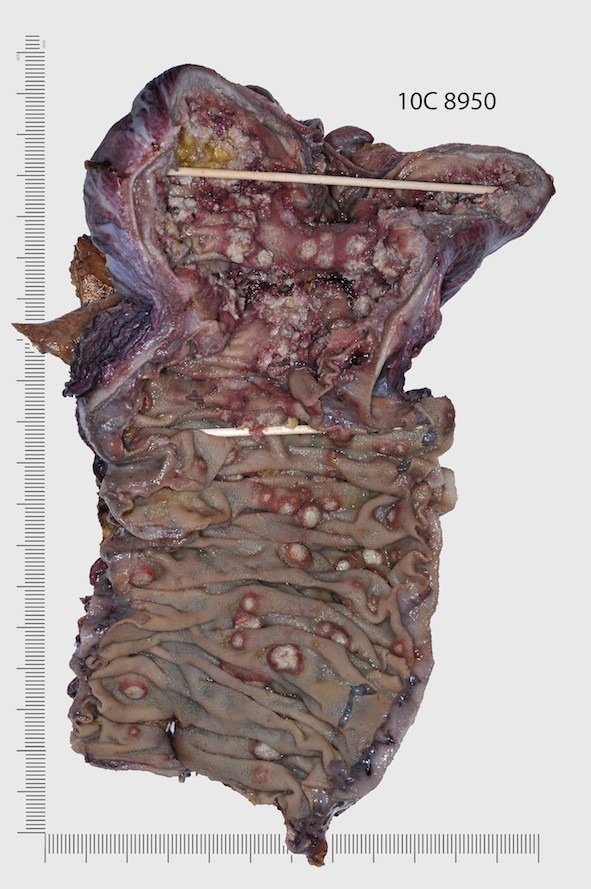
Gross appearance of caecum and ascending colon showing ulcerated and polypoidal amoebic lesions mimicking colonic mucosal tumours
The differential diagnosis at this stage included appendicitis, colonic Crohn’s disease, and colorectal neoplasia. Due to the possibility of colonic malignancy, it was decided to proceed to surgical resection. At laparotomy, an inflammatory mass involving the right colon was confirmed, and so the patient underwent a right hemicolectomy and drainage of liver abscess. She was continued on postoperative antibiotics and apart from a short period of paralytic ileus, she progressed well. She was discharged 9 days postoperatively.
Diagnosis of amoebic colitis was made by pathological examination of the resection specimen. Macroscopically, there were inflammatory exudates on the surface of the caecal and terminal ileal mucosa, as well as thickening and ulceration in the caecum. There were also multiple raised ulcerated lesions in the ascending colon (Figure 3). Microscopically, necrotic and haemorrhagic material was noted, with the base of the ulcers heavily infiltrated with inflammatory material involving the mucosa and submucosa. There were also amoebae parasites present within the inflammatory cellular exudates in most of the ulcers examined microscopically, but there was no granuloma formation, dysplasia or malignancy seen. In addition, serological testing was positive for anti-amoebic antibodies.
Figure 3.
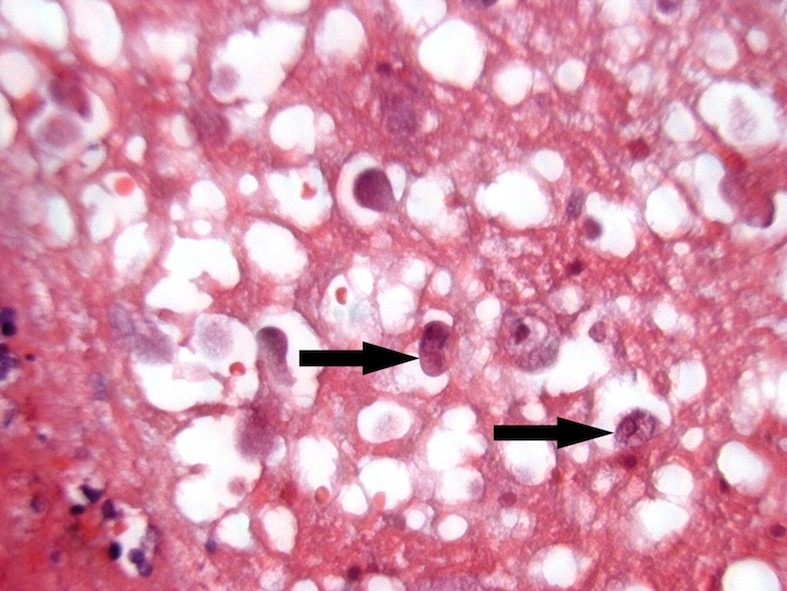
H&E stained histological section of amoebic abscess in the colonic wall demonstrating Entamoeba Histolitica parasites (arrowed).
DISCUSSION
Patients with intestinal amoebiasis are usually asymptomatic, but it can lead to colitis, abscess formation, perforation and rarely a tumour-like mass in the colon termed an amoeboma. Symptoms are dependent on the phase of infection. Initially abdominal pain and diarrhoea predominate, with bloody diarrhoea marking a progression to colitis that typically involves the caecum, ascending or sigmoid colon. An amoeboma is suggested by pain and swelling in the right iliac fossa, or symptoms of bowel obstruction. The most common extraintestinal manifestation of amoebiasis is liver abscess, due to parasites gaining entry into the portal circulation. This causes weight loss, right upper quadrant pain and fever.
There were 110 reported cases of Entamoeba Histolytica infection in England and Wales in 2009 (3). It occurs most commonly in patients aged 15-44 years. There is usually a history of recent travel to an endemic area. In the present case, the patient did not report a significant recent travel history, nor symptoms of diarrhoea. It is likely she had previously travelled to an endemic region and had developed an asymptomatic carrier state.
The typical features of amoebic colitis on CT are flask shaped ulcers with intramural dissection, whereas amoebic liver abscess typically causes well rounded, low density lesions with a clear fluid level. Amoeboma formation usually shows a localised hyperplastic granulomatous reaction forming an inflammatory mass that macroscopically resembles colon cancer. However, the association of colonic mass and liver abscess suggests an inflammatory rather than neoplastic aetiology, as there are few reports of abscess formation within colorectal liver metastases.
Serology aids the diagnosis of amoebiasis, being positive in 95% patients with amoeboma or hepatic amoebiasis, but only 60% in patients with amoebic colitis(4).
Treatment with metronidazole is effective, even in cases of amoeboma. Diloxanide furoate is given as a 10 day course in addition to eliminate luminal cysts. Surgery is only used when medical therapy fails, in rupture of liver abscess, or when there is diagnostic uncertainty.
This case highlights the diagnostic uncertainty that may occur in patients with amoebic colitis due to its ability to mimic colonic carcinoma, particularly if there is no definite recent history of travel to an endemic area. It highlights the importance of good history taking, in particular a thorough travel history, in patients with unusual intra-abdominal infections. Colonic resection is indicated when neoplasia cannot be excluded.
REFERENCES
- 1.Stanley SL., Jr Amoebiasis. Lancet. 2003; 361(9362): 1025–34 [DOI] [PubMed] [Google Scholar]
- 2.Pelaez M, Villazon A, Sieres Zaraboso R. Amebic perforation of the colon. Dis Colon Rectum. 1966; 9(5): 356–62 [DOI] [PubMed] [Google Scholar]
- 3.Ying K-S, Chan L-P, Wu S-H, Wu M-J, Chang T-Y, Lee C-H. CT Findings of Fulminant Amebic Colitis: a case report. Chin J Radiol. 2008; 33: 205–10 [Google Scholar]
- 4.Van Hal SJ, Stark DJ, Fotedar R, Marriott D, Ellis JT, Harkness JL. Amoebiasis: current status in Australia. Med J Aust. 2007; 186(8): 412–6 [DOI] [PubMed] [Google Scholar]



