Abstract
Child development may be subject to forms of motor, physical, cognitive and self-representation impairments when complex congenital heart disease (CHD) occurs. In some cases, inadequacy of both self-representation as well as the family system are displayed. It seems to be important to search the likely internal and external resources of the CHD child, and the possible connections among such resources, which may help him/her to manage his/her own risk condition. The research project inquires the possible resources related to the self-representation and self-esteem levels of the CHD child, and those related to maternal self-perception as competent mothers. A group of 25 children (mean age = 10.2; SD=1.8) suffering from specific forms of CHD, and a group made up of their relative mothers (mean age = 38.2; SD=5) were studied. The tools used were the Human Figure Drawing, to investigate child body-related self-representation; the TMA scale (Self-esteem Multidimensional Test), to investigate the child's self-esteem; and the Q-sort questionnaire, to assess how mothers perceived their maternal competence. Data concerning the likely correlations between the child's self-representation and the maternal role competence show [that] positive correlations between some indicators of maternal competence, specific aspects of CHD children's self-representation (mothers' emotional coping and children's self-image adequacy) and self-esteem (mothers' emotional scaffolding and children's self-esteem at an emotional level). By detecting the occurrence of specific correlations among resources of both child and mother, the study provides cardiologists with information that is useful for building a relationship with the families concerned, which would seem to enhance the quality of the process of the cure itself.
Key words: children's self-representation, children's self-esteem, mothers' perception of parental competence, developmental resources.
Introduction
Several European and International studies on the intricacy of paediatric conditions related to complex congenital heart disease (CHD) have detected impairments concerning the levels of motor and physical,1–3 as well as the cognitive development,4–6 the child's self-representation,7–9 and his/her interaction with the real-world.8 Such studies have also detected forms of psychological functioning disorder in each parent (e.g. inadequate perception of parental competence) and in the whole family system (e.g. entanglement among family members).10–15 The traditional deficit-centred model, however, is now almost obsolete,16 whereas nowadays models tend to focus on the impairments as well as on the possible child developmental resources and to parental representations, competences, abilities, etc., which are resources for managing the risk conditions of the mother or the father of a CHD child.17 Such parental resources could be factors of external protection to warrant child development.18 It has been stressed that CHD child adjustment is not often related to medical severity but to a distinct characteristic of the child's caregiver - that is, for example, how the mother perceives herself, her child, the pathology and the child's relation to it.19,20
To be more precise, this study has gone beyond exclusively focusing on specific resources of the CHD child and his primary caregivers - mothers in this case, and aims at exploring the relation between these resources which could facilitate the process of adjustment to disease and that of the development of both child and mother.10,21–25 The idea to focus on the above mentioned relation was inspired by the literature of Development Psychology and Social Psychology which highlights the mutual nature of mother-child interactions and claims that parents and children influence each other in a reciprocal manner.26–28,17 Some variables characterizing the child, such as his/her temperament, self-representation, skilfulness, etc., may affect the parenting practices.27,29,30 and some studies have even shown a chronic pathology which has seriously affected the parenting.28,31 Similarly, distinct variables of parental functioning, such as the perception and representation of both self and child, may in turn influence the emotional, cognitive and relational child development, as well as his/her behaviour, representations and experiences.27,29
In the light of these considerations, the study also focuses on the CHD child's internal variables, either impaired or as factor resources, related to body and self-esteem self-representation. The child's own perception of his/her body together with high levels of self-esteem may positively affect the quality of the developmental path of the child, who most likely will be more self-determined and adaptive while facing the chronic disease.32
A hierarchic and multidimensional model,33,34 which detects different interconnected dimensions such as the interpersonal, emotional, body-related and environmental mastery ones, has been adopted to analyse the child's self-esteem. In detail, the dimension of interpersonal relationships refers to how a child values interpersonal and socio-relational relationships with his/her peer group and adults; the dimension of environmental mastery is concerned with the ability of controlling and mastering the events of one's life as well as managing the surrounding environment; the dimension of emotionality is related to the ability of observing and analysing one's personal emotions as well as controlling and managing the negative ones; the dimension of body-related experiences refers to the perception of body image and the evaluation of one's personal abilities and physical performance.33,34 Finally, it needs to be pointed out that the model of self-esteem adopted by the study considers such a psychological dimension as a type of behavioural reaction. The evaluation made by an individual about his past behaviours and experiences, taking into account his/her individual achievements and failures, as well as strengthening individual events and how the others reacted to his/her actions and interacted with him/her. In other words, self-evaluation is based on information from both a personal as well as from other people's perspectives.
The reading model used for this study deals with both quality and quantity levels of body-related self-representation.35 With regard to quality, the analysed indicators of self-representation were adequacy of body image, which was assessed through the observance of the child's graphic representation of his/her body dimensions and proportions; the colour the child chose to draw his/her complexion and body proportion; and the integrity of his/her self-image, in terms of symmetry and dynamism of the human figure which they drew with a steady tract.
With regard to quantity the indicator was the children's cognitive maturity that refers to the concrete manifestation of graphic elements that derives from the activation of perceptive, spatial, logical and abstract processes.
Considering parents as external child's resources the mothers' perception of their parental competence is also assessed. This dimension of parental functioning is relevant since it is a perception that strongly defines the quality of children's care and reveals the capability of facing difficulties arisen from the children's disease.36,24,20 The reading model used in this study defines parentalness as active during a specific development period of the child, completing the sense of generativity with its functions.36,37 The three reference factors of maternal competence are:
Coping (A factor) refers to the mother's cognitive and emotional efforts to meet the needs arisen from the child's chronic disease to recognize, self-regulate and control emotions as well as the capability to redesign, at a cognitive level, the critical events related to child's health condition.
Scaffolding (B factor) refers to the maternal capability to support, steer and guide the child, to her ability to activate framing, building patterns and behavioural models in the relationships with her child.37–39 It is also the mother's willingness to emotionally support the child in his/her attempt to be self-determined,40 and to develop the ability to mediate with his/her environment (family, hospital, peer group, etc.).
Caregiving (C factor) refers to the maternal capability of being responsive, of providing an appropriate cure, and adjusting the mother's own reactions according to the child's developmental needs.
The correlations among the indicators of maternal competence (coping, scaffolding and caregiving), indicators of representation of the body-related self (self-image adequacy, body integrity, cognitive maturity) and those of the CHD child's self-esteem (interpersonal, body-related, emotional and environmental mastery) have been verified.
Materials and Methods
Participants
The study has been performed on a group of 25 children (mean age = 10.2; SD=1.8; range: 6–13 years), who suffer from different forms of CHD (Table 1), and a group of 25 relative mothers (mean age = 38.2; SD=5).
Table 1. Children sample: typologies of complex congenital heart disease.
| Frequency | % | |
|---|---|---|
| Hypertrophic cardiomiopathy | 5 | 20 |
| Aortic coarctation | 4 | 16 |
| Ventricle defect | 4 | 16 |
| Aortic valve stenosis | 3 | 12 |
| Fallot's tetralogy | 9 | 36 |
| Total | 25 | 100 |
The eligible participants were collected within a unit of the Pediatric Cardiology of Catania (Italy), according to the following criteria: children not younger than 8 years (minimum age required to administer the planned tools) and not older than 13; no serious neurological sequelae. The 25 child/mother pairs were selected among 40 pairs in the two Units during the 6 months of the research.
The study was accomplished in accordance with the ethical research guidelines, established by the Declaration of Helsinki in 1964. The participants gave their consent after they had been informed about the study protocol.
Measures and procedures
The following tools were administered to children/adolescents:
The Human Figure Drawing Test (HFDT),35 which is a projective paper-and-pencil test aimed at exploring the body-related self. It allows the study of both quality (self-image adequacy and body-related image integrity) and cognitive maturity (I.Q. maturity) evaluations. The procedure of marking the test includes the analysis of the graphic elements of the drawing that, according to the reference guide, would show the manifestation of body-related image adequacy and integrity. Each drawing comes with a marking grid designed using some descriptors related to the different graphic elements. The acceptance criteria established to detect the adequacy and integrity of the body-related image level, were: the expected indicators had to be present at a medium level, when 50% of the reference descriptors were detected; at a medium-low level, when less than 50% of the reference descriptors were detected; at a medium-high level, when more than 50% of the reference descriptors were detected; and they had to be absent when none of the descriptors were detected. A level was attributed to each indicator per child involved in the study (self-image adequacy, body-related integrity, I.Q. maturity); and the percentage frequency was calculated for each indicator.
The T.M.A. scale (Italian version of MSCS-Multidimensional Self-Concept Scale) is a validated and standardised questionnaire for the evaluation of distinct components of self-esteem.34 It consists of six 25-item scales: the interpersonal, school success, emotional and family life, body-related and environmental mastery scales. The child is invited to express his/her agreement to a number of statements and to indicate how true s/he considers each statement for him/herself. The answers correspond to a 4-mark Lykert scale (totally true; true; untrue; definitely untrue). A gross total of each scale is obtained by adding up the scores of the test. Each gross total, in its turn, is added up to obtain a global gross total of the child's self-esteem. Hence, through the comparison of the normative scores of TMA, the standard scores are calculated for each scale and for the total scale referring to self-esteem. Finally, as implied by the procedure of the test, the standard scores of each child, concerning both individual and global scales, are interpreted according to the range of the standard scores of the standardization sample in order to detect the level of self-esteem of the sample of the research (over 135 = extremely positive self-esteem; 126 to 135 = very positive self-esteem; 116 to 125 = slightly positive self-esteem; 86 to 115 = standard self-esteem; 76 to 85 = slightly negative self-esteem; 66 to 75= very negative self-esteem; under 66= extremely negative self-esteem).
The T.M.A. has excellent psychometric characteristics: a high level of liability (Cronbach's α of each scale is >0.80), and a low standard error of measurement (SEm<3.70). During a previous application of the tool during a pilot study on hospitalized children, it was decided not to administer two of the six scales (school success and family life), following the standard procedures and directions of the manual in question. It was also decided to eliminate some specific items considered not suitable for sick and hospitalized children, as they were a potential source of extreme emotional stressitem n. 47 of the scale of the environmental mastery; items n. 136, 142 and 143 of the scale of body-related experiences. Regarding the correction of the protocols and the counting of the partial and total scores, due to the elimination of the two scales and some items, some calculation expedients planned by the standardized procedures of the tool were applied.34
The Q-Sort on parental competence during the children's pathology questionnaire was given to mothers.36 This is a self-observation technique,41–44 designed as a Q-set of 90 different ways of behaviour related to the factors of the parental competence model. It consists of 40 items for coping - the A factor, subdivided in 20 items for the emotional coping (A1) and 20 for the cognitive one (A2); 30 items for scaffolding - the B factor, subdivided in 10 items for the emotional scaffolding (B1), 10 items for the cognitive one (B2) and the other 10 for the rational scaffolding (B3); 20 items for caregiving - the C factor, subdivided into 10 items related to different ways of behaviour that define the responsivity and 10 items that define the ability of adjustment to the children's developmental needs. The content of the questionnaire was validated through the technique of judges,45 while the competence criteria, to which the profiles of each subject undergoing the Q-sort was compared, was defined by the contributions of psychologists with experience in parenting and parental competence research and intervention.36 The coefficient of Cronbach's α was calculated in order to control the agreement level between the judges and the internal consistency of the competence criteria score, which is the outcome of the mean of profiles provided by judges (0.79).
With regard to the administration procedures, each mother involved in the research project was given a self-assessment form which divided the 90 items into 9 groups.46 She was then asked to identify to which degree her behaviour towards the child corresponded to the behaviour specified in the self-assessment survey. The items were collected and put into order using a 9-score Lykert scale ranging from item n.1: very different ways of behaviour to item n.9: very similar ways of behaviour. Each item received the score of the group with which the mother had decided to couple, and all scores were added up to obtain the total score of each factor of maternal competence.
Statistical analyses
The data were analysed using the statistical software SPSS V.10. Some data collected by the HFDT and the Q-sort questionnaire underwent both descriptive statistics and non-parametric tests (Spearman's ρ, Friedman's test, Bravais-Pearson's ρ), because they did not meet the requirements of the parametrical statistics (ordinal measurement scale). To be more precise, Spearman's ρ was calculated to detect the possible correlations between the indicators of the child's body representation (self-image adequacy, body integrity and cognitive maturity) and the indicators of the maternal competence; between the indicators of maternal competence and the child's self-esteem. Friedman's test was used to detect possible statistically significant differences among the scales of the TMA, the various indicators of the child's body-related self and the several factors of maternal competence measured by the Q-sort. Bravais-Pearson's ρ was calculated to compare the level of perceived maternal competence to the competence criteria obtained with the help of the judges technique.
Results
The data concerning the child's body-related self-representation (outcomes of the HFDT) show an important developmental resource, such as a quite standard cognitive maturity I.Q. (44% of all participants) and, in some cases, above standard (28% of all participants) (Figure 1). Other data show remarkable impairments in relation to self-image adequacy with scores at medium-low level and low level. 36% of all participants scored a medium-low level and 28% a low level (Figure 2). The scores of the sample related to body integrity are at a medium level of 36% and at a low level of 28% (Figure 3).
Figure 1.
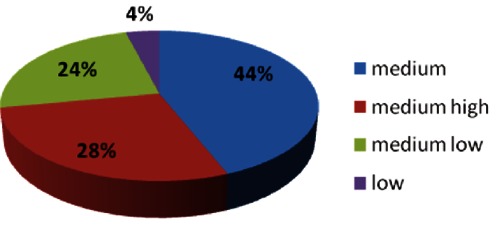
Children's body-related self-representation - level of Cognitive Maturity I.Q.
Figure 2.
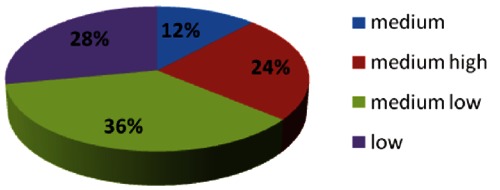
Children's body-related self-representation - level of Self-Image Adequacy (HFDT).
Figure 3.
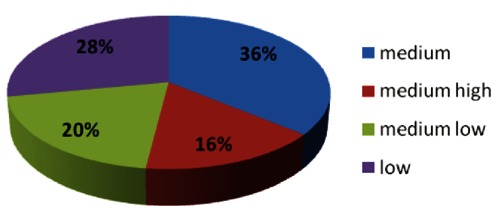
Children's body-related self-representation - level of Body Integrity (HFDT).
In every scale, the data related to the CHD child's self-esteem (results of the T.M.A.) are mostly of a standard level. Friedman's test shows the absence of statistically significant differences among the four scales used in this study, though the dimension of interpersonal relationship self-esteem and body-related self-esteem has scored a higher percentage (Table 2). The descriptive analysis of the data of the Q-sort (Table 3) shows that the mother perceives herself primarily in terms of both cognitive (A2: mean=93.72, SD=11.01) and emotional (A1: mean=85.32, SD=13.44) coping; secondly, in terms of caregiving related to responsivity (C2: mean=56.9, SD=8.2) and adjustment of her own reactions to the child's developmental needs (C1: mean=53.8, SD=8.4); finally, in terms of the three levels of scaffolding; the cognitive (B1: mean=51.1, SD=5.9), the emotional (B2: mean=52.7, SD=5.9) and the relational (B3: mean=48.6, SD=0). Such data are confirmed by the comparison among different indicators of maternal competence, performed by means of Friedman's test (Table 4), which detected a statistically relevant difference (χ2=101.04, df=6; P=0.01).
Table 2. Self-esteem scales (descriptives statistics and Friedman's test).
| Self-esteem scales | Mean | Standard deviation | Mean rank |
| Interpersonal relationship | 78.16 | 9.43 | 3.12 |
| Environmental mastery | 75.16 | 8.35 | 2.22 |
| Emotionality | 75.24 | 7.36 | 2.26 |
| Body perception | 76.24 | 8.43 | 2.40 |
Friedman's test: χ2: 8.11 - Df: 3 Asymptotic significance: 0.50.
Table 3. Indicators of maternal competence (Q-sort) (N=25).
| Indicators of maternal competence | Mean | Standard deviation |
| A1. emotional coping | 85.32 | 13.44 |
| A2. cognitive coping | 93.72 | 11.01 |
| B1. cognitive scaffolding | 51.16 | 6.34 |
| B2. emotional scaffolding | 52.72 | 5.95 |
| B3. relational scaffolding | 48.68 | 9.78 |
| C1. adjustment to child's needs | 53.80 | 8.49 |
| C2. responsivity | 56.96 | 8.22 |
Table 4. Differences among the indicators of maternal competence (Q-Sort) (Friedman's test) (N=25).
| Indicators of maternal competence | Mean rank |
| A1. emotional coping | 6.30 |
| A2. cognitive coping | 6.68 |
| B1. cognitive scaffolding | 2.60 |
| B2 emotional scaffolding | 2.98 |
| B3. relational scaffolding | 2.32 |
| C1. adjustment to child's needs | 3.36 |
| C2. responsivity | 3.76 |
Friedman's test: Chi-Square: 101.042 - Df: 6. Asymp. Sig. 0.001.
With respect to the data concerning the mother's perception of parental competence, the data obtained through the comparison with the maternal competence criteria (test Pearson's ρ), show that most mothers perceive themselves as not very competent, even if their scores were not always low. Only a few perceived themselves as incompetent (Table 5).
Table 5. Mothers'perception of parental competence (Q-Sort): comparison with the maternal competence criteria (test Pearson's ρ).
| Mothers | Pearson's r | Maternal competence's level | Mothers | Pearson's r | Maternal competence's level |
| 1 | 0.603** | High competence | 14 | 0.229* | Low competence |
| 2 | 0.599** | High competence | 15 | 0.460** | Low competence |
| 3 | 0.338** | Low competence | 16 | 0.387** | Low competence |
| 4 | 0.564** | High competence | 17 | 0.038 | Low competence |
| 5 | 0.024 | Low competence | 18 | 0.145 | Low competence |
| 6 | -0.114 | Incompetence | 19 | 0.389** | Low competence |
| 7 | 0.487** | Low competence | 20 | 0.628** | High competence |
| 8 | 0.613** | High competence | 21 | 0.420** | Low competence |
| 9 | 0.565** | High competence | 22 | 0.050 | Low competence |
| 10 | 0.318** | Low competence | 23 | 0.444** | Low competence |
| 11 | 0.628** | High competence | 24 | 0.373** | Low competence |
| 12 | 0.439** | Low competence | 25 | 0.050 | Low competence |
| 13 | 0.721** | High competence |
P<0.05,
P<0.01
The data concerning the correlations between the child's self-representation and maternal competence show that the positive correlations between some indicators of maternal competence and some aspects of the CHD child's self-representation (Table 6) and self-esteem (Table 7) would seem to be useful resources to the child's development. There is a statistically significant positive correlation between the mother's emotional coping (A1 factor of maternal competence) and the child's self-image adequacy (rho=0.44, P<0.01), and between the mother's emotional scaffolding (B1 factor of maternal competence) and the child's self-esteem at emotional level (rho=0.34, P<0.05). The data also show statistically significant negative correlations between the mother's cognitive scaffolding (B2 factor of maternal competence) and the child's body-related self-esteem (rho=−0.50, P<0.01), and between the mother's relational scaffolding (B3 of maternal competence) and the child's self-esteem related to personal competence (rho=−0.52, P<0.01).
Table 6. Correlations between indicators of maternal competence (Q-Sort) and indicators of CHD children's self-representation (Spearman's r Coefficient) (N=25).
| Indicators of maternal competence (Q-Sort) | |||||||
|---|---|---|---|---|---|---|---|
| Indicators of CHD | |||||||
| children's self-representation | A1 | A2 | B1 | B2 | B3 | C1 | C2 |
| Adequacy of body image | 0.43* | 0.11 | −0.18 | −0.25 | −0.07 | −0.31 | −0.20 |
| Integrity of self-image | 0.25 | 0.10 | −0.02 | −0.16 | 0.014** | −0.18 | −0.16 |
| Cognitive maturity | −0.11 | −0.17 | −0.09 | 0.35 | 0.06 | 0.10 | 0.14 |
P<0.05
P<0.01. A1 – emotional coping ; A2 – cognitive coping; B1 – cognitive scaffolding; B2 – emotional scaffolding; B3 – relational scaffolding; C1 – adjustment to child's needs; C2 – responsivity.
Table 7. Correlations between indicators of maternal competence (Q-Sort) and indicators of CHD children's self-esteem (T.M.A) (Spearman's r Coefficient) (N=25).
| Indicators of maternal competence (Q-Sort) | |||||||
|---|---|---|---|---|---|---|---|
| Indicators of CHD | |||||||
| children's self-representation | A1 | A2 | B1 | B2 | B3 | C1 | C2 |
| Interpersonal relationship | −0.019 | 0.26 | −0.09 | −0.08 | −0.26 | 0.10 | 0.15 |
| Environmental mastery | 0.14 | 0.28 | 0.11 | −0.042 | −0.54** | 0.12 | −0.14 |
| Emotionality | 0.19 | 0.088 | 0.34* | −0.18 | −0.33 | −0.05 | −0.19 |
| Body perception | 0.28 | 0.19 | −0.10 | −0.51** | −0.21 | 0.090 | 0.077 |
P<0.05
P<0.01. A1 – emotional coping ; A2 – cognitive coping; B1 – cognitive scaffolding; B2 – emotional scaffolding; B3 – relational scaffolding; C1 – adjustment to child's needs; C2 – responsivity
Discussion and Conclusions
This study examined the self-representation of children suffering from CHD, how the mothers perceived their maternal competence and the relationship between these factors. With regard to the results about some of the child's and mother's resources, and the related variables analysed in the study, the data concerning the body-related self-representation are remarkable. The presence of a standard maturity I.Q. shows that the CHD child, notwithstanding the impairments brought on by pathology, has got cognitive abilities which enable him/her to redefine his/her self-image and face the risk condition. Abstract reasoning enables them to perceive themselves not in terms of a sick body, but rather in terms of a child with a potentially able body; perceptive organization allows the child to redefine the representation of his/her own body and his/her interaction with the world. These results seem to be a confirmation of studies which have detected the absence of considerable differences between both the CHD and the healthy child in terms of cognitive abilities,31 whereas, at cognitive and self-representation levels, they contrast other studies which have recorded the presence of remarkable impairments in the CHD child.14,47–50 Further studies in this field are required. The findings which refer to the impairment of the body-related self-image support those of other studies in that field.13,51
The self-esteem resources have scored an average percentage in each scale of the TMA. These data show the ability to create bonds, exchanges, interactions and the search for alternatives; the ability to recognize and control emotions; environmental mastery; standard body perception. The latter, which is more present in this study than it is in the data of Royer, is a perception concerning strength, physical energy and self-appreciation only in terms of aesthetics. These data contradict other studies that have recorded a frequent impairment of the child's self-esteem levels.52
The data referring to the maturity I.Q and self-esteem suggest that children play an active role during the course of the disease. A child with good cognitive abilities, such as abstract reasoning and perceptive organization skills, could have more chances to understand what his/her cardiologist tells him/her about the treatment and would adhere more easily to the therapeutic project. Several recent theories have suggested that perception and cognition are fundamentally activated by the body.53–56
Appropriate levels of self-esteem can be considered as a valuable resource that could favour the adherence to the therapeutic project. Children, with cognitive instruments and good levels of self-esteem, are more likely to cope with the treatment and the therapy. Self-representation and self-esteem even play a fundamental role in coping with the risk condition of the chronic pathology.25,57
With regard to the data concerning the mother's perception of her own competence, there is more evidence,39 that mothers perceive themselves as almost competent in managing their emotions and relation with their child's disease (emotional and cognitive coping), and in taking care of him/her in terms of caregiving, steering and controlling (scaffolding). Such resources serve not only to protect the child, but also to build a relationship with the medical staff. A good maternal competence perception would seem to facilitate the alliance between the cardiologist and the parents whose relationship should be based on adherence and active parental participation in the child's cure, together with any choices regarding further treatments and/or surgical intervention necessary for the treatment of the chronic disease.
The correlations between the indicators of maternal competence (Q-Sort) and those of the child's self-representation highlight interesting outcomes; especially with regard to the child's body-related image (HFDT) and his/her self-esteem (TMA). Some results of this study confirm the findings of previous research projects that have reported that parents and children influence each other in a reciprocal manner.26,28,58 The positive correlations between a factor of maternal competence such as emotional coping (A1 factor of the Q-Sort) and the child's self-image adequacy (investigated by the HFDT), and emotional scaffolding (B1 factor of the Q-Sort) and the child's emotional self-esteem (TMA), would seem to suggest that the mother's ability to control her own emotions in the relationship with her CHD child as well as to show him/her how to manage his/her own emotions, tends to be connected with the child's body-related image and self-esteem. To put it briefly, it is likely that maternal emotional competence is strictly linked to an appropriate, balanced and positive self-image of the child. On the other hand, the mother's low emotional competence coupled with high levels of parenting stress is associated with an impairment of the child's self-image which can lead to difficulties in the adjustment process.
The correlation data from this study support the findings of Berant and associates,59 which suggest that the mother's anxiety and low emotional self-regulation when interacting with the child are associated with the child's emotional problems and poor self-image; this study also confirms the outcome of previous research indicating that the behavioural adjustment of children with CHD was significantly related to the level of parenting stress or vice-versa,19,58 that certain maternal relational competences are closely connected with the adjustment process of the CHD child.10,58,17
This study would imply that the mother's capacity to recognize her own emotions and to express them in a balanced way also in front of the child - emotional coping, as well as her ability to guide him/her to manage his/her own emotions - emotional scaffolding, is of utmost importance in the process of establishing a relationship with the child that is based on trust and shared emotions. This relational space of expression, control and orientation in the world of positive and negative emotions could help the child to learn how to deal with his/her own emotions and experiences related to his/her disease. It might also enable the child to tolerate the presence of the signs of this experience and in this way help to minimize the risk of developing a non-realistic self-image and low self-esteem. Given the reciprocal influence in the mother/child relationship that constitutes the theoretical background of this study,10,26,28 the results have also to be interpreted as the child's characteristics as opposed to the mother's psychological functioning. The study suggests that a child even if s/he suffers from CHD has an adequate image of his/her own body that integrates healthy and less healthy body parts and is aware of his/her good emotional competence, will be perceived by the mother as a strong, psychologically balanced child. Such a perception of the child boosts the mother's self-confidence making her realize that she is an adequate caregiver. This could make the mother more emotionally equipped to deal with the child.
However, the mother could perceive herself less competent in her relationship with the child when his/her self-representation is fragile and his/her environmental mastery is poor. Another source of insecurity might be her inappropriate reactions to the developmental needs of the child. The findings of certain studies on congenital heart disease show that the child's low emotional tone makes it difficult for the mother to meet the child's needs.60
These correlational data demonstrate how important a relationship based on an appropriate mastery of the emotions is for the wellbeing of both the CHD child and the mother.
It is also worth reflecting on statistically significant negative correlations between the child's self-esteem competence (HFDT) and the mother's capability of relational scaffolding (B3 of the Q-Sort on maternal competence), as well as between the child's body-related self-esteem (HFDT) and the mother's cognitive scaffolding (B2 of the Q-Sort on maternal competence).
Such data would seem to suggest that the more unconditional and rigid the child's interaction with the environment of cure and care is (the maternal relational scaffolding), the more difficult his/her environmental mastery will be (the child's self-esteem competence).
Similarly, the mother's excessive cognitive scaffolding would seem to lead to the child's low body-related self-esteem, in terms of physical strength and energy. If a child does not feel confident in his/her surroundings, above all in his/her family (personal-competence-related self-esteem), his/her mother may perceive him/her as a vulnerable child to be shielded and will consequently behave as his/her over-protective guide.
Such hypothesis and the relevant findings of the study correspond to other studies that have stressed that the tendency of the mother of the CHD child to be overprotective leads him/her to display non-adaptive modes of behaviour.17,61
This research project is unusual in the sense that it focuses, unlike most other studies, on the maternal competence related to the child's self-representation. The CHD child tends to frequently show poor self-esteem related to environmental mastery when the mother is overprotective,52 taking his/her place when making choices, interpreting events, etc. The findings of the research stress the significance of a good mother/CHD-child relationship where both of them are aware of his/her own distinct resources and competences, and none of them takes the place of the other.
Information on correlations between the self-representation of the CHD child and perceived maternal competence stress the need for the paediatric psychologist to support the child's parents in their fight for the child's wellbeing. At the same time, the study suggests to investigate the possible relation among other variables which refer to the parents (e.g. personality structure, style of parenting and his/her own representation of health/disease) and to the child (e.g. temperament, coping strategies and his/her own representation of health/disease) which were studied as independently associated rather than as interrelated variables.
The study also raises the issue of the significance of the information concerning the resources of the mother/child pair for the cardiologist in his/her relationship with both the child and the mother during the cure. If the cardiologist is aware of the child's cognitive, emotional and affective resources, s/he will be able to choose a different approach, suggesting a new treatment or surgical intervention. How to prepare a child for further invasive treatments depends on how the child has reacted to previous scars, whether s/he has developed an integrate and adequate body-related image or a structurally and functionally altered one.62
A clinical picture of each paediatric condition integrated with the child's psychological information will help cardiologists to redefine the cure in terms of care, and to strengthen the quality of life related to health (HRQL).63,64 The latter depends on the fusion of clinical conditions, its psychological implications and its impact on the family system.
Acknowledgments:
we would like to thank Maria Regina Morales, PhD, for her contribution to the research project. We are grateful to all children and mothers who took part in the research project. We also thank all the health workers in the operating unit of pediatric cardiology - Hospital Ferrarotto, Catania, who have facilitated the work of our researchers.
References
- 1.Careddu P, Castelli MA, Giuffre' L, et al. Milano: Casa editrice Ambrosiana; 2002. Pediatria generale e specialistica. [Google Scholar]
- 2.Smith P. primary care in children with congenital heart disease. J Pediatr Nurs. 2001;16:308–19. doi: 10.1053/jpdn.2001.26572. [DOI] [PubMed] [Google Scholar]
- 3.Rogers M, Fay BT, Whitfield MF, et al. Aerobic capacity, strength, flexibility and activity level in unimpaired extremely low birth weight survivors at 17 years of age compared with term-born control subjects. Pediatrics. 2005;116:58–65. doi: 10.1542/peds.2004-1603. [DOI] [PubMed] [Google Scholar]
- 4.Limperopoulos C, Majnemer A, Shevell MI, et al. Neurologic status of newborns and infants with congenital heart defects before and after open heart surgery. J Pediatr. 2000;137:638–45. doi: 10.1067/mpd.2000.109152. [DOI] [PubMed] [Google Scholar]
- 5.Mahle WT. Neurologic ad cognitive outcomes in children with congenital hearth desease. Curr Opin Pediatr. 2001;13:482–6. doi: 10.1097/00008480-200110000-00016. [DOI] [PubMed] [Google Scholar]
- 6.Daliento L, Melendugno A, Scarso P, Volpe B. Le alterazioni cognitive nella cardiopatie congenite. Proceedings del Convegno Alterazioni Neuropsichiche in Medicina Interna; Padova, Italy. 2003. [Google Scholar]
- 7.Di Cagno L, Massaglia P. Il rischio di sviluppo atipico nei bambini affetti da malattia cronica ad esordio precoce. Psichiatria dell'infanzia e dell'adolescenza. 1990;57:35–46. [Google Scholar]
- 8.Skinner RA, Piek JP. Psychosocial implications of poor motor coordination in children and adolescents. Hum Mov Sci. 2001;20:73–94. doi: 10.1016/s0167-9457(01)00029-x. [DOI] [PubMed] [Google Scholar]
- 9.Guarino A. Trento: Edizioni Erickson; 2006. Psiconcologia dell'età evolutiva. La psicologia nelle cure dei bambini malati di cancro. [Google Scholar]
- 10.Davies CL, Brown RT, Bokeman R, Campbell R. Psychological adaptation and adjustment of mothers of children with congenital hearth desease: stress, coping and family functioning. J Pediatr Psychol. 1998;16:137–49. doi: 10.1093/jpepsy/23.4.219. [DOI] [PubMed] [Google Scholar]
- 11.Goldbeck L, Braun J, Storck M, et al. Adaptation of parents to the diagnosis of a chronic disease in their child. Psychother Psychosom Med Psychol. 2001;51:62–7. doi: 10.1055/s-2001-10753. [Article in German] [DOI] [PubMed] [Google Scholar]
- 12.Lawoko S, Soares JJ. Distress and hopelessness among parents of children with hearth congenital disease, parents of children of other diseases, and parents of healthy children. J Psychosom Res. 2002;52:193–208. doi: 10.1016/s0022-3999(02)00301-x. [DOI] [PubMed] [Google Scholar]
- 13.Wray J, Sensky T. Psychological functioning in parents of children undergoing elective cardiac surgery. Cardiol Young. 2004;14:131–9. doi: 10.1017/S1047951104002045. [DOI] [PubMed] [Google Scholar]
- 14.Menahem S, Poulakis Z, Prior M. Children subjected to cardiac surgery for congenital hearth disease, Part. 1 – Emotional and psychological outcomes. Interact Cardiovasc Thorac Surg. 2008;7:600–4. doi: 10.1510/icvts.2007.171058. [DOI] [PubMed] [Google Scholar]
- 15.Spijkerboer AW, Helbing WA, et al. Long-term psychological distress in parents of children and adolescent who underwent invasive treatment for congenital heart disease. Cardiol Young. 2007;17:638–45. doi: 10.1017/S1047951107001333. [DOI] [PubMed] [Google Scholar]
- 16.Eiser C. Psychological effects of chronic disease. J Child Psychol Psychiatry. 1990;31:85–98. doi: 10.1111/j.1469-7610.1990.tb02274.x. [DOI] [PubMed] [Google Scholar]
- 17.Carey LK, Nicholson BC, Fox R. Maternal factors related to parenting young children with congenital heart disease. J Pediatr Nurs. 2002;17:174–83. doi: 10.1053/jpdn.2002.124111. [DOI] [PubMed] [Google Scholar]
- 18.Tak YR, McCubbin M. Family stress perceived social and coping following the diagnosis of a child's congenital heart disease. J Adv Nurs. 2002;39:190–8. doi: 10.1046/j.1365-2648.2002.02259.x. [DOI] [PubMed] [Google Scholar]
- 19.De Maso DR, Beardslee WR, Silbert AR, Fyler DC. Psychological functioning in children with cyanotic heart defects. J Devl Behav Pediatr. 1990;11:289–94. [PubMed] [Google Scholar]
- 20.Perricone G, Pipitone S, Morales MR, et al. Perception of family-system and parental competence in mothers of children suffering from chronic heart disease. J Cardiovasc Med. 2009;10:33. [Google Scholar]
- 21.De Maso DR, Campis LK, Wypij D, et al. The impact of maternal perceptions and medical severity on the adjustment of children with congenital heart disease. J Pediatr Psychol. 1991;16:137–49. doi: 10.1093/jpepsy/16.2.137. [DOI] [PubMed] [Google Scholar]
- 22.Thompson RJ, Gil KM, Burbach DJ, et al. Role of child and maternal processes in the psychological adjustment of children with sickle cell disease. J Consult Clin Psychol. 1993;61:468–74. doi: 10.1037//0022-006x.61.3.468. [DOI] [PubMed] [Google Scholar]
- 23.Wallander JL, Thompson RJ. Roberts M. Handbook of pediatric psychology. New York: Guilford; 1995. Psychosocial adjustment of children with chronic physical conditions. [Google Scholar]
- 24.Perricone G, Polizzi C, Morales MR, et al. Functioning of family system in paediatric oncology during treatment phase. Pediatr Hematol Oncol. 2012;29:652–62. doi: 10.3109/08880018.2012.695439. [DOI] [PubMed] [Google Scholar]
- 25.Perricone G, De Luca F, Polizzi C, et al. Perception of body self of children suffering from chronic heart disease and parent coping strategy. J Cardiovasc Med. 2009;10:44. [Google Scholar]
- 26.Belsky J. Parental and nonparental child care and children's socioemotional development: a decade review. J Marriage Fam. 1990;52:885–903. [Google Scholar]
- 27.Maccoby EE, Martin JA. Mussen PH. Handbook of Child Psychology. New York: Wiley; 1983. Socialization in the context of the family: parent-child interaction. [Google Scholar]
- 28.Maccoby EE. The role of parents in the socialization of children: an historical overview. Dev Psychol. 1992;28:1006–17. [Google Scholar]
- 29.Kazak AE. Families of chronically ill children: a systems and social-ecological model of adaptation and challenge. J Consult Clin Psychol. 1989;57:25–30. doi: 10.1037//0022-006x.57.1.25. [DOI] [PubMed] [Google Scholar]
- 30.O'Conner TG, Deater-Deckard K, Fulker D, et al. Genotype-environment correlations in late childhood and early adolescence: antisocial behavioral problems and coercive parenting. Dev Psychol. 1998;34:970–81. doi: 10.1037//0012-1649.34.5.970. [DOI] [PubMed] [Google Scholar]
- 31.Utens EM, Verhulsta FC, Meijbooma J, et al. Behavioural and emotional problems in children and adolescents with congenital heart disease. Psychol Med. 1993;23:415–24. doi: 10.1017/s0033291700028518. [DOI] [PubMed] [Google Scholar]
- 32.Fonagy P. La résilience des enfants, facteurs de risque, de protection. Pratiques Psycologiques. 2000;1:49–63. [Google Scholar]
- 33.Shavelson RJ, Hubner JJ, Stanton GC. Self-concept: validation of construct interpretations. Rev Educ Res. 1976;46:407–41. [Google Scholar]
- 34.TMA. Trento: Edizioni Erickson; 1993. Test di valutazione multidimensionale dell'autostima. [Google Scholar]
- 35.Royer J. Firenze: OS; 1979. Il disegno della figura umana. [Google Scholar]
- 36.Perricone G, Morales MR. Roma: Carocci; 2009. Madri in corsia. La competenza genitoriale nell'ospedalizzazione pediatrica. [Google Scholar]
- 37.Houzel D. Le dimensioni della genitorialità. In: Lucarelli D, Nicolò AM, Tavazza G, editors. Genitorialità in cambiamento. Vol. 23. Numero monografico di Interazioni; 2005. pp. 7–11. [Google Scholar]
- 38.Schaffer HR. Milano: Cortina editore; 2004. Psicologia dello sviluppo. [Google Scholar]
- 39.Kaye K, Fogel A. The temporal structure of face-to-face communication between mothers and infants. Dev Psychol. 1980;16:454–64. [Google Scholar]
- 40.Trevarthen C. Milano: Raffaello Cortina; 1998. Empatia e biologia. [Google Scholar]
- 41.Stephenson W. Chicago: Chicago University Press; 1953. The study of behavior: Q-tecnique and its methology. [Google Scholar]
- 42.Block J. Palo Alto: Consulting Psychological Press; 1978. The Q-sort method in personality assessment and psychiatric research. [Google Scholar]
- 43.Cassibba R. Tartabini A. Problemi e metodologie in un approccio comparatistico. Milano: McGraw-Hill; 1998. L'uso del metodo Q-sort nella ricerca osservativa.Tecniche di osservazione del comportamento infantile. [Google Scholar]
- 44.Perricone Briulotta G. Modelli e percorsi. Milano: McGraw-Hill; 2003. Agire l'osservazione. [Google Scholar]
- 45.Thurstone LL. A law of comparative judgement. Psychological Review. 1994;101:266–70. [Google Scholar]
- 46.Waters E, Deane K. Bretherton I, Waters E. Growing points in attachment theory and research (monographs of the Society for Research in Child Development) Chicago: University Of Chicago Press; 1985. Defining and assessing individual differences in attachment relantionship: Q-methodology and the organization of behavior in infancy and early childhood. [Google Scholar]
- 47.Wernovsky G, Shillingford A, Gaynor J W. Central nervous system outcomes in children with complex congenital heart disease. Curr Opin Cardiol. 2005;20:94–9. doi: 10.1097/01.hco.0000153451.68212.68. [DOI] [PubMed] [Google Scholar]
- 48.Mahle WT, Clancy R, Moss EM, et al. Neurodevelopmental outcome and lifestyle assessment in school-aged and adolescent children with hypoplastic left heart syndrome. Pediatrics. 2000;105:1082–9. doi: 10.1542/peds.105.5.1082. [DOI] [PubMed] [Google Scholar]
- 49.Scarso P, Volpe B, Melendugno A, Daliento L. Psychological problems and cognitive impairments in the GUCH Community. Italian Heart Journal. Supplement Official Journal of the Italian Federation of Cardiology. 2003;4:705–11. [PubMed] [Google Scholar]
- 50.Shillingford A, Glanzman MM, Ittenbach RF, et al. Inattention, hyperactivity, and school performance in a population of school-age children with complex congenital heart disease. Pediatrics. 2008;121:759–67. doi: 10.1542/peds.2007-1066. [DOI] [PubMed] [Google Scholar]
- 51.Kramer HH, Awiszus D, Sterzel U, et al. development of personality and intelligence in children with congenital heart disease. J Child Psychol Psychiatr. 2006;30:299–308. doi: 10.1111/j.1469-7610.1989.tb00242.x. [DOI] [PubMed] [Google Scholar]
- 52.Cohen M, Mansoor D, Langut H, Lorber A. Quality of life, depressed mood, and self-esteem in adolescents with heart disease. Psychosomc Med. 2007;69:313–8. doi: 10.1097/PSY.0b013e318051542c. [DOI] [PubMed] [Google Scholar]
- 53.Barsalou LW. Grounded cognition. Ann Rev Psychol. 2008;59:617–45. doi: 10.1146/annurev.psych.59.103006.093639. [DOI] [PubMed] [Google Scholar]
- 54.Gallagher S. Oxford: Oxford University Press; 2005. How the body shapes the mind. [Google Scholar]
- 55.Gallese V, Lakoff G. The brain's concepts: the role of the sensory-motor system in reason and language. Cognitive Neuropsych. 2005;22:455–79. doi: 10.1080/02643290442000310. [DOI] [PubMed] [Google Scholar]
- 56.Proffitt DR. Embodied perception and the economy of action. Perspect Psychologic Sci. 2006;1:110–22. doi: 10.1111/j.1745-6916.2006.00008.x. [DOI] [PubMed] [Google Scholar]
- 57.Perricone G, Morales MR, Polizzi C, Fontana V. Schemi narrativi sul sé e autostima nel bambino con neoplasia: uno studio pilota pretest. Minerva Pediatrica. 2010;62(1):43–50. [PubMed] [Google Scholar]
- 58.Collins WA, Maccoby EE, Steinberg L, et al. Contemporary research on parenting: the case for nature and nurture. Am Psychologist. 2000;55:218–32. [PubMed] [Google Scholar]
- 59.Berant E, Mikulincer M, Shaver PR. Mothers' attachment style, their mental health, and their children's emotional vulnerabilities: a 7-year study of children with congenital heart disease. J Personal. 2008;76:31–66. doi: 10.1111/j.1467-6494.2007.00479.x. [DOI] [PubMed] [Google Scholar]
- 60.Gardner FV, Freeman NH, Black AM, Angelini GD. Disturbed mother-infant interaction in association with congenital heart disease. Heart. 1996;76:56–9. doi: 10.1136/hrt.76.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Steinberg L, Lamborn S, Darling N, et al. Over-time changes in adjustment and competence among adolescents from authoritative, authoritarian, indulgent and neglectful families. Child Dev. 1994;65:754–70. doi: 10.1111/j.1467-8624.1994.tb00781.x. [DOI] [PubMed] [Google Scholar]
- 62.Helman C. The body image in health and disease: exploring patients' maps of body and self. Patient Educ Couns. 1995;26:169–75. doi: 10.1016/0738-3991(95)00753-m. [DOI] [PubMed] [Google Scholar]
- 63.Koot HM. Koot HM, Wallander JL. Quality of life in child and adolescent illness. Hove: Brunner-Routdeledge; 2001. The study of quality of life: concepts and methods. [Google Scholar]
- 64.Landolt MA, Valsangiacomo Buechel ER, Latal B. Health related quality of life in children and adolescents after open-hearth surgery. J Pediatr. 2008;152:349–55. doi: 10.1016/j.jpeds.2007.07.010. [DOI] [PubMed] [Google Scholar]


