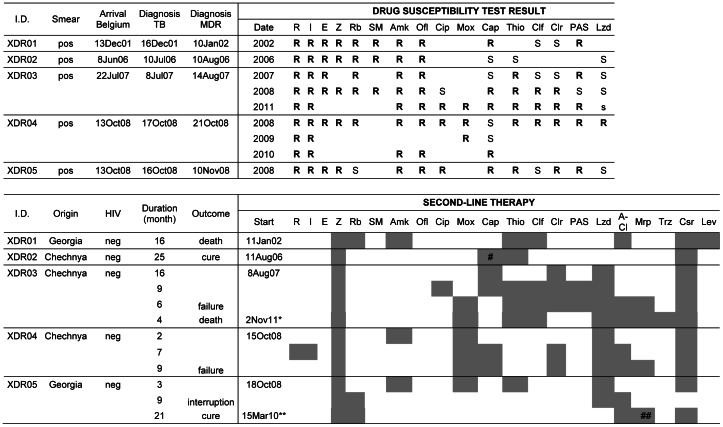
Figure 5. Patients with XDR-TB in their first isolate examined in Belgium, 1994–2008.
Part I: patient characteristics and DST results. Part II: second-line therapy with treatment outcome. Legend: *New treatment regimen initiated after 19 months without anti-TB treatment **Retreatment after interruption of 5 months #Stop after 8 months ##Stop after 7 months Antibiotics: R = Rifampicin, I = Isoniazid, E = Ethambutol, Z = Pyrazinamid, Rb = Rifabutin, SM = Streptomycin, Amk = Amikacin, Ofl = Ofloxacin, Cip = Ciprofloxacin, Mox = Moxifloxacin, Cap = Capreomycin, Thio = Thioamides, Clf = Clofazimin, Clr = Clarithromycin, PAS = para-aminosalycilic acid, Lzd = Linezolid, A-Cl = amoxicillin–clavulanate, Mrp = Meropenem, Trz = Thioridazine. The first treatment failure (XDR03) was simultaneously infected by two genetically different Beijing XDR strains, as detected by double alleles in 5 MIRU-VNTR loci. The second strain, not included in this study because not isolated from the patient’s first specimen, had additional resistance to capreomycin and clofazimine compared to the first one. After 31 months of unsuccessful hospital-supervised therapy, treatment was stopped. Nineteen months later, a new 9-drug regimen (including thioridazine) was prescribed but the patient died 4 months later. The second failure case (XDR04, the “panresistant” patient MDR169 mentioned in the text) returned to his home country after 18 months therapy, and subsequently died.