Abstract
Objectives
The financing and organization of primary care in the United States (US) has changed dramatically in recent decades. Primary care physicians have shifted from solo practice to larger group practices. The culture of a medical practice is thought to have an important influence on physician behavior. This study examines the effects of practice culture and organizational structure (while controlling for patient and physician characteristics) on the quality of physician decision making.
Methods
Data were obtained from a balanced factorial experiment which employed a clinically authentic videotaped scenario of diabetes with emerging peripheral neuropathy.
Results
Our findings reveal significant impacts of several key practice culture variables on clinical decision making with respect to diabetes. These data suggest that practice culture may contribute more to whether essential examinations are performed than patient, physician or the structural characteristics of organizations.
Conclusions
Attention is beginning to focus on physician behavior in the context of different organizational environments. This study provides additional support for the suggestion that organization-level interventions (especially focused on practice culture) may offer an opportunity to reduce healthcare disparities and improve the quality of care.
INTRODUCTION
The financing and organization of primary health care in the United States (US) has changed dramatically in recent decades. Previously, primary care physicians were solo practitioners working independently in fee-for-service systems. Nowadays, most primary care physicians are salaried employees working in large group settings. When operating in a fee-for-service system physicians had a considerable autonomy; they could see patients when they wanted, for as long as they wanted, prescribe what they wanted, and order whatever tests they wanted. During this so-called “Golden Age of Doctoring”, doctors enjoyed high levels of clinical autonomy and considerable latitude in decision making 1. However, in the current climate of larger practice settings, doctors may now find their clinical decision making tightly monitored and highly regulated.
Given the primary care shift from solo practice to group practice, an organizational perspective is now increasingly employed to understand physician behavior 2. In particular, the culture of a medical practice has been identified as a major influence on the cost and quality of health care 3–6. The Committee on Quality Healthcare in America identifies practice culture as a fundamental factor in improving patient quality of care and reducing adverse events 7. Curoe and Kaissi have shown that practice culture is associated with organizational structures (i.e., size and ownership of practice) and the availability of quality related programs (i.e., electronic medical records (EMR), use of practice guidelines) in a medical practice 8, 9. However, studies of the effects of medical culture on physician behavior have produced mixed results. Possible explanations for the lack of consistent findings have been interactions with organization characteristics, differences in patient/physicians characteristics, and un-measurable differences in presenting illness.
In this paper, we examine the relative contributions of practice culture, organizational characteristics, patient attributes, and physician characteristics on physician decision making for diabetes. Specifically, we address three questions: 1) Does the culture of a medical practice have any effect on the clinical management of diabetes by primary care physicians? 2) Are organizational characteristics related to practice culture? 3) What contributes the most to physician decision making with respect to diabetes: practice culture, organizational characteristics, physician characteristics, or patient attributes? To our knowledge, this is the first study to examine the effect of practice culture on physician decision making in the management of diabetes.
METHODS
Study Design
We conducted a factorial experiment using clinically authentic videotaped patient scenarios. The study focused on a range of clinical decisions as they relate to a case of diagnosed diabetes with an emerging peripheral neuropathy. Research methods are summarized below. 10
A version of the videotaped diabetes “patient” with an emerging peripheral neuropathy condition (varying by age, race/ethnicity, SES, or gender) was shown to each of the physicians recruited as subjects for the experiment. We recruited a total of 192 primary care physicians, stratified according to gender and level of clinical experience until each cell was filled. The “patient”, had already been diagnosed with diabetes and reported symptoms suggestive of peripheral neuropathy: “burning in the feet which sometimes goes up the ankle” that “comes and goes.” Each case was developed with the input of expert clinicians who regularly treat patients with diabetes and confirmed the accuracy of the clinical content. A clinical consultant to the study advised that real patients seldom present as pure “text-book cases”, therefore several minor distractions were embedded in the presentation, including a single high blood pressure reading (145/98). The patient stated that they were concerned about the blood pressure reading and reported being on blood pressure medication but with non-ideal compliance. These distractions were not included to make the task more difficult but to increase the clinical authenticity of the clinical scenario.
Immediately after viewing the selected video for the experiment, the experimental subjects (physicians) completed a semi-structured interview. This interview included questions concerning how they would manage the case of diagnosed diabetes with the emerging complication depicted in the video in their everyday clinical practice, including their test ordering, prescriptions, lifestyle recommendations, and what other information they might seek.
Experimental Stimuli (Scenarios)
Professional actors and actresses were trained under experienced physician supervision to realistically portray a diabetic “patient” presenting to a physician with the signs and symptoms of emerging peripheral neuropathy. Twenty-four versions of the scenario were videotaped, systematically varying the “patient’s” age (35 vs. 65), race/ethnicity (black, white, or Hispanic), gender and SES (lower vs. higher social class – a janitor vs. a lawyer). Each videotaped encounter simulated an initial interview with a primary care provider and was of 5–7 minutes in duration, reflecting the average length of face-time with a primary care physician in the US.
Experimental Subjects (Physicians)
To be eligible for selection physicians had to: (a) be primary care physicians; (b) be trained at an accredited medical school in the US (since this was a subset of an international study); (c) be currently providing clinical care at least half time; (d) have ≤12 years clinical experience (graduated between 1993–99) or ≥22 years experience (graduated between 1969–83). The dichotomy on years of clinical experience was created in order to ensure clear separation on less/more clinical experience. Eligible physicians were purposively sampled from throughout New Jersey, New York, and Pennsylvania to equally fill four design cells. Patient and physician characteristics were balanced by design to ensure orthogonality (un-confounded estimates on all design variables). Screening telephone calls were conducted to identify eligible subjects and an hour-long, in-person interview was scheduled (at which time written informed consent was obtained). A subset of the 192 US physicians, excluding 70 physicians in solo practice who did not answer the questions on practice culture (N=122) were included in these analyses.
Measures
Physicians’ practice culture was measured by an abbreviated version of the Medical Group Practice Culture Survey a standardized self-administered questionnaire with 10 Likert-scaled items measuring 9 cultural dimensions. 2, 11 The instrument was developed with the input of medical directors and primary care physicians.6 There is no gold standard for measuring the culture of medical group practices, however, the psychometric properties of this instrument indicate validity and reliability.6 The Medical Group Practice Culture Survey has shown to have predictive value in small and large group practice environments.8, 9 Many measures of organizational culture have focused on hospitals rather than medical practices.12 The Medical Group Practice Culture Survey was explicitly designed for use among primary care physicians making it the most appropriate measure of practice culture for our study population. The items are listed in Table 1 with means and standard deviations for each practice culture dimension. Participants were asked to indicate the extent to which they agreed with the statements from 1=Not at all to 4=A great extent.
Table 1.
Practice Culture Dimensions, Mean (Standard Deviation)
| Cultural Dimensions | Group Physicians N=122 |
|---|---|
| Collegiality | 2.8 (0.82) |
| There is a great deal of sharing clinical information | |
| Information emphasis | 3.0 (0.79) |
| We value information technologies | |
| Quality Emphasis | 2.9 (0.79) |
| We encourage internal discussion of patient care adverse events. | |
| Management Style | 2.7 (0.84) |
| Our administrative decision making process can best be described as consensus building. | |
| Cohesiveness | 2.9 (0.75) |
| 1. There is an identifiable practice style that we all try to adhere to. | |
| 2. There is a strong sense of belonging to the group. | |
| Organizational Trust | 2.8 (0.84) |
| There is a high degree of organizational trust. | |
| Adaptive | 2.5 (0.81) |
| We are quick to adopt new techniques and practices. | |
| Autonomy | 2.8 (0.92) |
| There is a feeling that we are each autonomous clinicians, but practicing in the same organization for support services. | |
| Business Emphasis | 2.3 (0.89) |
| Business decisions are heavily weighted toward profit maximization. |
1=Not agree with this statement at all
2=Sometimes agree with this statement
3=Often agree with the statement
4=Agree with this statement to a great extent
Organizational characteristics found to be influenced by practice culture in previous studies were also included in our analysis: practice size, ownership, availability of clinical guidelines, and use of an EMR. Patient and physician characteristics were included as possible explanatory factors since they were design factors of the study.
Widely accepted guidelines from the American Diabetes Association, the Agency for Health Research and Quality, and an experienced consulting diabetologist to the projects suggest that three examinations be performed at any suggestion of foot ailments among diabetics.13, 14 The three key examinations are: 1) visual inspection for ulcers—the most common foot injuries leading to lower extremity amputation; 2) vibration/monofilament exam—a simple test in which a monofilament is gently pressed against the foot to test how much sensation a person has in his or her feet. This provides an indication of whether nerve damage has occurred; and 3) palpation of foot pulses—absent foot pulses indicate peripheral vascular disease which conveys a greater risk for foot ulceration. A number of other examinations/tests (i.e. any foot exam, loss of sensation, altered biomechanics, increased pressure), medications (i.e. antidiabetic agents, anti-platelets), advice (i.e. perform foot self exams, increase compliance with other medications) and referrals (podiatrist, ophthalmologist) were included as potential dependent variables.
Statistics
The independent variables are the practice culture dimensions. The dependent variables are the clinical actions the physicians reported they would take if presented with a patient as in the videotaped scenario. Due to the large number of comparisons, there are potential problems with multiple testing. Recognizing this issue, we focus on the consistency of our findings, rather than on any single statistically significant result. Logistic regression analyses were used to obtain odds ratios and p-values. Odds ratios are presented for a one unit change in practice culture. A generalized coefficient of determination (R2) statistic 15 was used to determine the relative contributions of practice culture, structure, patient characteristics and physician characteristics in a logistic regression model. The R2 can be interpreted as the proportion of variation in the dependent variable that can be explained by each independent variable in the model 16. Model building was conducted in three phases: 1) each variable was introduced to the model independently, without other covariates, 2) covariates were ranked by their influence, as determined by the coefficient found in the first step, and 3) coefficients were added to the final model by order of influence, as found in the second step, and their contribution to the R2 was calculated. All analyses were conducted using SAS 9.1 (Cary, NC, US).
RESULTS
Of the 122 group practice physicians in our analytic sample, 47.4% (n = 57) would perform a visual examination for ulcers, 63.1% (n = 77) would perform a vibration/monofilament exam, and 67.2% (n = 82) would check the patient’s foot pulses. Only 52 (42.6%) would perform all three examinations. Our first analysis examined the main effects of practice culture on these three key examinations as well as other clinical activities (i.e. examinations, prescription writing, and referrals).
Several practice culture dimensions were found to have an impact on the major outcome of interest: vibration/monofilament exam, check for ulcers, and foot pulses (Table 3). Physicians in practices that emphasize collegiality (OR=1.6, p=0.04), information emphasis (OR=1.8, p=0.02), cohesiveness (OR=1.6, p=0.05), and organizational trust (OR=1.7, p=0.02) were all more likely to perform the vibration/monofilament exam. Physicians in practices that emphasize organizational trust were also more likely to perform a visual examination for ulcers (OR=1.7, p=0.02), while physicians in practices that emphasize autonomy were less likely to perform this key examination (OR=0.7, p=0.05). Physicians working in a practice with a culture of autonomy were less likely to perform a number of examinations, including: examination for ulcers (p=0.05), loss of sensation (p = 0.009), increased pressure (p = 0.05), bone deformity (p=0.02), and nail pathology (p< 0.001).
Table 3.
Effects of Practice Culture on Diabetes Management Outcomes (Odds Ratio, p-value)
| Collegiality | Information Emphasis | Quality Emphasis | Management Style | Cohesiveness | Organizational Trust | Adaptive | Autonomy | Business Emphasis | |
|---|---|---|---|---|---|---|---|---|---|
| Examinations | |||||||||
| Vibration/Monofilament test | 1.6 (0.04) | 1.8 (0.02) | 1.2 (0.53) | 1.2 (0.42) | 1.6 (0.05) | 1.7 (0.02) | 1.1 (0.58) | 0.8 (0.33) | 1.5 (0.09) |
| Ulcers | 1.3 (0.21) | 1.1 (0.58) | 1.1 (0.61) | 1.1 (0.64) | 1.4 (0.18) | 1.6 (0.04) | 0.9 (0.64) | 0.7 (0.05) | 1.3 (0.16) |
| Foot Pulses | 1.1 (0.61) | 1.0 (1.00) | 0.9 (0.63) | 1.2 (0.47) | 1.1 (0.62) | 1.3 (0.31) | 0.9 (0.81) | 0.7 (0.15) | 1.2 (0.44) |
| Foot Exam | 0.9 (0.86) | 0.8 (0.63) | 1.0 (0.95) | 1.1 (0.72) | 1.2 (0.55) | 0.8 (0.40) | 0.9 (0.64) | 0.6 (0.10) | 0.6 (0.11) |
| Loss of sensation | 1.0 (0.85) | 1.0 (0.85) | 1.0 (0.89) | 1.2 (0.37) | 1.5 (0.12) | 1.3 (0.19) | 0.9 (0.69) | 0.6 (0.009) | 1.2 (0.51) |
| Altered biomechanics | 1.0 (0.99) | 0.9 (0.71) | 1.0 (1.00) | 1.3 (0.39) | 1.6 (0.14) | 1.5 (0.16) | 0.9 (0.82) | 0.7 (0.09) | 1.1 (0.77) |
| Increased pressure | 1.1 (0.74) | 1.0 (0.99) | 0.9 (0.77) | 0.7 (0.09) | 1.0 (0.87) | 1.0 (0.86) | 0.6 (0.09) | 0.7 (0.05) | 1.3 (0.24) |
| Bone deformity | 1.5 (0.26) | 0.8 (0.57) | 1.1 (0.70) | 1.1 (0.85) | 1.7 (0.18) | 1.2 (0.63) | 0.8 (0.47) | 0.5 (0.02) | 1.0 (0.92) |
| PVD Peripheral vascular disease | 0.7 (0.23) | 0.9 (0.62) | 0.7 (0.09) | 0.5 (0.004) | 0.8 (0.32) | 0.7 (0.09) | 0.7 (0.23) | 0.7 (0.09) | 1.0 (0.87) |
| Nail pathology | 1.2 (0.41) | 1.0 (0.96) | 1.3 (0.38) | 1.2 (0.45) | 1.5 (0.15) | 1.2 (0.56) | 0.7 (0.24) | 0.4 (<0.001) | 1.2 (0.43) |
| Fundoscopic exam | 0.8 (0.58) | 0.8 (0.71) | 0.9 (0.85) | 2.1 (0.14) | 1.0 (0.97) | 1.6 (0.32) | 0.5 (0.21) | 1.5 (0.35) | 2.1 (0.06) |
| Tests | |||||||||
| Fasting Glucose/HBA1C Test | 1.1 (0.83) | 0.8 (0.31) | 1.0 (0.99) | 1.0 (0.95) | 1.0 (0.95) | 1.3 (0.26) | 0.7 (0.21) | 0.7 (0.11) | 1.3 (0.32) |
| Fasting lipid profile | 1.1 (0.60) | 0.9 (0.79) | 1.0 (0.95) | 1.4 (0.18) | 1.3 (0.32) | 1.0 (0.86) | 0.9 (0.80) | 1.1 (0.77) | 1.2 (0.43) |
| Non-fasting lipid profile | 1.8 (0.23) | 1.0 (0.93) | 6.7 (0.02) | 2.1 (0.15) | 2.4 (0.15) | 2.8 (0.07) | 2.4 (0.08) | 1.0 (0.93) | 2.1 (0.09) |
| Medications | |||||||||
| Antidiabetic agents | 1.0 (0.93) | 1.1 (0.84) | 1.4 (0.27) | 1.0 (0.96) | 1.0 (0.90) | 1.2 (0.46) | 0.9 (0.55) | 0.8 (0.38) | 1.6 (0.05) |
| Anti-Platelets | 0.7 (0.21) | 1.3 (0.31) | 0.9 (0.60) | 1.0 (0.88) | 0.9 (0.82) | 1.0 (0.88) | 0.8 (0.38) | 0.9 (0.78) | 1.6 (0.05) |
| Lipid Medications | 1.0 (0.88) | 1.5 (0.25) | 1.7 (0.16) | 1.2 (0.54) | 1.0 (0.90) | 1.1 (0.84) | 0.6 (0.13) | 1.2 (0.61) | 1.4 (0.31) |
| Blood Pressure Medications | 1.0 (0.83) | 1.0 (0.92) | 0.9 (0.76) | 1.1 (0.78) | 1.0 (0.95) | 1.1 (0.77) | 0.7 (0.18) | 0.7 (0.11) | 1.0 (0.83) |
| Advice | |||||||||
| Foot self exams | 0.9 (0.67) | 1.1 (0.83) | 1.4 (0.26) | 1.0 (0.96) | 1.2 (0.45) | 1.1 (0.73) | 1.2 (0.40) | 0.7 (0.07) | 1.1 (0.74) |
| Increase compliance with other medications | 0.8 (0.35) | 0.9 (0.75) | 1.2 (0.37) | 1.1 (0.58) | 0.8 (0.50) | 1.2 (0.52) | 0.8 (0.38) | 1.0 (0.92) | 1.5 (0.05) |
| Referrals | |||||||||
| Podiatrist/Chiropodist | 1.6 (0.11) | 1.2 (0.46) | 2.5 (0.004) | 1.7 (0.06) | 2.0 (0.03) | 1.6 (0.09) | 0.9 (0.72) | 0.9 (0.61) | 1.1 (0.64) |
| Opthamologist | 1.2 (0.50) | 1.0 (0.97) | 1.6 (0.10) | 1.3 (0.29) | 1.6 (0.09) | 1.7 (0.04) | 1.1 (0.73) | 1.2 (0.51) | 1.0 (0.84) |
Bold = relationship is significant at 0.05 or below
An odds ratio greater than 1.0 indicates a positive relationship (i.e. for a one unit increase in organizational trust the odds that a physician will perform a vibration/monofilament exam are 1.7 times higher)
An odds ratio less than 1.0 indicates a negative relationship
Physicians reporting their group practice to be oriented towards profit maximization were the only group of physicians more likely to emphasize medications including: prescribing anti-diabetic agents (p=0.05), prescribing anti-platelets (p=0.05), and advising increased compliance with other medications (p=0.05).
Table 4 illustrates the relationship between practice culture and. selected organizational characteristics. Practices with a culture of collegiality are associated with greater use of an EMR (OR=1.8, p=0.02). Having an information emphasis is associate with greater access to (OR=2.3, p=0.01) and use of (OR=2.1, p=0.02) clinical guidelines and greater use of an EMR (OR=4.6, p < 0.0001). Cultures of quality emphasis, cohesiveness and organizational trust are associated with physician-ownership (OR=2.1, 2.3, and 2.4, respectively). Several of these findings are consistent with other studies indicating that our necessarily shortened practice culture scale appears to have not diminished the validity of the components 8, 9.
Table 4.
Relationships between Organizational Characteristics and Practice Culture (Odds ratio, p-value)
| Collegiality | Information Emphasis | Quality Emphasis | Management Style | Cohesiveness | Organizational Trust | Adaptive | Autonomy | Business Emphasis | |
|---|---|---|---|---|---|---|---|---|---|
| Practice Size (4 or more physicians vs. 2–3 physicians) | 1.0 (0.86) | 0.9 (0.79) | 0.7 (0.14) | 1.2 (0.52) | 0.7 (0.25) | 0.7 (0.07) | 1.0 (0.98) | 1.0 (0.93) | 1.4 (0.15) |
| Physician Owned (vs. hospital owned or other) | 1.3 (0.27) | 1.0 (0.94) | 2.1 (0.004) | 1.2 (0.36) | 2.3 (0.003) | 2.4 (<0.001) | 1.5 (0.10) | 1.1 (0.80) | 1.4 (0.09) |
| Access to clinical guidelines | 1.2 (0.49) | 2.3 (0.01) | 1.2 (0.46) | 1.0 (0.87) | 1.0 (0.90) | 1.1 (0.65) | 1.3 (0.37) | 0.9 (0.67) | 0.8 (0.43) |
| Use clinical guidelines | 1.2 (0.45) | 2.1 (0.02) | 1.0 (0.95) | 0.9 (0.71) | 1.0 (0.94) | 1.0 (0.99) | 1.2 (0.49) | 0.8 (0.44) | 0.8 (0.30) |
| Use of EMR | 1.8 (0.02) | 4.6 (<0.001) | 1.0 (0.88) | 1.0 (0.87) | 1.3 (0.29) | 1.2 (0.37) | 1.2 (0.40) | 1.0 (0.83) | 0.9 (0.80) |
Bold = relationship is significant at .05 or below
An odds ratio greater than 1 indicates a positive relationship
An odds ratio less than 1 indicates a negative relationship
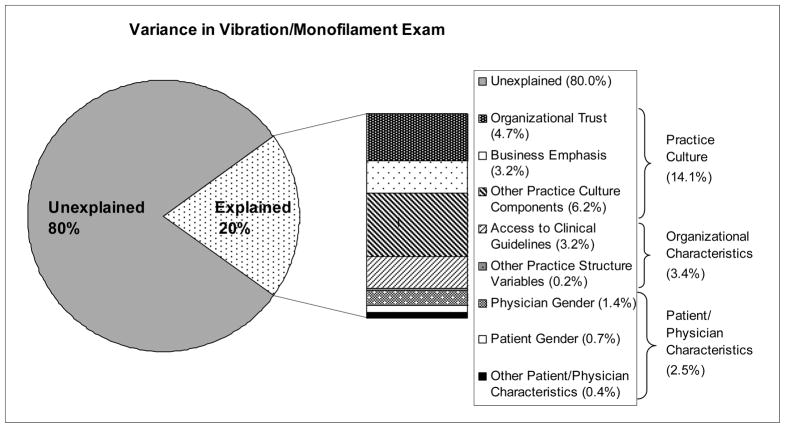
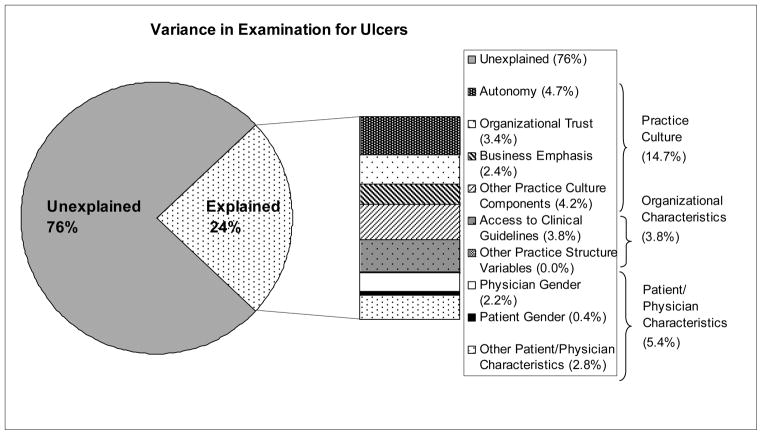
Finally, we examined the relative contributions of practice culture, practice structure and resources, patient characteristics and physician characteristics on an outcome of particular interest: the vibration/monofilament exam, which is considered a vital exam for the detection of peripheral neuropathy (Figure 1). With respect to practice culture, organizational trust and business emphasis contribute the most to the variance in the vibration/monofilament exam. These two cultural dimensions explain about 8% of the variability in the vibration/monofilament exam. When all nine practice culture dimensions are considered 14.1% of the variance in this examination is explained. Access to clinical guidelines explains about 3% of the variability, while other structural/resource variables measured here contributed little to the variability in the vibration/monofilament exam (0.2%). Patient characteristics (race/ethnicity, SES, age, and gender) and physician characteristics (gender and experience) explain only 2.5% of the variability. Results were strikingly similar for the examination for ulcers (Figure 2). No cultural dimensions were found to significantly impact palpitation of the foot pulses.
Figure 1.
Percent of Variance in Vibration/Monofilament Exam Explained by Practice Culture, Organizational Resources, Patient and Physician Characteristics
Figure 2.
Percent of Variance in Examination for Ulcers Explained by Practice Culture, Organizational Resources, Patient and Physician Characteristics
DISCUSSION
This study provides new information on the effects of several dimensions of practice culture on physician decision making with respect to diabetes. Practice culture may contribute more to the variability in the management of diabetes than patient and physician attributes combined, which is where much research is currently focused.
Physicians in practices that score high on collegiality, information emphasis, cohesiveness, and organizational trust were all more likely to report they would perform a vibration/monofilament exam. This is not surprising since these components are all related, yet distinct, culture constructs. The collegiality component reflects a shared sense of belonging to a close knit group of clinicians who openly share information. Conversely, the information component is more focused on the technical side of communications and reflects a commitment to information-based clinical practices to assist in decision-making. Organization trust reflects open organizational communications and a commitment to structures that support clinical practices, while cohesiveness reflects an organizational level approach to patient care 11.
The business and autonomy components diverge theoretically from the components discussed above. The business emphasis component expresses the degree to which bottom-line financial performance and profits are thought to dominate the culture of the practice 9. Physicians in practices that emphasize profit maximization were not generally focused on the guideline suggested examinations, but rather on the prescribing medications and adherence to a medication regimen.
A practice culture of Autonomy values physicians’ individuality and these practices have been described to have a “me” rather than an “us” orientation 11. In theory this construct is the opposite of cultures with a high degree of collegiality. Physicians practicing in cultures that score high on autonomy were less likely to report they would perform a variety of examinations for their patients. Out of the 22 items examined in our study, physicians in practices that emphasize autonomy were less likely to perform 16/22 of the items. In previous studies, practices that emphasize autonomy were found to be negatively associated with the use of quality-related programs, including the use of clinical guidelines 9. Our data showed a similar trend. This may indicate that without adequate support systems a culture of autonomy may have a detrimental effect on the quality of patient care.
Our study challenges the hypothesis that much of the variability in episodes or care are the result of unobserved patient and illness characteristics5 since all patient and physician characteristics were controlled in our factorial design. Moreover, all illness/severity characteristics were absolutely identical in the videotapes. Our statistical results indicate that practice culture may contribute more to the variability in the performing of key examinations than either patient or physician characteristics.
Strengths/Limitations
Several strengths and limitations of this study should be noted. The experimental approach in this study offers excellent internal validity and allows for the control of important patient/physician characteristics. However, the use of hypothetic “patients” may threaten external validity. This concern centers on whether a physicians’ evaluation and management of the case presented on the videotape reflects their behavior with real patients. We took a number of steps to hopefully minimize any problems with external validity. First, we made every effort to assure that the videotapes were realistic, 90.2% of the physicians thought the patient was typical or very typical of patients in their practice. Second, physicians viewed the videotapes in their office during their regular office hours. Third, physicians were specifically instructed at the outset to view the “patient” as one of their own, and respond as they would typically in their own practice. While there was initial resistance to the use of videotaped scenarios in health services research this appears to have now dissipated with accumulating evidence that they produce valid findings and that they have distinct advantages over other approaches (written scenarios and standardized patients) 17–20.
Conclusion
In order to address worrisome variations in diabetes care that occur at the level of the primary care provider, future interventions should focus on modifications to the practice/organizational culture. Our findings reinforce the literature suggesting that practice culture influences the nature and quality of medical decision making. This study has important implications for future interventions to reduce health care disparities occurring at the level of provider behavior. Most research to date has focused on patient and physician attributes, and likewise, most interventions focus on changing patient behavior and individual physician performance Attention is beginning to focus on physician behavior in the context of different organizational environments. This study provides support for the suggestion that modification of the organizational context within which physicians work (specifically practice culture) may offer an additional opportunity to improve the quality of care 21.
Table 2.
Organizational characteristics of the physicians included in the study sample
| Group Physicians N=122 | |
|---|---|
| Practice Size | |
| 2–3 physicians | 44 (36.1%) |
| 4–10 physicians | 59 (48.4%) |
| More than 10 physicians | 19 (15.6%) |
| Ownership | |
| Physician Owned | 54 (44.6%) |
| Hospital Owned | 38 (31.4%) |
| Other | 29 (24.0%) |
| Access to quality-related programs (% Yes) | |
| Access to clinical guidelines | 101 (82.8%) |
| Use clinical guidelines | 98 (80.3%) |
| Use electronic medical records (EMR) | 35 (28.7%) |
Acknowledgments
Financial support for this study was provided entirely by a grant from National Institutes of Health (#R01 DK66425)
Contributor Information
Rebecca J. Shackelton, Email: rshackelton@neriscience.com, New England Research Institutes, 9 Galen Street, Watertown, MA 02472, USA, Tel: (617) 923-7747 ext. 419; Fax: (617) 926-8246.
Carol L. Link, Email: clink@neriscience.com, New England Research Institutes.
Lisa D. Marceau, Email: lmarceau@neriscience.com, New England Research Institutes.
John B. McKinlay, Email: jmckinlay@neriscience.com, New England Research Institutes.
NOTES
- 1.McKinlay JB, Marceau LD. The end of the golden age of doctoring. International Journal of Health Services. 2002;32(2):379–416. doi: 10.2190/JL1D-21BG-PK2N-J0KD. [DOI] [PubMed] [Google Scholar]
- 2.Kralewski JE, Wingert TD, Barbouche MH. Assessing the culture of medical group practices. Med Care. 1996 May;34(5):377–388. doi: 10.1097/00005650-199605000-00001. [DOI] [PubMed] [Google Scholar]
- 3.Shortell SM, Jones RH, Rademaker AW, Gillies RR, Dranove DS, Hughes EFX, Budetti PP, Reynolds KSE, Huang CF. Assessing the Impact of Total Quality Management and Organizational Culture on Multiple Outcomes of Care for Coronary Artery Bypass Graft Surgery Patients. Medical Care. 2000;38(2):202–217. doi: 10.1097/00005650-200002000-00010. [DOI] [PubMed] [Google Scholar]
- 4.Shortell SM, Zazzali JL, Burns LR, Alexander JA, Gillies RR, Budetti PP, Waters TM, Zuckerman HS. Implementing Evidence-Based medicine: The Role of Market Pressures, Compensation Incentives, and Culture in Physician Organizations. Medical Care. 2001;39(7 Suppl):I62–I78. [PubMed] [Google Scholar]
- 5.Kralewski JE, Wallace W, Wingert TD, Knutson DJ, Johnson CE. The Effects of Medical Group Practice Organizational Factors on Physicians’ Use of Resources. Healthcare Management. 1999;44(3):167–182. [PubMed] [Google Scholar]
- 6.Kralewski JE, Dowd BE, Heaton A, Kaissi A. The influence of the structure and culture of medical group practices on prescription drug errors. Med Care. 2005 Aug;43(8):817–825. doi: 10.1097/01.mlr.0000170419.70346.b8. [DOI] [PubMed] [Google Scholar]
- 7.Committee on Quality of Health Care in America. Crossing the quality chasm: a new health system for the 21st Century. Washington, DC: Institute of Medicine; 2001. [Google Scholar]
- 8.Curoe A, Kralewski J, Kaissi A. Assessing the cultures of medical group practices. J Am Board Fam Pract. 2003 Sep-Oct;16(5):394–398. doi: 10.3122/jabfm.16.5.394. [DOI] [PubMed] [Google Scholar]
- 9.Kaissi A, Kralewski J, Curoe A, Dowd B, Silversmith J. How does the culture of medical group practices influence the types of programs used to assure quality of care? Health Care Manage Rev. 2004 Apr-Jun;29(2):129–138. doi: 10.1097/00004010-200404000-00006. [DOI] [PubMed] [Google Scholar]
- 10.McKinlay J, Link C, Arber S, et al. How do Doctors in Different Countries Manage the Same Patient? Results of a Factorial Experiment. Health Services Research. 2006;41(6):2182–2200. doi: 10.1111/j.1475-6773.2006.00595.x. [Erratum in 2141(2186):2303] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kralewski J, Dowd BE, Kaissi A, Curoe A, Rockwood T. Measuring the culture of medical group practices. Health Care Manage Rev. 2005 Jul-Sep;30(3):184–193. doi: 10.1097/00004010-200507000-00002. [DOI] [PubMed] [Google Scholar]
- 12.Scott T, Mannion R, Davies H, Marshall M. The Quantitative Measurement of Organizational Culture in Health Care: A Review of Available Instruments. Health Services Research. 2003;38(3):923–945. doi: 10.1111/1475-6773.00154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.American Diabetes Association. Standard of Medical Care in Diabetes-2008. Diabetes Care. 2008;31(Supplement 1):S12–S54. doi: 10.2337/dc08-S012. [DOI] [PubMed] [Google Scholar]
- 14. [Accessed March 17, 2008];The National Guideline Clearinghouse. http://www.guidelines.gov.
- 15.Cox DR, Snell EJ. Analysis of Binary Data. 2. Chapman & Hall; 1989. [Google Scholar]
- 16.Rothman KJ, Greenland S. Modern Epidemiology. 2. Philadelphia: Lippincott, Williams, & Wilkins; 1998. [Google Scholar]
- 17.McDaniel SH, Beckman HB, Morse DS, Silberman J, Seaburn DB, Epstein RM. Physician self-disclosure in primary care visits: enough about you, what about me? Arch Intern Med. 2007 Jun 25;167(12):1321–1326. doi: 10.1001/archinte.167.12.1321. [DOI] [PubMed] [Google Scholar]
- 18.Veloski J, Tai S, Evans AS, Nash DB. Clinical vignette-based surveys: a tool for assessing physician practice variation. Am J Med Qual. 2005 May-Jun;20(3):151–157. doi: 10.1177/1062860605274520. [DOI] [PubMed] [Google Scholar]
- 19.Peabody JW, Luck J, Glassman P, Dresselhaus TR, Lee M. Comparison of Vignettes, Standardized Patients, and Chart Abstraction: A Prospective Validation Study of 3 Methods for Measuring Quality. Journal of the American Medical Association. 2000 Apr 5;283(13):1715–1722. doi: 10.1001/jama.283.13.1715. [DOI] [PubMed] [Google Scholar]
- 20.Dresselhaus TR, Peabody JW, Lee M, Wang MM, Luck J. Measuring compliance with preventive care guidelines: standardized patients, clinical vignettes, and the medical record. J Gen Intern Med. 2000 Nov;15(11):782–788. doi: 10.1046/j.1525-1497.2000.91007.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Shortell SM, Singer SJ. Improving Patient Safety by Taking Systems Seriously. JAMA. 2008;299(4):445–447. doi: 10.1001/jama.299.4.445. [DOI] [PubMed] [Google Scholar]