Abstract
Purpose
To compare the safety and efficacy of naftopidil and tamsulosin with prednisolone as medical expulsive therapy for distal ureteric stones.
Materials and Methods
Between July 2010 and March 2012, 120 adult patients presenting with distal ureteric stones of size 5 to 10 mm were randomized equally to tamsulosin (group A), naftopidil (group B) or watchful waiting (group C). Tamsulosin or naftopidil was given for a maximum of four weeks. In addition patients in group A and B were given 5 mg prednisolone once daily (maximum one week). Stone expulsion rate, time to stone expulsion, analgesic use, number of hospital visits for pain, follow-up and endoscopic treatment and adverse effects of drugs were noted. Statistical analyses were done using chi-square test, Mann-Whitney test and analysis of variance.
Results
There was a statistically higher expulsion rate in groups A (70%) and B (87.5%) as compared to group C (32.5%) (p<0.001). The expulsion rates were not statistically different between groups A and B (p=0.056). The mean time to expulsion was comparable between groups A and B but longer in group C. Analgesic use was significantly lower in groups A and B. Average number of hospital visits for pain, follow-up and endoscopic treatment was similar in all groups. There was no serious adverse event.
Conclusions
Medical expulsive therapy for the distal ureteric stones using either naftopidil or tamsulosin in combination with prednisolone is safe and efficacious.
Keywords: Naftopidil, Prednisolone, Tamsulosin, Ureteral calculi
INTRODUCTION
The lifetime risk of urinary stone disease is estimated to be between 5% and 12% in Europe and the United States, afflicting 13% of men and 7% of women [1]. Because up to 50% of patients may experience the recurrence of renal stones within 5 years of their first episode, urolithiasis is a chronic disease with substantial economic consequences and great public health importance [1]. It is well established that almost 50% of ureteral stones will pass spontaneously over time and that stone size is a critical factor influencing expulsion (only 20% of stones greater than 8 mm will pass spontaneously) [2,3]. Alpha-1-adrenergic receptors are present throughout the ureter with a high concentration in the distal third of the ureter. Blockage inhibits basal smooth muscle tone and hyperperistaltic uncoordinated frequency while maintaining tonic propulsive contractions [4]. Ureteral calculi can induce ureteral spasms that interfere with the expulsion of calculi; thus, reduction of spasm with maintenance of normal peristaltic activity can facilitate expulsion of calculi. It has been shown that ureteral calculi induce inflammatory changes in the ureteral wall and that submucosal edema around a calculus may worsen ureteral obstruction, thus increasing the risk of impaction and retention [5]. Thus, steroid drugs can facilitate stone expulsion by reducing the submucosal edema. On the basis of these observations, medical expulsive therapy using α-1-adrenergic receptor antagonists or calcium channel blockers and steroids has recently emerged as an efficacious and safe option for the initial management of ureteral stones. Tamsulosin has already been proven to increase the stone expulsion rate and to decrease the time to expulsion [6]. Recently, the newer alpha-blocker naftopidil has been studied in patients with lower urinary tract symptoms due to benign prostatic hyperplasia and has been found to be better than tamsulosin for nocturia owing to its α-1D-adrenoceptor blocking action [7]. Because the lower ureter and bladder are rich in α-1D-adrenoceptors, there is a theoretical advantage in using naftopidil in medical expulsive therapy, because it may reduce the pressure in the intramural part of the ureter, thereby facilitating stone passage. Indeed, naftopidil was shown to increase the spontaneous expulsion rate of distal ureteral stones compared with placebo in a recent study [8]. Therefore, we planned to evaluate the efficacy of naftopidil in comparison with tamsulosin in the management of distal ureteral stones.
MATERIALS AND METHODS
The study was conducted in a tertiary care institute in northern India after approval from the institutional ethics committee. Between July 2010 and March 2012 all patients older than 18 years of age with a ureteral stone 5 mm to 10 mm in size located below the common iliac vessels, as assessed by noncontrast computed tomography, were eligible for the study if pain relief was achieved with diclofenac administration within 1 day. Patients who had fever, severe hydronephrosis, acute or chronic renal failure, multiple ureteral stones, a history of open surgery or endoscopic procedures in the urinary tract, diabetes, peptic ulcer, or concomitant treatment with β-blockers, calcium antagonists, or nitrates; those who were pregnant or lactating; and those desiring immediate stone removal were excluded.
After providing written informed consent, the patients were prospectively randomly assigned by use of a computer-generated table into three equal groups of 40 patients each. The randomization table was stored centrally and the group to which each patient was assigned was conveyed to the author after the patient provided consent to participate in the study. Patients in group A were given tamsulosin 0.4 mg once daily, and those in group B were given naftopidil 75 mg once daily. In addition, patients in groups A and B received prednisolone 5 mg once daily for a maximum of 1 week. In both groups, alpha-blockers were continued until stone expulsion or for a maximum of 4 weeks. Patients in group C were given analgesics as and when required. All patients were evaluated by physical examination; serum creatinine; urine culture; plain X-ray of the kidneys, ureters, and bladder (KUB); ultrasonography; and noncontrast computed tomography of the KUB region. All patients presenting with ureteral colic were given pain relief with intramuscular diclofenac. Patients were instructed to filter their urine by using a standard mesh net to detect stone expulsion. The time to expulsion; analgesic use; numbers of hospital visits for pain, follow-up, and endoscopic treatment; and adverse effects of the drugs were noted. The maximum time of follow-up was 4 weeks, after which patients underwent semirigid ureterorenoscopy for removal of stones that were not expelled. The primary outcome studied was the stone expulsion rate. Secondary endpoints studied were time to stone expulsion, number of painful episodes, analgesic use, and self-reported side effects related to medical therapy. Expulsion of stones was confirmed with plain X-ray, ultrasonography, or noncontrast computed tomography.
Normality of the measurable data was tested by use of the Kolmogorov-Smirnov test. All three groups were compared for normally distributed data by analysis of variance followed by a post-hoc test (Student-Newman-Kuels procedure for pairwise comparisons). The skewed data were analyzed for all the three groups by using the Kruskal-Wallis test, followed by the Mann-Whitney U test for comparison. All the classified and categorical data were analyzed for all three groups by using the chi-square test. Because there was multiple testing, using Bonferroni correction, the level of significance was taken as p<0.004. Data were fed into a Microsoft Excel worksheet and were analyzed by using the SPSS ver. 17 (SPSS Inc., Chicago, IL, USA). The sample size of 40 patients in each group was calculated on the basis of an expected 40% spontaneous expulsion rate and a 75% expulsion rate in the α-blocker groups and was enough to achieve a statistical power of 90% at a type I error rate of 5%.
RESULTS
All enrolled patients were able to complete the study protocol. All three groups were comparable with respect to age and sex and the size and side of stones (Table 1). The stone expulsion rate was 70%, 87.5%, and 32.5% in group A, group B, and group C, respectively. The expulsion rates in group A (p=0.002) and group B (p<0.001) were significantly higher than in group C. Although there was a trend toward a higher expulsion rate in group B than in group A (p=0.056), it was not statistically significant. The time to expulsion was comparable between group A and B (p=0.68). The time to expulsion was significantly higher in group C than in groups A (p<0.001) and B (p<0.001). The use of analgesic and the number of episodes of pain was also significantly lower in groups A and B than in group C (p<0.001). The average number of hospital visits for pain and follow-up were 3.2±0.8 (range, 2 to 5), 3.1±0.9 (range, 2 to 5), and 4.0±0.9 (range, 2 to 5) in groups A, B, and C, respectively. These were lowest in group B and highest in group C, but the difference was not statistically significant (Table 2).
TABLE 1.
Patient characteristics in the three groups
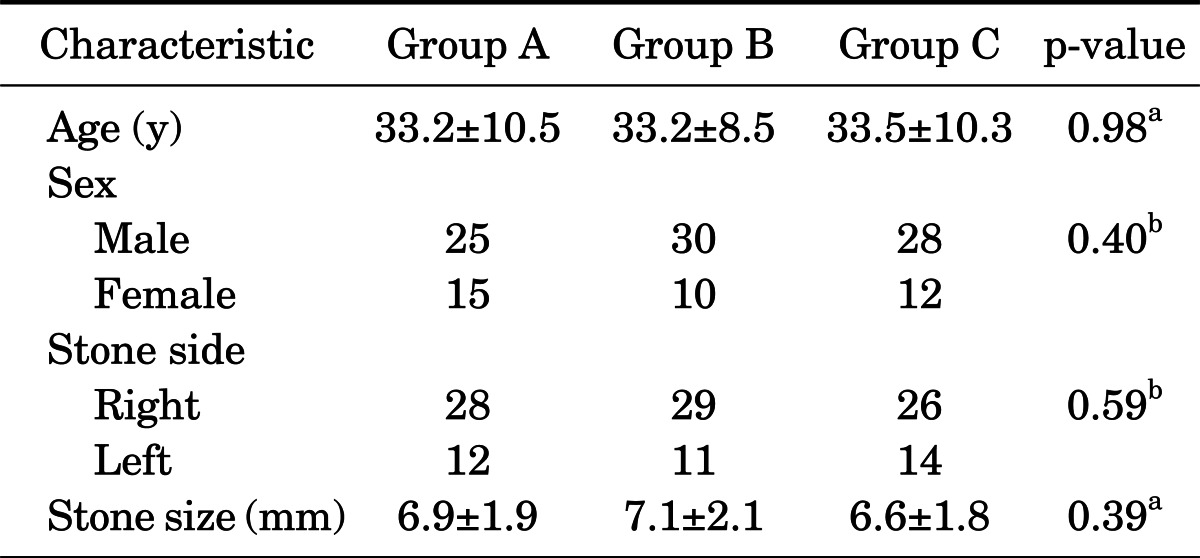
Values are presented as mean±standard deviation.
Group A, tamsulosin+prednisolone; Group B, naftopidil+prednisolone; Group C, watchful waiting.
a:Statistical significance was analyzed by one-way analysis of variance. b:Statistical significance was analyzed by chi-square test.
TABLE 2.
Treatment outcome parameters in the three groups
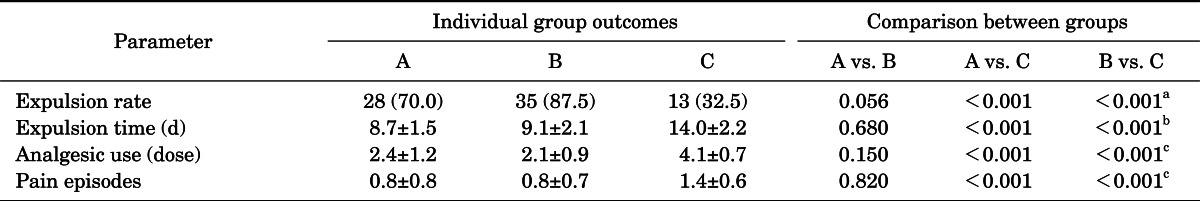
Values are presented as number (%) or mean±standard deviation.
Group A, tamsulosin+prednisolone; group B, naftopidil+prednisolone; group C, watchful waiting.
a:Statistical significance was analyzed by chi-square test. b:Data were analyzed using Kruskal-Wallis test, followed by Mann-Whitney test for comparison between two groups. c:Data were analyzed using analysis of variance, followed by Student-Newman-Kuels method for pair wise comparison.
None of the patients included in the study developed urosepsis. In group A, the expulsion rate in the first week was 12.5% and that in the second week was 65%. No patients expelled stones in the third or fourth week. In group B, the cumulative expulsion rate was 15% in the first week, 85% in the second week, and 87.5% in the third week. In group C, the expulsion rate was 0% in the first week, 12.5% in the second week, and 32.5% in the third week. Forty-six patients did not expel the stones (13, 5, and 27 in groups A, B, and C, respectively) after 4 weeks. These patients underwent ureteroscopic stone removal uneventfully. One patient each in group A and B reported retrograde ejaculation. Dizziness was reported by one patient in group A. None of the other patients reported any side effects related to the drugs.
DISCUSSION
Among all urinary tract stones, 20% present as ureteral stones, of which 70% are found in the lower third of the ureter [9]. The factors influencing the spontaneous expulsion of ureteral stones are stone location, size, number, and shape; spasm in the ureteral smooth muscles; mucosal edema or inflammation; and ureteral anatomy [10,11]. It has been shown that stones less than 6 mm can be observed for spontaneous expulsion [12]. It would seem logical that medical therapy should be used to reduce edema, spasm, and relaxation of smooth muscles. Current therapeutic options for distal ureteral stones include surgical intervention, medical expulsive therapy, and conservative wait and watch approaches. The efficacy of minimally invasive therapies, such as shock wave lithotripsy and ureterorenoscopy, has been proven by several studies [11,13]. However, although such procedures are effective, they are not free from risk or inconvenience, and there are consequent implications such as lowering the quality of life, high cost, and suspension of regular activities [13,14].
A watchful waiting approach can be used in a large number of cases, as demonstrated by several studies that revealed spontaneous passage rates of up to 85% for distal ureteral stones less than 5 mm [15,16]. Watchful waiting does not always result in stone clearance and may be associated with recurrent renal colic [17]. The rate of spontaneous passage diminishes as stone size increases [18]. Thus, to increase the expulsion rate and reduce analgesic consumption, there is a great deal of enthusiasm for adjuvant pharmacological intervention, which can reduce symptoms and facilitate stone expulsion [17-19].
Malin et al. [4] first described the presence of α- and β-adrenergic receptors throughout the entire length of the human ureter and the physiological response (increase in tone and frequency of contraction) of the ureter when exposed to α-adrenoceptor agonists. Later it was found that α-1D and α-1A-adrenoceptors are expressed in significantly larger amounts than the α-1B-adrenoceptor in the human ureter [20]. It was also demonstrated that the distal ureter expresses a greater amount of α-1-adrenoceptor mRNA than do the proximal and middle ureter. Itoh et al. [21] reported that α-1D-adrenoceptor mRNA is more highly expressed than α-1A-adrenoceptor mRNA in each region of the ureter. According to their results, an α-1D-adrenoceptor antagonist can be expected to be more effective for the expulsion of the ureteral stones than an α-1A-adrenoceptor antagonist.
Alpha-1-receptors have been classified into three subtypes (α-1A, α-1B, and α-1D). The α-1A-receptors predominate in the proximal urethra, prostate, and bladder outflow; the α-1B-receptors are distributed widely in the vascular smooth muscles; and the α-1D-receptors are found predominantly in the intramural ureter and detrusor muscle. The distribution of these receptors in the distal ureter is α-1D>α-1A>α-1B [21]. Numerous clinical trials have been performed to investigate the efficacy of the α-1A-selective α-blocker tamsulosin. Most of these studies were randomized and revealed that tamsulosin treatment significantly improves the expulsion rate of medium-sized (3-10 mm) distal ureteral stones. Thus, tamsulosin represents a noninvasive and cost-effective alternative to interventional approaches [6]. Although medical expulsive therapy has become a standard treatment option used by urologists, it is still underused by other physicians in emergency departments [22].
Because α-1D-receptors are found prevalently in the distal ureter [23], these receptors may be a promising target for medical expulsive therapy. Although naftopidil acts on both α-1A- and α-1D-receptors, it has approximately three-fold stronger affinity for the α-1D-receptors than for the α-1A [23]. Naftopidil has been used in the treatment of benign hyperplasia of the prostate and has been proved to be more effective and safe than tamsulosin [7]. Recently, it has shown efficacy in medical expulsive therapy also [8]. It is possible that the effect of α-1D-receptor antagonist on the obstructed ureter is to induce an increase in the intraureteral pressure gradient around the stone, as well as decreased peristalsis below the ureter. It may also cause a decrease in basal and micturition pressures. For this reason, it induces a strong gradient to expel the stone.
We observed a stone expulsion rate of 87.5% with the use of naftopidil. The expulsion rate of naftopidil in previous studies varied from 61% to 90% [8,23,24]. The higher dose of naftopidil (75 mg/d) used in our study group as compared to previous studies [23,24] and the concomitant use of prednisolone could have led to the better expulsion rate in our study than in these previous studies. It was previously shown that the combination of steroid with tamsulosin leads to a higher stone expulsion rate [6]. The better stone expulsion rate as compared to tamsulosin may be due to the three times higher affinity of naftopidil for the α-1D-adrenoceptor than for the α-1A-adrenoceptor [25], which allows it to cause relaxation of both detrusor and ureteral muscles more effectively. Because of the simultaneous detrusor and intramural ureteral relaxation, the compression at the intramural part of the ureter, which is the narrowest part of the ureter that the ureteral calculus has to negotiate, is relieved. We believe that this peculiar action of naftopidil is a major reason for its higher stone expulsion rate compared with tamsulosin, although the difference was not statistically significant.
In our study, the expulsion rate was 70% in patients who received tamsulosin, which was significantly higher than that of the control group (32.5%). Tamsulosin has been shown to have a stone expulsion rate varying from 54% to 100% in previous studies [26]. The time to expulsion in both the tamsulosin and naftopidil groups was similar to that in previous studies [24,27]. The mean time to expulsion with naftopidil monotherapy was 7 to 15 days in previous studies [23,24].
The reported side effects were minimal in our study. This was probably because of the younger study population and the lack of any associated comorbidity. The use of a near physiological dose of prednisolone [28] and the careful exclusion of patients with contraindications to steroids may explain the lack of significant side effects related to steroid use. The 5-mg dose of prednisolone is nearly five times lower than the 30-mg deflazacort dose used in previous studies [29].
Analgesic use in the control group was significantly higher than in the tamsulosin and naftopidil groups. Kinnmen et al. [30] opined that α-blockade may relieve ureteral colic by blocking the C-fibers responsible for mediating pain. Use of α-blockers for expulsion of ureteral stones probably decreases the analgesic requirement in two ways: expulsion of stones, leading to longer stone-free periods, and blockade of C-fibers. It is difficult to assess which of these may be primarily responsible for decreasing the analgesic requirement, because α-blockers are known to be associated with both.
CONCLUSIONS
Medical expulsive therapy using either naftopidil or tamsulosin combined with prednisolone is safe and efficacious compared with watchful waiting for distal ureteral stones. There was a trend toward a better expulsion rate in the group treated with naftopidil, but this needs to be studied further in adequately powered studies.
Footnotes
The authors have nothing to disclose.
References
- 1.Hollingsworth JM, Rogers MA, Kaufman SR, Bradford TJ, Saint S, Wei JT, et al. Medical therapy to facilitate urinary stone passage: a meta-analysis. Lancet. 2006;368:1171–1179. doi: 10.1016/S0140-6736(06)69474-9. [DOI] [PubMed] [Google Scholar]
- 2.Ueno A, Kawamura T, Ogawa A, Takayasu H. Relation of spontaneous passage of ureteral calculi to size. Urology. 1977;10:544–546. doi: 10.1016/0090-4295(77)90097-8. [DOI] [PubMed] [Google Scholar]
- 3.Carstensen HE, Hansen TS. Stones in the ureter. Acta Chir Scand Suppl. 1973;433:66–71. [PubMed] [Google Scholar]
- 4.Malin JM, Jr, Deane RF, Boyarsky S. Characterisation of adrenergic receptors in human ureter. Br J Urol. 1970;42:171–174. doi: 10.1111/j.1464-410x.1970.tb10018.x. [DOI] [PubMed] [Google Scholar]
- 5.Yamaguchi K, Minei S, Yamazaki T, Kaya H, Okada K. Characterization of ureteral lesions associated with impacted stones. Int J Urol. 1999;6:281–285. doi: 10.1046/j.1442-2042.1999.00067.x. [DOI] [PubMed] [Google Scholar]
- 6.Porpiglia F, Vaccino D, Billia M, Renard J, Cracco C, Ghignone G, et al. Corticosteroids and tamsulosin in the medical expulsive therapy for symptomatic distal ureter stones: single drug or association? Eur Urol. 2006;50:339–344. doi: 10.1016/j.eururo.2006.02.023. [DOI] [PubMed] [Google Scholar]
- 7.Nishino Y, Masue T, Miwa K, Takahashi Y, Ishihara S, Deguchi T. Comparison of two alpha1-adrenoceptor antagonists, naftopidil and tamsulosin hydrochloride, in the treatment of lower urinary tract symptoms with benign prostatic hyperplasia: a randomized crossover study. BJU Int. 2006;97:747–751. doi: 10.1111/j.1464-410X.2006.06030.x. [DOI] [PubMed] [Google Scholar]
- 8.Sun X, He L, Ge W, Lv J. Efficacy of selective alpha1D-blocker naftopidil as medical expulsive therapy for distal ureteral stones. J Urol. 2009;181:1716–1720. doi: 10.1016/j.juro.2008.11.118. [DOI] [PubMed] [Google Scholar]
- 9.Wolf JS., Jr Treatment selection and outcomes: ureteral calculi. Urol Clin North Am. 2007;34:421–430. doi: 10.1016/j.ucl.2007.04.010. [DOI] [PubMed] [Google Scholar]
- 10.Wang CJ, Huang SW, Chang CH. Efficacy of an alpha1 blocker in expulsive therapy of lower ureteral stones. J Endourol. 2008;22:41–46. doi: 10.1089/end.2007.0133. [DOI] [PubMed] [Google Scholar]
- 11.Segura JW, Preminger GM, Assimos DG, Dretler SP, Kahn RI, Lingeman JE, et al. The American Urological Association. Ureteral Stones Clinical Guidelines Panel summary report on the management of ureteral calculi. J Urol. 1997;158:1915–1921. doi: 10.1016/s0022-5347(01)64173-9. [DOI] [PubMed] [Google Scholar]
- 12.Tchey DU, Ha YS, Kim WT, Yun SJ, Lee SC, Kim WJ. Expectant management of ureter stones: outcome and clinical factors of spontaneous passage in a single institution's experience. Korean J Urol. 2011;52:847–851. doi: 10.4111/kju.2011.52.12.847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bensalah K, Pearle M, Lotan Y. Cost-effectiveness of medical expulsive therapy using alpha-blockers for the treatment of distal ureteral stones. Eur Urol. 2008;53:411–418. doi: 10.1016/j.eururo.2007.09.012. [DOI] [PubMed] [Google Scholar]
- 14.Gettman MT, Segura JW. Management of ureteric stones: issues and controversies. BJU Int. 2005;95(Suppl 2):85–93. doi: 10.1111/j.1464-410X.2005.05206.x. [DOI] [PubMed] [Google Scholar]
- 15.Hubner WA, Irby P, Stoller ML. Natural history and current concepts for the treatment of small ureteral calculi. Eur Urol. 1993;24:172–176. doi: 10.1159/000474289. [DOI] [PubMed] [Google Scholar]
- 16.Coll DM, Varanelli MJ, Smith RC. Relationship of spontaneous passage of ureteral calculi to stone size and location as revealed by unenhanced helical CT. AJR Am J Roentgenol. 2002;178:101–103. doi: 10.2214/ajr.178.1.1780101. [DOI] [PubMed] [Google Scholar]
- 17.Shokeir AA. Renal colic: pathophysiology, diagnosis and treatment. Eur Urol. 2001;39:241–249. doi: 10.1159/000052446. [DOI] [PubMed] [Google Scholar]
- 18.Borghi L, Meschi T, Amato F, Novarini A, Giannini A, Quarantelli C, et al. Nifedipine and methylprednisolone in facilitating ureteral stone passage: a randomized, double-blind, placebo-controlled study. J Urol. 1994;152:1095–1098. doi: 10.1016/s0022-5347(17)32511-9. [DOI] [PubMed] [Google Scholar]
- 19.Porpiglia F, Destefanis P, Fiori C, Fontana D. Effectiveness of nifedipine and deflazacort in the management of distal ureter stones. Urology. 2000;56:579–582. doi: 10.1016/s0090-4295(00)00732-9. [DOI] [PubMed] [Google Scholar]
- 20.Sigala S, Dellabella M, Milanese G, Fornari S, Faccoli S, Palazzolo F, et al. Evidence for the presence of alpha1 adrenoceptor subtypes in the human ureter. Neurourol Urodyn. 2005;24:142–148. doi: 10.1002/nau.20097. [DOI] [PubMed] [Google Scholar]
- 21.Itoh Y, Kojima Y, Yasui T, Tozawa K, Sasaki S, Kohri K. Examination of alpha 1 adrenoceptor subtypes in the human ureter. Int J Urol. 2007;14:749–753. doi: 10.1111/j.1442-2042.2007.01812.x. [DOI] [PubMed] [Google Scholar]
- 22.Itano N, Ferlic E, Nunez-Nateras R, Humphreys MR. Medical expulsive therapy in a tertiary care emergency department. Urology. 2012;79:1242–1246. doi: 10.1016/j.urology.2011.12.033. [DOI] [PubMed] [Google Scholar]
- 23.Tsuzaka Y, Matsushima H, Kaneko T, Yamaguchi T, Homma Y. Naftopidil vs silodosin in medical expulsive therapy for ureteral stones: a randomized controlled study in Japanese male patients. Int J Urol. 2011;18:792–795. doi: 10.1111/j.1442-2042.2011.02850.x. [DOI] [PubMed] [Google Scholar]
- 24.Zhou SG, Lu JL, Hui JH. Comparing efficacy of α1D-receptor antagonist naftopidil and α1A/D-receptor antagonist tamsulosin in management of distal ureteral stones. World J Urol. 2011;29:767–771. doi: 10.1007/s00345-011-0739-3. [DOI] [PubMed] [Google Scholar]
- 25.Takei R, Ikegaki I, Shibata K, Tsujimoto G, Asano T. Naftopidil, a novel alpha1-adrenoceptor antagonist, displays selective inhibition of canine prostatic pressure and high affinity binding to cloned human alpha1-adrenoceptors. Jpn J Pharmacol. 1999;79:447–454. doi: 10.1254/jjp.79.447. [DOI] [PubMed] [Google Scholar]
- 26.Seitz C, Liatsikos E, Porpiglia F, Tiselius HG, Zwergel U. Medical therapy to facilitate the passage of stones: what is the evidence? Eur Urol. 2009;56:455–471. doi: 10.1016/j.eururo.2009.06.012. [DOI] [PubMed] [Google Scholar]
- 27.Porpiglia F, Ghignone G, Fiori C, Fontana D, Scarpa RM. Nifedipine versus tamsulosin for the management of lower ureteral stones. J Urol. 2004;172:568–571. doi: 10.1097/01.ju.0000132390.61756.ff. [DOI] [PubMed] [Google Scholar]
- 28.Yildiz O, Doganay M, Aygen B, Guven M, Kelestimur F, Tutuu A. Physiological-dose steroid therapy in sepsis [ISRCTN36253388] Crit Care. 2002;6:251–259. doi: 10.1186/cc1498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Nayak S, Acharjya B. Deflazacort versus other glucocorticoids: a comparison. Indian J Dermatol. 2008;53:167–170. doi: 10.4103/0019-5154.44786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kinnman E, Nygards EB, Hansson P. Peripheral alpha-adrenoreceptors are involved in the development of capsaicin induced ongoing and stimulus evoked pain in humans. Pain. 1997;69:79–85. doi: 10.1016/s0304-3959(96)03257-5. [DOI] [PubMed] [Google Scholar]


