Abstract
Background
Patients with early onset neurodegenerative disease can present with a clinical syndrome that overlaps with schizophrenia, and it is not uncommon for these patients to undergo long-term care in psychiatric settings rather than receiving more appropriate care by neurologists specializing in their disease.
Case report
A 35-year old woman who presented with new-onset delusions, eating abnormalities, disorganized behavior, lack of insight, disinhibition, and stereotypical motor behaviors was diagnosed with schizophrenia and institutionalized. Later she was found to have a MAPT tau S356T mutation and a focal pattern of brain atrophy consistent with frontotemporal dementia (FTD).
Conclusion
Physicians should be aware of the potential overlap in symptoms and age of onset between some forms of FTD and schizophrenia, and should include FTD in the diagnostic differential for adult patients with new onset, rapidly progressive personality changes or behavioral symptoms such as binge eating, high levels of social disinhibition, or progressive mutism.
Introduction
Contrary to common clinical assumptions, neurodegenerative disease can begin as early as the third decade of life, and some of these young patients present with isolated neuropsychiatric rather than cognitive symptoms. These cases can exemplify the diagnostic overlap between psychiatric and neurologic disease, as well as the procedural gaps that sometimes occur between psychiatric and neurologic clinical services. While technically these patients present with a psychiatric disorder, the cause of their symptoms is a specific neuropathological disease that in many cases may be identifiable by genetic testing or a careful family history. Symptomatic and even disease-modifying treatments for some of these neurodegenerative diseases are currently in clinical trials and thus it is becoming increasingly urgent that clinicians recognize these “zebras” early in the disease process. Retrospective examination of these patients’ clinical course may yield important information to improve diagnostic accuracy in the future. We report the case of a young woman who was initially diagnosed with schizophrenia in her 30’s, but was found to have a rare genetic mutation in a tau-related gene, which together with a specific pattern of brain atrophy, predict a 3R tauopathy, i.e., frontotemporal lobar degeneration (FTLD) with Pick’s neuropathology.1 This suggests that the more appropriate clinical diagnosis for this patient was behavioral variant frontotemporal dementia (bvFTD), a diagnosis that could have led to an entirely different clinical care plan.
Case History
Ms. A was referred to our tertiary care memory disorders clinic at the age of 43 after an eight-year history of progressive personality, behavioral and language changes. Symptoms began at age 35 when she stole her mother’s wedding ring. When confronted by her mother, Ms. A admitted to taking the jewelry but was indifferent to her mother’s distress and stated that her mother gave her the ring. This same year she was fired from her job due to inappropriate sexual behavior (e.g. grabbing colleagues’ genitals and stating, “You will like it!”). At age 36, Ms. A became self-centered, sexually inappropriate with friends, emotionally distant, and was unconcerned about her significant occupational, financial and personal losses. She began hoarding animal carcasses, compulsively stuffing her mouth with pet food and inedible objects such as paper and gained 30 pounds due to binge eating.
Ms. A did not enter into medical care until age 37 when she was caught shoplifting at a store she had robbed hours earlier, at which time she was jailed and referred for mental health evaluation. At evaluation, Ms. A was delusional and incorrectly claimed she was a park ranger who “saved a little girl from being bitten by a rattle snake. The snake did not bite me as I picked it up and kissed it. I guess the snake knew that I wasn’t afraid of wild life.” She also explained how she had saved a child from sexual assault by showing her breast to the assailant and distracting him. Her physician noted “an overall sense of suspiciousness and [an] absolutely strikingly inappropriate affect in that she is totally unconcerned with having been to jail…she denies having a mental health condition and denies stealing property.” Initially she was diagnosed with delusional disorder and this was later changed to paranoid schizophrenia. Shortly afterwards, the patient underwent psychiatric institutionalization due to increasingly aberrant eating behavior (she ate rapidly and choked on food and inedible objects), self-neglect (e.g. unwillingness to maintain hygiene), and dangerous behavior (e.g. walking through traffic, shoplifting, hypersexuality). During the course of her psychiatric treatment and institutionalization, the patient was started on antipsychotic medications and underwent ineffective trials of olanzapine (max daily doses: 40mg), sertraline (50 mg), clozaril (500mg), risperidone (5mg), and ziprasidone (440mg). While institutionalized, Ms. A developed bladder incontinence, gained an additional 20 pounds, and stopped engaging in even basic self-care, eventually requiring constant one-on-one supervision. She became mute, which clinicians attributed to paranoiaand the effects of lorazapam. She was put in group therapy to encourage her to speak and the lorazapam was tapered, but her mutism remained constant. Ms. A continued to receive social support from her mother, but she lost contact with her two brothers who were angry at her because of the grief her disinhibited and criminal behavior caused their family.
A developmental history revealed that Ms. A was born prematurely and stayed in the NICU two days. As an infant she had pneumonia and was diagnosed with “cough-induced seizure disorder”, but achieved normal developmental milestones by 9 months of age. She completed a master’s degree in anthropology, worked as an office assistant and was a successful, published poet. She had no history of head injury, psychiatric illness or significant substance use. Family history was significant for unknown psychiatric illnesses in the patient’s father, two paternal aunts, and a paternal grandmother, as well as two paternal cousins who both were diagnosed with paranoid schizophrenia and both committed suicide.
Ms. A’s mother was concerned that her daughter’s treatment resistant, progressive deterioration was dissimilar to other patients with schizophrenia at the institution, and successfullyfought for her to receive neurological evaluation a year after Ms. A had been institutionalized. On examination at our clinic, Ms. A was not depressed, aggressive, or agitated but was occasionally anxious and irritable. She chewed gum, violated interpersonal space by leaning inappropriately close to the examiner, rocked her body back and forth in her chair and played with a toy cat, which she petted and hid in her sleeves. Vital signs and general physical exam were unremarkable. Her lack of speech limited neurological examination, although her motor functioning showed normal bulk and power in all extremities. She walked with a narrow base and normal stride, but with decreased arm swing bilaterally. There was slight increase in tone in the upper extremities bilaterally.
A brief standard neuropsychological battery was attempted with Ms. A, but she provided only minimal verbal responses, had poor task persistence even with maximal redirection by the examiner, and was highly stimulus-bound and perseverative on written and visuospatial tasks. She was able to read 6/10 regular and irregular words out loud, repeated 1/5 phonemically complex phrases, named colors on demand, and named 1/15 objects (“flower”) on a confrontation naming task, saying nonsense words or becoming echolalic on the other items. She copied many gestalt and detail elements of a complex figure (8/17 points), despite obtaining a score of 0/30 on the MMSE.
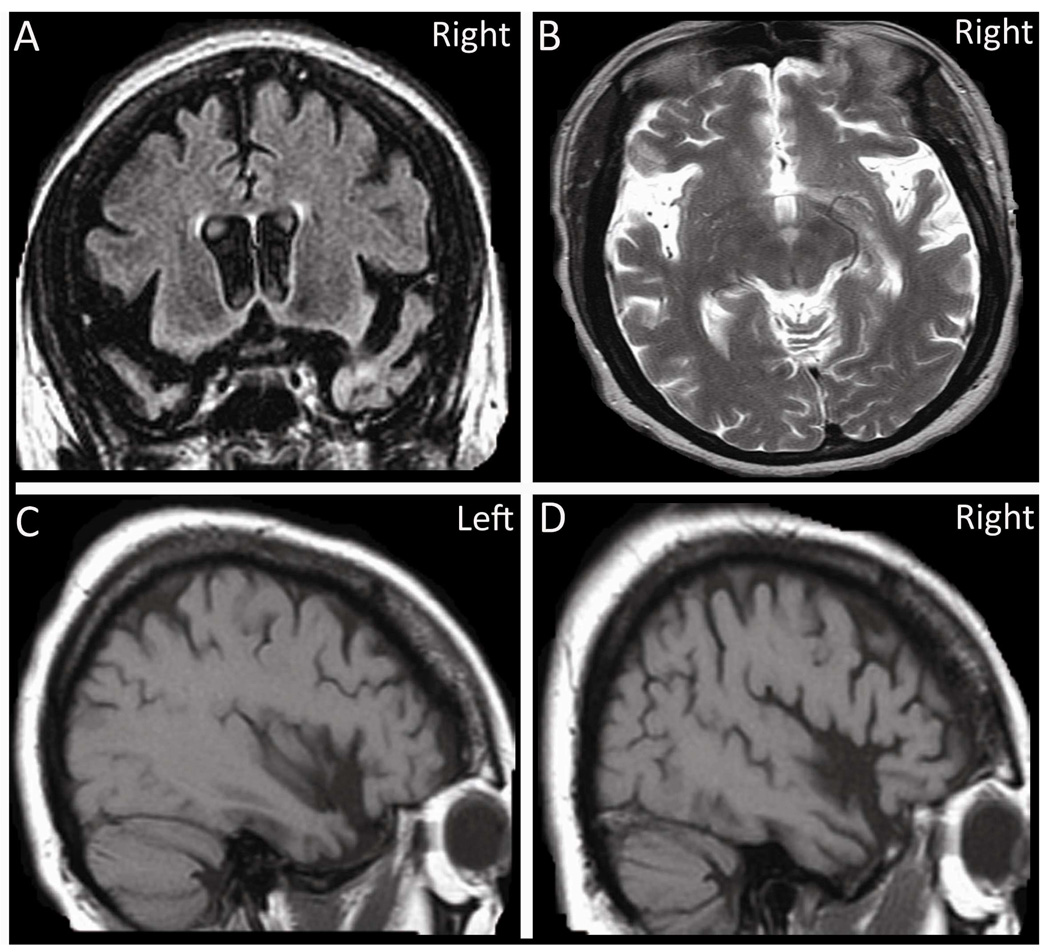
A structural brain MRI showed severe bilateral frontal orbital and insular atrophy (Fig 1). Laboratory studies of serum electrolytes, and liver and thyroid function were within normal range. RPR was negative. Genetic testing showed a MAPT tau T>A mutation in exon 12, predicted to cause the amino acid change S356T. Based on the patient’s progressive cognitive, behavioral and personality changes, and further supported by the tau mutation and characteristic pattern of medial frontal-anterior temporal brain atrophy, she was given a clinical diagnosis of behavioral variant frontotemporal dementia (bvFTD), with a predicted neuropathology of FTLD-Pick’s, a 3-repeat tauopathy.
Figure 1.
Discussion
We report the case of a young woman with bvFTD and a rare tau-mutation who was initially diagnosed with schizophrenia, but for whom a more accurate clinical diagnosis would have been bvFTD because the neuropathological cause of her symptoms is a known neurodegenerative disease. The majority of individuals presenting in their 30’s with new-onset psychotic symptoms do not have identifiable neurologic diseases, and are thus appropriately diagnosed and treated for schizophrenia. With Ms. A, the clinical diagnosis of schizophrenia led to a long psychiatric institutionalization involving inappropriate behavioral and psychotropic treatments and significantly increased discord in her family, which substantially improved after they learned the genetic, neurodegenerative nature of her condition and received disease-appropriate counseling. Early, accurate diagnosis could have ensured that bvFTD-specific psychotropic and behavioral interventions would be used to manage her symptoms, and the progression of her symptoms could have been better predicted which would have helped her family cope. Though there are currently no cures for schizophrenia or bvFTD, Ms. A may have been a candidate for one of the new clinical trials that are currently underway to treat neurodegenerative tauopathies2 had her condition been identified earlier. The new treatment options that are rapidly appearing raise the stakes for clinicians to provide the most accurate clinical diagnosis possible for a patient presenting with a new-onset neuropsychiatric disorder.
Distinguishing between bvFTD and schizophrenia is a diagnostic challenge, particularly in a young patient. Symptoms of bvFTD may include sexual disinhibition, poor hygiene, compulsivity, anti-social behavior, loss of insight, diminished executive function and loss of empathy,3, 4 which may be mistaken for symptoms of schizophrenia.4 Additionally, while psychosis is only reported in 10% of bvFTD cases,5 Ms. A demonstrates that psychosis in patients with bvFTD may increase a clinician’s suspicion of schizophrenia and delay neurological referral. The grandiose and paranoid nature of her delusions is typical for what is seen with bvFTD.The incidence of bvFTD before age 45 is not known, but it is presumably less than 3.5–4.8 per 100,000 people, the incidence observed in the age group 45–64.6,7 While rare, bvFTD onset before age 45 is reported, with some of the earliest cases occurring in patients’ mid-twenties.8 Often, these early-onset cases are the result of a genetic mutation transmitted in their family. The incidence of first-onset schizophrenia between age 30 and 45 is estimated to be 37.5–96.0 per 100,000 people,9 thus is more common than bvFTD during mid-life.6 Thus, a diagnosis of schizophrenia in a young patient with new onset behavioral symptoms is statistically more common, which may bias clinicians against recognizing bvFTD.
A family history of a psychotic illness is considered supportive of a diagnosis of schizophrenia, however, it is now recognized in some families with mutations in tau, familial schizophrenia was the first diagnosis.8 In retrospect, patients with familial bvFTD often demonstrate a highly penetrant, autosomal-dominant pattern of inheritance,10 and it is unlikely that bvFTD would have been accurately diagnosed in previous generations due to lack of medical attention to this disease until recent years. Thus, a family history of a highly penetrant psychotic illness may be equally likely to indicate familial bvFTD or schizophrenia. In fact, the genetic mutation seen in Ms. A was previously reported to cause early onset bvFTD in a family in which multiple individuals were incorrectly diagnosed with schizophrenia.8 Ms. A’s symptoms included delusions, disorganized behavior, lack of insight, disinhibition, and repetitive behavior, which in conjunction with her young age and family history of apparent psychiatric illness, suggest that the degree to which the clinical syndrome of bvFTD can overlap with schizophrenia should not be underestimated.
Some differences may be discerned. Although in young, familial cases of bvFTD the diagnostic markers distinguishing bvFTD and schizophrenia are elusive, by aggregating the natural histories of this case and a series of other similar cases recently appearing in the literature, it may be possible to delineate symptom patterns which suggest FTLD neuropathology as the source of a patient’s symptoms. Retrospectively, qualitative analysis of Ms. A’s eating abnormalities, the specific nature of her disinhibition and decrease in speech, and the rapid, treatment-resistant progression of her symptoms were all more suggestive of bvFTD than schizophrenia.
First, eating abnormalities are well-characterized features of bvFTD1, 11 and Ms. A’s early binge eating, weight gain and compulsive desire to eat inedible objects may have been a useful diagnostic clue that she suffered from bvFTD. Pica is rare in schizophrenia12 and there is at least one other report of a young patient with pica being diagnosed with schizophrenia but actually having bvFTD.13 Also unlike patients with schizophrenia, patients with bvFTD often show a qualitative change in the manner of food intake, which can include overstuffing their mouths to the point of gagging, and being unable to stop themselves from eating long after they feel full as long as food remains in front of them.11 Overeating and weight gain when present in schizophrenia are typically due to physiological side effects from atypical anti-psychotic medications. Ms. A’s compulsive overeating, weight gain and pica began prior to the initiation of these medications, and taking these drugs likely merely exacerbated Ms. A’s already profound eating disturbances.
Second, Ms. A’s social disinhibition, i.e., her tendency to say and do socially inappropriate and even shocking things without regard to social context (e.g., at work), was a profound and early symptom in her illness. Though patients with schizophrenia can certainly be inappropriate, particularly when speaking out of a delusional belief system, the broad degree of disregard for all social rules seen in Ms. A is more consistent with bvFTD than schizophrenia. Even when compared directly, patients with bvFTD are rated by caregivers as significantly more disinhibited than are patients with schizophrenia.14
Third, Ms. A’s steady decline in speech production and her eventual near-muteness was attributed to social paranoia and to medications, but this deterioration progressed despite adding support groups to encourage speech and tapering of her medications. Patients with bvFTD are known to have progressively decreased speech output and often become mute, though this is typically a form of “elective mutism” due to apathetic disengagement and failure to organize a speech response, rather than a loss of motor speech production or capacity for language comprehension.1 Although patients with schizophrenia are often characterized by decreased speech output,14 these patients rarely become permanently mute. Finally, Ms. A’s rapid, treatment-resistant progression over 8 years is distinct from the typically slow decline and long periods of plateaued functioning seen in younger patients with schizophrenia. Furthermore, Ms. A’s symptoms did not respond at all to multiple antipsychotic drug trials, which may have been a clue that she did not have a typical schizophrenia syndrome.
The accurate diagnosis of neurodegenerative diseases, particularly in early onset cases, is important for appropriate treatment and clinical care. Patients like Ms. A present a particular challenge to physicians, who must carefully weigh the benefit of a costly neurological referral versus the risk of an incomplete diagnostic work-up leading to misdiagnosis and inappropriate treatments, such as antipsychotic medications that may worsen cognitive symptoms.15 Importantly, patients with bvFTD are prone to harsher consequences of an erroneous diagnosis such as inappropriate imprisonment, because bvFTD challenges the legal notion of “insanity”.16 Clues that merit further neurological work-up in patients diagnosed with schizophrenia include profound eating abnormalities before the administration of psychotropics, high levels of social disinhibition, severe poverty of speech, the presence of a family history of a highly penetrant, autosomal dominant psychiatric illness (which could represent a repeatedly misdiagnosed neurodegenerative disease) and most importantly, rapidly progressive symptoms which may be unresponsive to medications. Physicians should be aware of the potential overlap in symptoms and age of onset between bvFTD and schizophrenia, and should include bvFTD in the diagnostic differential of adult patients with new symptoms of behavioral and personality change.
Acknowledgments
Funding Support: This research was supported in part by the National Institute on Aging (NIA) grants 5-P01 AG19724 and P50 AG023501, the State of California, Alzheimer's Disease Research Center of California (ARCC) grant 03-7527.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Declaration of interest for all authors: All authors report no competing interests.
Location: University of California San Francisco Memory and Aging Center, Department of Neurology, 350 Parnassus Avenue, San Francisco, CA 94143.
Contributor Information
Baber K. Khan, University of California San Francisco, Memory and Aging Center, Department of Neurology, 350 Parnassus Avenue, San Francisco, CA 94143.
Josh D. Woolley, University of California San Francisco, Langley Porter, Department of Psychiatry, 401 Parnassus Avenue, Room 159, San Francisco, CA 94143..
Steven Chao, University of California San Francisco, Memory and Aging Center, Department of Neurology, 350 Parnassus Avenue, San Francisco, CA 94143..
Tricia See, University of California San Francisco, Memory and Aging Center, Department of Neurology, 350 Parnassus Avenue, San Francisco, CA 94143..
Anna M. Karydas, University of California San Francisco, Memory and Aging Center, Department of Neurology, 350 Parnassus Avenue, San Francisco, CA 94143.
Bruce L. Miller, University of California San Francisco, Memory and Aging Center, Department of Neurology, 350 Parnassus Avenue, San Francisco, CA 94143..
Katherine P. Rankin, University of California San Francisco, Memory and Aging Center, Department of Neurology, 350 Parnassus Avenue, San Francisco, CA 94143..
References
- 1.Cairns N, Bigio E, Mackenzie I, et al. Neuropathologic diagnostic and nosologic criteria for frontotemporal lobar degeneration: consensus of the Consortium for Frontotemporal Lobar Degeneration. Acta Neuropathol. 2007;114(1):5–22. doi: 10.1007/s00401-007-0237-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Boxer A. A 12 Week Randomized Placebo Controlled Pilot Clinical Trial of Davunetide fot FTLD with Predicted Tau Pathology (CBD, PSP, PNFA) [abstract]. American Academy of Neurology Annual Meeting; Tuesday April 12th, 2011; Hawaii: Scientific Platform Session; 2011. Abstract number 003. [Google Scholar]
- 3.Weder ND, Aziz R, Wilkins K, et al. Frontotemporal dementias: a review. Ann Gen Psychiatry. 2007 Jan 1;6(15):1–10. doi: 10.1186/1744-859X-6-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Woolley J, Khan B, Murthy N, et al. The Diagnostic Challenge of Psychiatric Symptoms in Neurodegenerative Disease: Rates of and Risk Factors for Prior Psychiatric Diagnosis in Patients with Early Neurodegenerative Disease. J. Clin Psych. doi: 10.4088/JCP.10m06382oli. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Swartz R, Miller B, Benson D, et al. Behavioral Phenomenology in Alzheimer's disease, frontotemporal dementia and late-life depression: a retrospective analysis. J Geriatr Psychiatry Neurol. 1997;10:67–74. doi: 10.1177/089198879701000206. [DOI] [PubMed] [Google Scholar]
- 6.Knopman DS, Petersen RC, Edland SD, et al. The incidence of frontotemporal lobar degeneration in Rochester, Minnesota, 1990 through 1994. Neurology. 2004 Feb 10;62(3):506–508. doi: 10.1212/01.wnl.0000106827.39764.7e. [DOI] [PubMed] [Google Scholar]
- 7.Mercy L, Hodges JR, Dawson K, et al. Incidence of early-onset dementias in Cambridgeshire, United Kingdom. Neurology. 2008 Nov 4;71(19):1496–1499. doi: 10.1212/01.wnl.0000334277.16896.fa. [DOI] [PubMed] [Google Scholar]
- 8.Momeni P, Wickremaratchi MM, Bell J, et al. Familial early onset frontotemporal dementia caused by a novel S356T MAPT mutation, initially diagnosed as schizophrenia. Clin Neurol Neurosurg. 2010;112(10):917–920. doi: 10.1016/j.clineuro.2010.07.015. [DOI] [PubMed] [Google Scholar]
- 9.Vanasse A, Courteau J, Fleury M-J, et al. Treatment prevalence and incidence of schizophrenia in Quebec using a population health services perspective: different algorithms, different estimates. Soc Psychiatry Psychiatr Epidemiol. 2011 doi: 10.1007/s00127-011-0371-y. E-Pub. [DOI] [PubMed] [Google Scholar]
- 10.Chen-Plotkin A, Martinez-Lage M, Sleiman P, et al. Genetic and clinical features of progranulin-associated frontotemporal lobar degeneration. Arch Neurol. 2011;68(4):488–497. doi: 10.1001/archneurol.2011.53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Woolley J, Gorno-Tempini M, Seeley W, et al. Binge eating is associated with right orbitofrontal-insular-striatal atrophy in frontotemporal dementia. Neurology. 2007;69(14):1423–1433. doi: 10.1212/01.wnl.0000277461.06713.23. [DOI] [PubMed] [Google Scholar]
- 12.Neil J, Horn T, Himmelhoch J. Psychotic pica, nicotinism, and complicated myocardial infarction. Dis Nerv Syst. 1977;38(9):724–726. [PubMed] [Google Scholar]
- 13.Stone J, Griffiths TD, Rastogi S, et al. Non-picks frontotemporal dementia imitating schizophrenia in a 22-year old man. J Neurol. 2003;250:369–370. doi: 10.1007/s00415-003-0989-0. [DOI] [PubMed] [Google Scholar]
- 14.Ziauddeen H, Dibben C, Kipps C, et al. Negative schizophrenic symptoms and the frontal lobe syndrome: one and the same? Eur Arch Psychiatry Clin Neurosci. 2011;261:59–67. doi: 10.1007/s00406-010-0133-y. [DOI] [PubMed] [Google Scholar]
- 15.Liperoti R, Pedone C, Corsonello A. Antipsychotics for the treatment of behavioral and psychological symptoms of dementia (BPSD) Curr Neuropharmacol. 2008;6(2):117–124. doi: 10.2174/157015908784533860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mendez M. The Unique Predisposition to Criminal Violations in Frontotemporal Dementia. J Am Acad Psychiatry Law. 2010;38:318–323. [PMC free article] [PubMed] [Google Scholar]