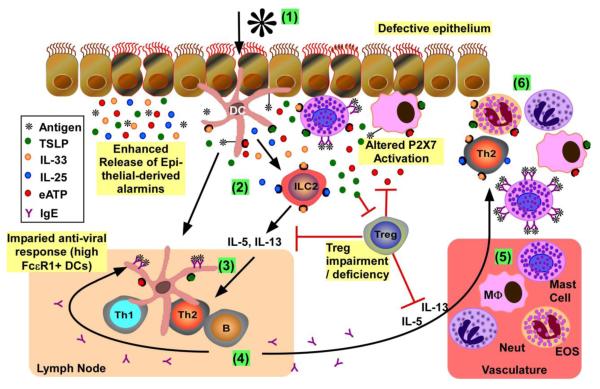
Figure 1. Overview of mucosal immune response to allergens and viruses in atopic asthma.
(1) Initial activation of epithelium and resident innate immune cells: Allergens and/or viruses activate epithelium to induce release of mediators, including alarmins (e.g., TSLP, IL-25, IL-33 and ATP). When epithelia are damaged, there is increased epithelial-mediated alarmin release together with exposure of resident immune cells (e.g., DCs, macrophages, mast cells) to pathogens to further promote pro-inflammatory mediator release. Resident antigen presenting cells (i.e., DCs, macrophages) process and present antigens to activate the adaptive immune response. Mast cells with bound IgE to FcεR1 can bind allergens, inducing FceR1 crosslinking and mediator release (e.g., histamine, TSLP, ATP). Released ATP from mast cells and/or damaged cells activates purinergic receptors on the surface of multiple immune cells (e.g., DCs, macrophages, mast cells) to further promote pro-inflammatory mediator release; the availability of active ATP for purinergic receptor binding is regulated by Tregs. (2) DC skewing and type 2 ILC (ILC2) expansion: Exposure of DCs to IL-33 and TSLP skews the DCs to support differentiation of naive T cells to Th2 in draining lymph nodes. IL-25 and IL-33 induce the maturation and activation of type 2 ILCs, which subsequently release IL-5 and IL-13. Tregs can inhibit the release of Th2 cytokines, but are suppressed by TSLP. (3) Th2 differentiation: The combination of primed DCs and released Th2-promoting cytokines (i.e., IL-4, IL-5, IL-13) lead to the maturation/activation of Th2 lymphocytes in the draining lymph nodes. (4) IgE production: Th2 cells induce B cell immunoglobulin isotype switching, leading to the release of antigen-specific IgE. Increased expression of FceR1 on DCs is inversely related to antiviral (i.e., IFN release) responses. (5) Recruitment of pro-inflammatory leukocytes from vasculature: Release of aforementioned mediators potentiates the release of chemokines from activated innate immune cells/epithelium to promote immune cell recruitment from the vasculature. (6) Chronic Inflammation: Recruited immune cells release more proinflammatory mediators, leading to exaggerated and chronic cellular inflammation.