Abstract
Purpose
To understand the journey of care in the prevention and management of secondary health conditions (SHCs) following spinal cord injury (SCI).
Method
This was a case study design with ‘Ontario’ as the case. The Network Episode Model was used as the conceptual framework. Data sources included in depth interviews with persons with SCI, care providers, and policy and decision makers. Document analysis was also conducted on relevant materials and policies. Key informants were selected by purposeful sampling as well as snowball sampling to provide maximum variation. Data analysis was an iterative process and involved descriptive and interpretive analyses. A coding structure was developed based on the conceptual framework which allowed for free nodes when emerging ideas or themes were identified.
Results
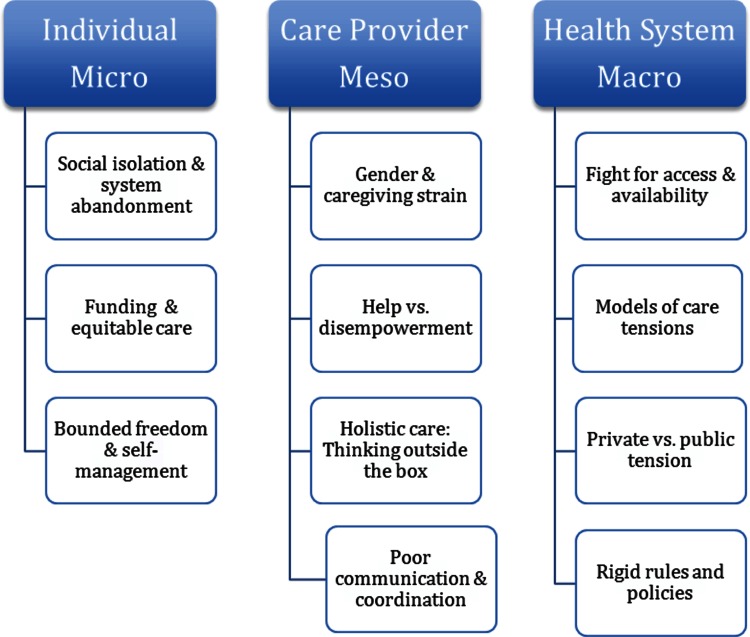
Twenty-eight individuals were interviewed (14 persons with SCI and 14 persons representing care providers, community advocacy organization representatives, system service delivery administrators and policy-makers). A major over-arching domain that emerged from the data was the concept of ‘fighting’. Eleven themes were identified: at the micro-individual level: (i) social isolation and system abandonment, (ii) funding and equitable care, (iii) bounded freedom and self-management; at the meso care provider level: (iv) gender and caregiving strain, (v) help versus disempowerment, (vi) holistic care-thinking outside the box, (vii) poor communication and coordination of care; and at the macro health system level: (viii) fight for access and availability, (ix) models of care tensions, (x) private versus public tensions and (xi) rigid rules and policies.
Conclusions
Findings suggest that the journey is challenging and a persistent uphill struggle for persons with SCI, care providers, and community-based advocates. If we are to make significant gains in minimizing the incidence and severity of SHCs, we need to tailor efforts at the health system level.
Implications for Rehabilitation
Secondary health conditions are problematic for individuals with a spinal cord injury (SCI).
This study aimed to understand the journey of care in the prevention and management of secondary health conditions (SHCs) following SCI.
Findings suggest that the journey is challenging and a persistent uphill struggle for persons with SCI, care providers, and community-based advocates.
All stakeholders involved recognized the disparities in access to care and resources that exist within the system. We recommend that if we are to make significant gains in minimizing the incidence and severity of SHCs, we need to tailor efforts at the health system level.
Keywords: Health services, secondary health conditions, spinal cord injury
Introduction
A spinal cord injury (SCI) is a chronic condition that involves an insult to the spinal cord resulting in significant motor, sensory and/or bowel and bladder impairments. Advances in early acute care and rehabilitation have contributed to increased life expectancy and frequency of community discharge [1]; however, these individuals continue to be at risk of serious secondary health conditions (SHCs) [2–5].
SHCs can include the following: respiratory disease, urinary tract infections (UTIs), heart disease, osteoporosis, overuse upper extremity injuries, sleep disorders, sexual disorders, suicides, pressure ulcers, chronic pain, fatigue, depression and/or respiratory infection [2,6]. Despite the fact that many of these SHCs are potentially preventable, they are purported to be key contributors for ED visits, re-hospitalizations and/or death in the post-acute phase [4,7]. Furthermore, SHCs continue to be problematic in approximately 20% of this population [8].
Given the reduced lengths of inpatient rehabilitation, persons with SCI often require outpatient care to manage SHCs that have not stabilized at the time of index discharge [9,10]. Indeed, this shift from inpatient care to community care has led to an increased role of formal care provision (paid medical professionals), as well as informal caregiving (unpaid providers such as family, friends, community organizations) to assist persons in the community [9,11,12]. These high utilization rates of health care services [7,13–15] suggest that care needs in the community are not being met for this population. Unmet care needs in primary health care, such as lack of information/education [10,16], psychosocial care [17], sexual and reproductive health [18], and health promotion have been previously identified in a few studies for persons with a SCI [10,17–21]. Further, previous disability research has identified structural and process barriers in the community that influence the extent to which health care needs are met [9,22–24]. Structural and physical barriers relate to the access (e.g. inaccessibility of office facilities, transportation, diagnostic services) and availability (e.g. absence of services) of services; whereas process barriers are obstacles that an individual may encounter with the health service delivery process such as inadequate services (lack of lifts or transfer expertise), and fragmentation of services [22,24].
Overall, there is a paucity of research that has examined unmet needs for persons with SCI living in the community [21], and in particular, very few that have examined factors related to the prevention and management of SHCs beyond the bio-medical focus [25,26]. Most of the research to date examining SHCs has been narrow in scope lacking the examination of broader social, community and environmental/health system factors [25], such as access, availability, satisfaction of service delivery, and social networks [26]. These factors may play a role in the development of SHCs, health care utilization patterns, journey of care, and outcomes and warrant further investigation [25–27].
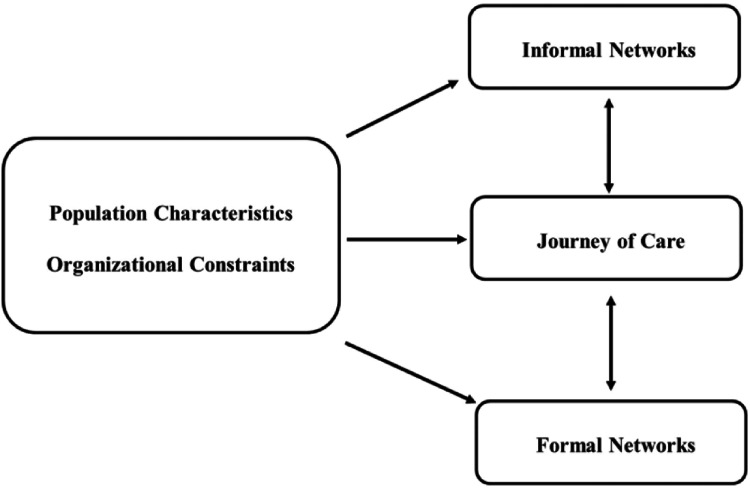
In other vulnerable populations with high health care utilization, such as mental health, investigation of the social context has been useful in understanding the journey of care [28–34]. In particular, Pescosolido’s (1991) Network Episode Model (NEM; see Figure 1) has been used as a conceptual guide in the mental health literature to understand the interactions at the micro level (individual), meso level (care networks), and macro level (health systems) with the overall journeys of health care (referred to as ‘illness career’ in Pescosolido’s model) [35]. The NEM has four dynamic domains, social context (sociodemographic characteristics or the organizational/health system constraints), social support system (informal networks), the treatment system (formal networks) and the illness career (journey of care). Networks of care are conceptualized by structure (e.g. size), content (strength of relationships, attributes of relationship) and functions (the outcome of interaction such as advice, physical or emotional assistance, satisfaction with relationship).
Figure 1. .
Conceptual framework based on Network Episode Model.
Understanding these dynamic interconnected factors such as the structures and roles of care networks and their overall function are important, especially for populations that frequently interact with the health care system [29,30]. Individuals who have suffered a SCI who are living in the community are one such population.
Currently, there is a gap in the literature pertaining to understanding the journey of care related to SHCs for persons living in the community with a SCI. Most research has examined non-modifiable bio-medical variables (such as age, level of injury, mechanism of injury) as predictors of SHCs [25,26]. There is a need to examine more contextual process-related factors to better understand the prevention and management of SHCs [9,25,26]. Despite the relatively low prevalence of SCI, the burdens imposed on the individual, care providers, and health care system are significant as demonstrated by high health care utilization, decreased quality of life, and considerable financial costs [25,36,37]. While we know that SHCs are likely influencing health care use, the paucity of research that has examined these issues in depth highlights that we have a poor understanding of what factors at the micro level (individual), meso level (care provider) and macro (health system) level, may be associated with SHCs development and persistence. There is a need to comprehensively examine the journey of care related to SHCs and factors related to their onset in a broader social context if any significant gains are to be made in minimizing their occurrence [25,26].
Therefore, in light of the importance of this topic, this paper sought to address the existing research gap by understanding the journey of care of persons with SCI related to SHC prevention and/or management. The primary objectives of this study were to describe the journey of care related to the prevention and/or management of SHCs for community-dwelling persons with SCI and to understand factors at the micro (individual), meso (care provider) and macro (health system) level that may influence the journey of care.
Methods
Case study design
A single exploratory case study design was used to understand the journey of care related to SHCs and the influence of informal and formal networks, health system and policies on this care. Case study design is ideal for understanding a phenomenon in complex detail and gaining insight into the contextual factors that may be related to the research question [38]. For this research question, the province of Ontario was defined as the ‘case’ under inquiry. The province of Ontario is situated in central Canada and has a population of approximately 13 million inhabitants [39]. Health care is publicly funded in Canada. Specifically within Ontario, the Ministry of Health and Long-Term Care (MOHLTC) provides publicly funded health care for medically necessary hospital and physician services.
Conceptual framework
Pescosolido’s (1991) NEM was used to guide the research as this model acknowledges the interdependency and social context that exists between individuals and interactions with care providers and the health care system (refer to introduction).
Theoretical position
The theoretical approach underlying this study was that of relativist ontology; that is, a priori knowledge helped inform assumptions but allowed for emerging themes to arise [40]. The paradigm guiding this research question was a naturalistic interpretive one. This multi-lens approach was concerned with understanding the subjective, complex, and contextual experiences of participants [41], which consequently helped inform and reshape knowledge gained from the research inquiry [42]. Further, principles from Thorne’s interpretive description methodology facilitated the scientific inquiry, as this approach allowed for a priori assumptions (e.g. network episode theory) to be synthesized with knowledge gained from data, as well as other theoretical and contextual health services clinical knowledge [42].
Key informant interviews
Semi-structured key informant interviews provided the primary source of data. Key informants included persons with a SCI living in the community, formal and informal care providers, case managers, administration/executive managers, policy-makers and decision makers. The recruitment strategy included purposeful snowball sampling for maximum variation in stakeholder experiences [38]. In particular for persons with SCI, we specifically aimed to have fair representation across gender, level of injury (cervical, thoracic, lumbar), and mechanism of injury (traumatic and non-traumatic), as well as socioeconomic status/funding source for health care services (private payments from motor vehicle accident compensation, public payment for services). Key informant interviews were conducted in two phases. The first phase involved interviews with persons with a SCI recruited in the community by advertising the study via the Canadian Paraplegic Association (CPA)-Ontario division’s website and email distribution. The second phase of interviews involved formal and informal care providers, case managers, and policy/decision makers. A preliminary list of key informants for this phase was developed by the research team and increased with snowball sampling techniques. In this second phase, key informants were those individuals with detailed knowledge of processes involved in managing SHCs for individuals with SCI and were not directly connected to phase I participants.
Document analysis
In addition to key informant interviews, documents were reviewed to gain a better understanding of the health system context for individuals with SCI living in Ontario. These documents provided data to assist with comparing and contrasting data obtained from key informant data. Considerable efforts were made to review documents from multiple sources (gray literature, websites, and brochures). Participants were also invited to suggest any relevant documents that would help inform the research inquiry.
Informed consent
Approval for this study was obtained from the University Health Network Research Ethics Board, as well as the University of Toronto. All participants provided informed consent prior to the interview.
Data collection
Phase I and phase II
Phase I interviews were conducted with persons with a SCI and phase II with care providers, managers, policy-makers, and decision makers. The interview process involved using open-ended questions and probes (see Tables I–II for open-ended questions). Due to geographical and potential accessibility limitations, the interviews were conducted over the telephone and audio-recorded. Phase I interviews ranged from 60 to 90 min in length and the second phase ranged from 30 to 60 min in length. These interviews were conducted by telephone and audio-recorded.
Table I. .
Phase I Interview guide for open-ended questions with participants with SCI.
| 1 | What have been your experiences with your health care in the community? |
| Probes: What made your health care experience easier? Harder? | |
| 2 | What have been your experiences with care related to prevention and/or management of secondary complications? |
| Probes: What made it easier? Harder? | |
| 3 | What has been the role of your informal social networks (friends/family) related to secondary complications? |
| 4 | Is there anything else you would like to mention that we have not had the opportunity to discuss? |
Additional probes were used to facilitate discussion if needed such as “Can you tell me more about that? Can you speak more about the process? How so?”
Table II. .
Phase II interview guide for open-ended questions with care providers, managers, policy-makers.
| 1 | Would you be able to tell me a little bit about your professional role? |
| 2 | What are some important barriers in preventing and/or managing secondary health conditions? |
| 3 | What are some facilitators in preventing and/or managing secondary health conditions? |
| 4 | What are some strategies and/or solutions that might help assist the prevention and/or management of secondary health conditions in the community? |
Additional probes were used to facilitate discussion if needed such as “Can you tell me more about that? Can you speak more about the process? How so?”
Data analysis
All interviews were audio-recorded and transcribed verbatim. Data analysis was an iterative constant comparative process involving descriptive and interpretive analyses [38,40,43]. Using template analysis approach [44], a flexible coding structure was developed based on our conceptual framework (population characteristics, social networks, journey of care) which allowed for free nodes when emerging ideas or themes were identified. After each interview, the principal investigator (SG) wrote detailed reflexive notes on major emerging themes that were later discussed in detail with research investigator (SJ). The principal investigator (SG) coded all transcribed interviews to generate initial codes. The other investigators (SJ, LLC, CC, TC and MM) independently reviewed a sample and compared emergent themes. The investigators reviewed and discussed these developing themes at investigator meetings. Based on the emerging themes identified in phase I, the investigators identified significant tensions and an over-arching ‘fighting’ concept throughout the themes. Based on these reflections, the principal investigator (SG) analyzed the themes from both phases I and II together with the perspective of ‘fighting’ and discussed in weekly meetings with research investigator (SJ). Themes were then organized into ‘micro’, ‘meso’, and ‘macro’ categories based on the original NEM. Data management was facilitated using NVivo9 qualitative analysis computer software.
Assurance of quality
We followed Lincoln and Guba’s principles of trustworthiness [41] as well as Yin’s validity guidelines for case methods [38]. Theoretical saturation, constant comparative analysis, trustworthiness and validity checks provided assurance of data quality and rigor [38,41].
Results
In phase I, fourteen interviews were conducted with individuals who had a SCI (see Appendix D for more clinical characteristics). The majority of participants (n = 13) identified having significant problems with SHCs in the past year. Fourteen participants were also interviewed in phase II (see Table III for stakeholder representation). These participants represented the following categories, care providers, community advocacy organization representatives, system service delivery administrators and policy-makers across Ontario. Case documents were collected from the participants, community advocacy organizations and various other websites (see Appendix A for a list of documents reviewed). The documents reviewed triangulated with the themes discussed below.
Table III. .
Participants by stakeholder involvement.
| Stakeholder representation | Number* |
|---|---|
| Persons with SCI | 14 |
| Traumatic SCI-motor vehicle related | 4 |
| Traumatic SCI-non motor vehicle related | 7 |
| Non-traumatic SCI | 3 |
| Care providers | 10 |
| Formal (physiatrist, GP/FP, PT, case managers) | 9 |
| Informal | 1 |
| Community advocacy organization representatives | 6 |
| Regional services coordinators | 2 |
| Senior administrators | 4 |
| System service delivery administrators | 2 |
| Public senior administrator and policy maker | 1 |
| Private senior administrator | 1 |
*Numbers do not add to 28 because many participants represented multiple roles.
GP/FP: General practitioner/family practitioner, PT: Physical therapist, SCI: Spinal cord injury
Journey of care: a fight across the continuum
A major over-arching domain that emerged from the data was the concept of “fighting” for all key stakeholder groups (e.g. between individuals with a SCI and the care providers;between individuals with a SCI and the health system, among care providers, and between care providers and the health system). Given this, the results will be structured within the context of the ‘fighting’ and themes stratified by micro (individual-level), meso (care provider level) and macro (health system level). In efforts to maintain participant anonymity, only phase I or II, gender, and the broad stakeholder category will be included with each quote. Overall, eleven themes were identified and represented in Figure 2.
Figure 2. .
Thematic results in conceptualization of the journey of care related to secondary health conditions.
Micro level: individual experiences
Three major themes emerged from the data that represented individual struggles/battles experienced by participants related to SHCs: (i) social isolation and system abandonment, (ii) funding and equitable care, and (iii) bounded freedom for self-management.
Social isolation and system abandonment
Participants in both phases described several challenges in transitioning from inpatient rehabilitation to the community in dealing with SHCs. In particular, participants highlighted the issues with social isolation and spoke about a perception of system abandonment. Several examples were described of individuals being discharged home prior to any home and/or vehicle modifications occurring, which posed increased risk for adverse events and SHCs.
“An individual that I was working with was really isolated. He was discharged to his home. The second story of his home was where the only bathroom was. So basically he was stuck on the second floor of his home with no way of getting down those stairs... I was very concerned about his safety and the very fact that if there was an emergency he would be at the mercy of the fire department to get him out. Anyway, because he was like in bed most of the time it took a couple of months for a physiotherapist. He was not in a position to be able to attend any kind of outreach, physical therapy opportunities. So yeah, it took like some time and he had a huge problem with edema.” (phase II; female community advocacy representative; informal care provider)
Participants in both phases spoke of the social isolation due to limited resources in more rural communities such as those in Northern Ontario. Recreational activities and community participation were noted as being important aspects of overall health and minimizing SHCs.
“…the lack of so many things that we all consider vital to our overall health and wellbeing, that the access and availability to it is so limited. I guess it’s again the social isolation that people face.” (phase II; female community advocacy representative)
In addition to rural areas, participants noted similar challenges with limited resources in suburban areas. Participants highlighted that unless they lived in an urban center with access to a specialized rehabilitation center for SCI, they were more likely to feel lost and disconnected.
The vulnerability of persons with SCI was evident and participants stressed the importance of feeling supported by their health care providers in dealing with SHCs. Participants in both phases spoke about the need to be easily connected with health care providers, especially given the acuity and sensitivity of some SHCs that can transition rapidly from a non-emergent scenario to an emergent situation. In particular, participants with SCI spoke about using the emergency departments as means to access primary care services due to various challenges in accessing a general practitioner.
“I did have one situation where I had a physician dump me as a patient and it was at a critical time from a mental health perspective…That can be much more devastating for somebody who has a spinal cord injury and finds himself in a position where they don’t have a family physician, especially if you’re in kind of a crisis situation…” (phase I; male with a SCI)
There was an added sense of social isolation if persons with SCI were not of the ‘typical’ SCI, such as those with non-traumatic SCI. Participants spoke about research and supportive literature for SHCs being biased towards traumatic SCI with limited resources for persons who might not fit the stereotypical pattern of a SCI. For example, participants spoke about the common perception that SCI is only traumatic and typically affects young males. This stereotyping can promote persons who might not fit in this stereotype to feel isolated in dealing with their SCI and associated SHCs.
“…the other gap I think is the non trauma… Trauma comes through a certain trajectory. You end up in an emergency, trauma send you up to acute care and you by and large end up in rehab… If you come out from oncology, you don’t and you are lost in the system… If you … didn’t graduate from Toronto Rehab, you cannot get in without a GP (general practitioner) referral and it depends when you have a GP and if you have a GP that has the time, energy and effort to sort of manage that piece for you…” (phase II; male senior system administrator)
On the other hand, the importance of community advocacy groups, like the CPA, was identified in minimizing social isolation, as these organizations helped link individuals to services within the community.
“…rehab is non-existent up here… There’s no follow up… CPA [Canadian Paraplegic Association], if it hadn’t been for the regional coordinator, I would have been left slapping in the wind.” (phase I; female with a SCI)
Fight for funding and equitable care
Participants in both phases highlighted the inequities based on funding and insurance coverage. Inequities were suggested to be critical factors related to the prevention and/or management of SHCs. Particular differences were noted in community rehabilitation between those individuals with private insurance versus individuals solely relying on publically funded rehabilitation such as home care services. Individuals with private insurance were able to receive private rehabilitation such as physical therapy, occupational therapy, massage therapy, while those individuals relying on home care services were not having needs addressed that would minimize the occurrence and progression of SHCs.
“…when I didn’t have insurance, there was like oh it’s ADP [Assistive Devices Program] so they’re going to get the bare minimum, so let’s get them in a chair. My chair was totally wrong for me when I got home, totally wrong… when I went to CPA, the regional coordinator kept looking at me and my chair going ‘you’re not sitting very well.’ She had somebody come and check it... I was practically laying down in my chair and she had it adjusted so that I could at least function until I could get a new chair… I remember the girl that was in the room with me, she had insurance and I didn’t and like she had tried out like 4 or 5 different chairs. I got like 2 to try and then they were pressuring me to order. The only reason I got 2 to try was because I didn’t like the first one. So like a really big difference and a lot of people will tell you that too. The care is totally different… If you don’t advocate for yourself, then you’re totally lost.” (phase I; female with a SCI)
Participants in both phases highlighted the battles for individuals who did not have private insurance with respect to accessing proper technology and assistive devices, home and vehicle modifications, medical expenses for equipment such as catheters. One male participant spoke of the financial ‘sacrifice’ that he and his wife consciously made to use new catheters every time to minimize the occurrence of UTI.
“She was very vulnerable. She was reusing catheters. ADP (Assistive Devices Program) will give you a power chair but they won’t give you a manual backup. So if the power chair breaks, you’re stuck at home or stuck in bed. She will be able to purchase all of those services when she gets her settlement. So she’s going to go back into a house or a condo or something that is accessible. She will get a vehicle. She will be able to be mobile within her community. She will be able to manage her bladder better because she will have more attendant care and she won’t need to be reusing catheters. I mean the whole quality of her life is going to change as soon as this lawsuit is settled.” (phase II; female formal care provider)
The necessity for advocacy was noted whether it be driven by the person with the SCI, care provider, or advocacy group. The time required to negotiate the various processes and policies for funding such as assistive devices was ascribed to be similar to a full-time job. ‘There’s a lot of negotiating, managing, working through, pulling out hair…’ (phase I; male with a SCI)
Bounded freedom: the fight to self-manage
Participants with SCI expressed frustrations at the care provider, as well as the health system level with respect to the concept of self-management. Persons with SCI spoke about having the self-efficacy to self-manage but highlighted that the health care system was paternalistic with barriers imposed on one’s ability to self-manage. For instance, participants spoke of not being able to initiate home care services without a general practitioner/family practitioner’s referral in circumstances when timely access is critical (e.g. wound management).
“The thing is he has to refer everything, so I have to go through my GP. Then it goes to CCAC [Community Care Access Centre/home care service], they have to approve it and they prioritize at CCAC. Then my nurse prioritized me though and then it goes to an agency and then with time restrictions for them, it took... it had been okayed at CCAC in two weeks and then it took another two weeks for the OT to come to me. So it had been sitting at the agency then…I’m top priority and I’ve waited a month… because my cushion needed checking and I was top priority for that and it took them over a month to get to me.” (phase I; female with a SCI)
Some participants noted that their formal health care providers were not paternalistic in their interactions with patients, as there was a trust established with their formal health care providers to initiate needed care; rather, the larger health system is structured in a paternalistic manner with barriers at the system/policy level that prevented initiation of care.
“When I had this gash, I phoned up my family doctor and she’s superb. I’ve had her for 20 years and knows me on a first named basis. I sort of said ‘I’ve got this gash. I need somebody to come in and look at it.’ She sort of said ‘okay, try and do it yourself.’ Initially it was phone CCAC and see if you can do it yourself. Well their policy is you as the patient cannot initiate care unless you want to pay for it. It has to be done through a GP or what not. So it wound up being sort of a laggy process because my doctor doesn’t work 5 days a week, 8 hours a day… we wound up skipping through a weekend before we could get back on the phone to her and say ‘please make the phone calls to initiate this and this’ and it took a day or two to get that set up... I couldn’t get what I knew I needed fast enough… When the family doctor called, the earth moved. So it bothered me a little. Maybe it’s just me because I’m not the kind of person who tends to cry wolf. But you know I clearly knew there was a problem and an issue, let’s just get it solved and let’s just get it solved and do it. I felt constrained by the system I guess.” (phase I; male with a SCI)
Meso level: caregiving tensions
Four major themes emerged from the data at the meso care provider level: (i) gender and informal caregiving strain, (ii) help versus disempowerment, (iii) holistic care and thinking outside the box, and (iv) poor communication and coordination.
Gender and informal caregiving strain
The importance of informal caregiving was articulated by participants and often referred to as a ‘secondary team’ and ‘filling in the gaps’ of the formal health care system. In particular, women seemed to be providing more of the caregiving role, whether as a wife, mother, daughter or female friend.
“Her mother is elderly. When she dies I would imagine that she’ll probably have to be placed. She’ll go into long-term care. She’s very young. I don’t even know at this point if she’s eligible for senior housing and would probably cycle in and out of hospital as she ages and she starts to develop the chronic medical problems that we know that people with spinal cord injuries who have to function solely within the system do sustain.” (phase II; female formal care provider)
Men who experienced an SCI seemed to be coping better in the prevention and management of SHCs as often their wives were performing on-call duties for activities such as bowel and bladder management. In contrast, women who were married or had a common-law relationship did not speak of their male significant others to be assisting with the more intimate personal care.
“Now my wife fortunately works literally 10 minutes down the road from the house, so if all of a sudden I’m going I’ve got to go now, I often can just pick up the phone and say please come home now if you can. And she does…” (phase I; male with a SCI)
Most participants in both phases were aware of how dynamics between family and friends change with informal caregiving.
“…let’s go back to this same individual that spent that first year pretty much isolated in this small second story bedroom, that his wife was feeling overwhelmed because she actually maintained a full time job and she had minimal energy left at the end of the day to actually even clean her own house… the frustration because so many things are out of your control. That’s another part of this, whether it’s anything to do with systems or government or whatnot, is that feeling of being disempowered, when everything is out of your control, when you’re waiting by the phone so to speak for somebody to call and say ‘yes, it’s been approved.’... there’s a lot of caregiver burnout. Because you go to work, you come home and there are other things that need to be done. There’s more laundry, there’s incontinence issues.” (phase II; female community advocacy representative; informal care provider)
In particular, female participants with SCI spoke of being uncomfortable with these new role changes that occur with their informal care providers. There was a sense of frustration that they required help from informal care providers to help with day-to-day activities.
“Even with my family, I relied on them an awful lot but I didn’t want my mom to feel that she got her baby back. You know I was 40 some years old when this happened to me.” (phase I; female with a SCI)
Help versus disempowerment
Participants in both phases, particularly in phase II, spoke of the delicate balance between helping persons with SCI versus ‘over-prescription’ and ‘disempowerment’. This balance was noted to be critical in maximizing independence and fostering a person with SCI’s ability to deal with SHCs. Participants noted that there is a risk of over-prescription, particularly in the event that an individual with SCI has access to private insurance coverage, such as that from a motor vehicle accident.
“So they want to give everybody 24 hours of attendant care. Now if you actually receive 24 hours of attendant care when you don’t need it and you receive homemaking services and childcare services, all of a sudden there’s a question and there would be a question in my mind, is are we almost supporting a disability lifestyle. So there’s also a concern I know on the insurer part that over prescription in fact may promote a sense of greater disability and a sense of needing help and a sense of becoming more and more dependent. Whereas I know in many cases attendant care is critical for toileting and dressing. There’s no question there’s a need for attendant care. But again, there’s a concern that it’s being over prescribed.”(phase I; female with a SCI)
Holistic care and thinking outside the box
The findings highlighted perceptions of a struggle for validation and the necessity to continue ‘fighting’ to have concerns heard by health care providers. Moreover, participants in both phases spoke of frustrations experienced with health care professionals primarily stemmed from the treatment of a SHC in a manner that fails to consider the ‘whole person’ or context. Participants noted that treating a SHC with a silo narrow-minded lens led to a myriad of potential adverse risks.
“I think that doctors need to take a look at the whole person and how everything kind of fits together and how something like bladder and bowel problems can affect things like skin breakdown. They wanted to try different oral diabetic medications with me but most of them have diarrhea as a side effect. With a neurogenic bowel, that’s not the right way to go. But they don’t see that. They just see how these medications can help with the one disease or ailment that they are treating. They don’t see it as oh well, if it’s a neurogenic bowel, that means prone to diarrhea anyway, so you add a medication with the diarrhea as a side effect, that can lead to skin breakdowns, bladder infections, pressure sores. They don’t see it that way.” (phase I; female with a SCI)
Poor communication and care coordination
Participants in both phases spoke about challenges with communication between persons who have a SCI, informal care providers and formal health care providers. Participants in phase II particularly noted that having access to a case coordinator made a significant difference in facilitating communication and care coordination. For example, several participants described how a private case coordinator is able to facilitate virtual rounds for all the formal health care professionals, informal care providers and the person with the SCI to discuss care management and SHCs.
“This is really kind of frustrating because when people don’t even know what they actually could be rightfully entitled to or what they could actually achieve... it’s so fortunate for the people that actually do have some kind of insurance coverage that at least quite often they will end up with a case manager or a lawyer or somebody that’s actually on their team. …it’s a fight for everything... unless they have an unusual opportunity to have an ally or for example a wife or a parent or somebody that is just a go getter… But not everybody has that support… It’s a lot of connecting of the dots. When a person is depressed or having a bad pain day or whatever reason, that’s when they’re most vulnerable and that’s when they’re least capable of doing all this work, all this coordination. They don’t have the energy.” (phase II; female community advocacy representative; informal care provider)
Despite the increased role of informal care providers and community advocates such as regional service coordinators with the CPA, many participants perceived a lack of respect for these individuals on the part of formal care providers and a failure to recognize them as an integral part of the team.
Macro level: health system influences on the journey of care
At the health system level, four major themes emerged from the data: (i) fight for access and availability, (ii) models of care tensions, (iii) private versus public tensions, and (iv) rigidity and inflexibility of policies.
Fight for access and availability
Participants in both phase I and phase II spoke about having to fight for access to services, particularly access to specialists (especially urologists) and rehabilitation professionals. In particular, participants noted significant wait-times for care, which was suggested to have exponential consequences for SHCs. As an example, several participants noted the lengthy wait-times for occupational therapy seating assessments. During this wait-time, participants spoke of pressure sores developing and causing a series of negative consequences including re-admission to the acute care. Re-admissions to acute care were required for several participants due to further wait-times to obtain access to community wound care management.
“…it’s just so promising to see all the research…And then when I think of coming back to [small town] and my community and what little there is for us and how long it takes individuals to actually get a referral to a urologist. I can give you an example of an individual that waited almost a year to see a urologist to get the results of urodynamics testing and then after all was said and done now he’s waiting another almost nine months for a referral to a urologist in the Toronto area. In the meantime he’s living life with ongoing incontinence issues and it’s really impacted the quality of life… It has far reaching systemic impact.” (phase II; female community advocacy representative; informal care provider)
In both phases, participants spoke of the challenges in physically accessing different health services in the community that are not in close proximity. Participant identified a need to have a ‘one stop shop’ where all services would be in the same facility (diagnostic testing, screening services, specialists, general practitioners, rehabilitation professionals).
“… most of the people that I speak to with spinal cord injuries can’t get to their GPs because it’s not accessible. They can’t get on the examining bed.” (phase II; female formal care provider)
Models of care tensions
Models of care tensions were identified in four main areas: (i) bio-medical versus social determinants; (ii) prevention versus acute care; (iii) GPs versus specialists; and (iv) informal versus formal care provision. Participants noted that health is beyond the traditional bio-medical model and includes social determinants of health and preventative care. Participants spoke of frustrations with the narrow scope of publicly funded health care and noted that it is important to address the long-term well-being of a person in thinking about SHCs.
“Welfare and social assistance and all that needs to be considered because you’re looking at the person from a holistic point of view. You have to look at where they are in their life cycle and what are their needs and it’s not just healthcare. Other things contribute to probably their health deterioration… It’s health in its broadest sense, broadest term. So health and well-being fundamentally.” (phase II; female senior system administrator)
Models of care were seen to take a reactive approach that focuses on acute care following worsening of symptoms rather than a pro-active approach that focuses on prevention. The health system was consequently described as ‘putting out fires’ (phase II; female community advocacy representative; informal care provider) rather than working on preventing SHCs.
“We don’t move money to the areas of high need. We react to the political pressures. Nor do we have a long run view. We have a short view… So what gets us through tomorrow or gets them out today, not what’s the best thing ultimately. You have to invest in that and I think prevention is a classic one. No one argues prevention. No one just wants to invest in it because it’s an opportunity cost against something today.” (phase II; male senior system administrator)
Participants in both phases also spoke of caregiving tensions surrounding the question of who should provide care to persons with SCI, in addition to the pros and cons of adopting different models of care in the process (specialist versus general practitioner, formal versus informal). The interviews reflected a lack of consensus among participants regarding who is best able to provide care. Several participants spoke about the responsibility of the formal system, particularly using general practitioners/family practitioners as the main source of care provision. Other participants suggested that SCI requires specialized knowledge, resources and time to which general practitioners/family practitioners do not have easy access. Given the specialized care that is often required when treating SCI, several participants highlighted the need for general practitioners to be supported by experts such as physiatrists.
“Most specifically with the healthcare is a lack of I guess awareness or lack of specialization on the parts of our local physicians about spinal cord injury and those secondary complications. Most physicians don’t have very much, if any, experience working with someone with a spinal cord injury. So I don’t think they understand those complications at all. As a result, they’re not able to effectively deal with those secondary complications or make appropriate referrals.” (phase II; female community advocacy representative)
There were also tensions regarding the increasing emphasis on informal care provision and decreasing responsibility of the formal providers. Several participants highlighted concerns with this growing shift in care delivery.
“Caregivers… they’re doing all the work. They’re doing themselves a service and a disservice. They’re servicing, they’re looking after a loved one. The problem is they’re masking the system’s inability to look after, so that they’re actually solving the problem so it isn’t a problem. They’re stretched to the limit to do that. As long as they can manage that piece one more time, then the system doesn’t… need to look after that individual because mom and dad are. In fact mom and dad are getting older, that the individual has no place to go when they pass on. That they can’t be caregivers to their parents is we don’t want to talk about that...” (phase II; male senior system administrator)
Participants in phase II noted that a case management model is useful in assisting individuals within the community deal with SHCs, and how case managers can appreciate the influence of the context in which an individual lives; however, differences were noted between private case management versus the publically funded model with home care services (to be discussed in more detail below).
Public versus private tension
In both phases, significant tensions were noted in the discussion related to publically versus privately funded care. Private insurance coverage, particularly within motor vehicle accidents, can provide individuals with significant financial protection compared to that of the publically funded health care. Several participants in both phases noted that this access to funds could lead to inappropriate and inefficient use of services within the health care community and professionals with over-prescription. This notion of over-prescription in the privately funded community is a contrast to the significant struggles participants highlighted for basic services and equipment that are sought through publically funded channels throughout the journey of care. Participants in both phases noted the challenges of working within a multi-tiered healthcare system, particularly with community rehabilitation, which represents an important component for individuals with SCI.
“Well I think that there’s a general perception that Canada has a single tiered healthcare system and that’s simply not true and it’s unfortunate that people think that. I think it’s not so much the insurance sector. I think it’s the auto insurance sector where there are rich benefits for people who have spinal cord injury. So if you compare funds available to someone who sustains a spinal cord injury in a car crash versus someone who sustains spinal cord injury by a fall in their backyard, there’s a huge discrepancy… I think that because there are such rich accident benefits that are quite easy to access... they’re all fighting over a piece of the pie and nobody has to cure our patients. So they treat and treat and treat. I think there are a lot of good providers. I think there’s probably 25% or 50% of the system are really good people trying to do the right thing but the rest of the system is just trying to juice it. Of course the good providers get trapped in that whole game. Insurers become cynical and distrustful and they distrust the good provider just as they distrust the bad provider. Then there’s this misunderstanding and again, frustration, on all parts.” (phase II; female formal care provider)
Rigidity and inflexibility of policies
Participants in both phases noted frustrations with policies pertaining to initiation of health services particularly related to home care services. Previous frustrations are described in the ‘bounded freedom’ theme with respect to policies requiring a physician’s referral to initiate services such as wound care or rehabilitation. In addition, participants noted frustrations with the rules established for determining rehabilitation eligibility. Participants with SCI commented on how being refused for rehabilitation led to increased risks for developing and/or worsening SHCs. These rules for rehabilitation eligibility were perceived by participants to highlight the ‘reactive’ nature of health care rather than a focus on “prevention” and ‘maintenance of well-being’.
Participants in phase II also noted significant challenges with how family physicians and general practitioners are financially compensated. Most of these physicians are compensated by fee for service rather than salary-based compensation. As such, certain services that are not financially compensated (e.g. renewing prescriptions over the phone) require physicians to perform the service free-of-charge or individuals to physically visit the clinic.
“So how perverse is that? So that if I’m a family doctor, why would I take an hour for an individual when I’m compensated for 10 minutes?... Forget altruism. I mean it’s just unfair to make people do that. With that incentive system, take a whole bunch of people that don’t need healthcare or are they already well. So again, our models aren’t sweet enough to differentiate. It’s a one size fits all… I think that’s frustrating for individual families because they come out of it from that level. It’s about them. I mean it’s not about the policy. They’re saying I need these kinds of things to improve my quality and manage myself... So we over service some things and we under service other things.” (phase II; male senior system administrator)
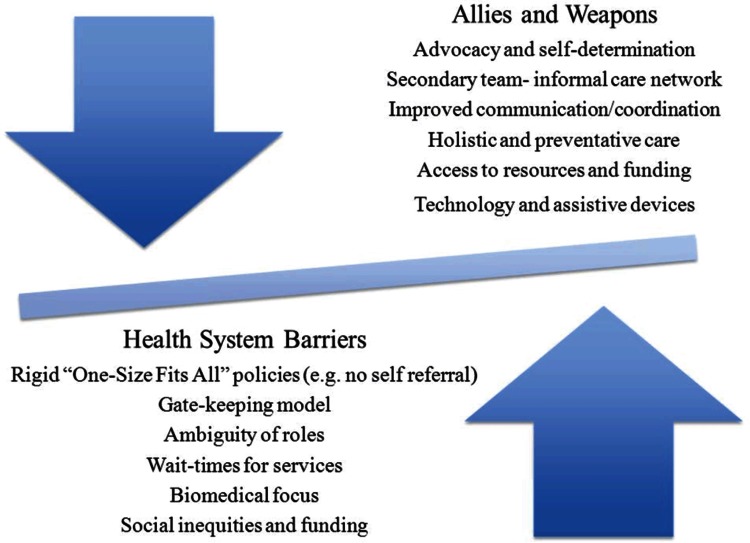
Discussion
Using Pescolido’s NEM, we identified several key themes related to the journey of care for preventing and managing SHCs for persons with SCI living in Ontario. Specifically, we identified significant tensions and struggles that exist for persons with SCI, care providers, administrators and policy-makers. While these tensions were evident across the micro, meso and macro levels, these findings suggest that the structural and policy-related barriers within the macro health system are major obstacles in the care pathway (see Figure 3).
Figure 3. .
The uphill journey in the prevention and management of secondary health conditions.
Taken together, the findings point to a general uphill journey for persons with SCI and for those who assist with care provision in the community. The individual struggles at the micro level were also highlighted, particularly with respect to perceived abandonment by the health system due to shortcomings with the provision of support and services, as well as various restrictions resulting from health care policies that are perceived to be strongly paternalistic in nature [45].
These micro level battles seemed to be influenced by overall macro health system structures and rigid policies. Particular structural obstacles were identified that rendered pathways of care more arduous such as distribution of and access to services. Participants identified frustrations rising out of an inability to initiate care with the current gate-keeping referral model. These tensions reflect Lawn’s concept of ‘responsiblizing’ without power sharing (p.e7) and contributes to overall frustrating experiences with the health care system in dealing with SHCs, especially given most of the intervention efforts to date have been targeted to patient knowledge and self-management behaviors [9].
Further, given the current gate-keeping model of primary care and the vulnerability of persons with SCI developing SHCs, it is critical for persons with SCI to feel validated and concerns heard [46]. The present study builds on previous work highlighting caregiving tensions between persons with SCI and care providers. Lack of formal care providers’ knowledge and negative attitudes [22,23,46] seem to promote frustrating health care experiences for persons with SCI, and their informal care providers.
Additionally, participants noted rigid rules and policies within home care services that rendered significant difficulty in accessing ‘maintenance rehabilitation’. Unless persons with SCI have access to private insurance and/or personal funds, community-based rehabilitation is limited in Ontario [47]. Maintenance rehabilitation can serve an important role in preventing and/or slowing down the potential decline in functional ability; however emphasis is not placed on rehabilitation but rather acute medical needs [9]. This is particularly important given the decreased length of stay in acute and rehabilitation facilities and earlier discharges to the community [9]. It is beyond the scope of this paper to engage in a philosophical debate regarding what constitutes ‘rehabilitation’ but results of this study suggest that this discourse on rehabilitation and how we operationalize and implement the concept of rehabilitation warrants further attention.
The fight to access maintenance rehabilitation under the publicly funded health system highlights a significant weakness in it’s focus on acute bio-medical management rather than embracing a more individualized prevention chronic care and living well model. The lack of rehabilitation services available within the publicly funded system once persons are discharged to the community was highlighted as a key barrier in preventing and managing SHCs.
The present research identified caregiving tensions with respect to who should be assisting with care and, in particular, the ambiguity of roles for informal care providers. We have transitioned responsibility to informal care providers without perhaps proper reflection of the ethics associated with this change of care delivery [11,48]. Informal care providers and individuals associated with advocacy groups provide numerous roles as ‘secondary team members’ for persons with SCI (see paper 2). These secondary team members serve as critical allies in creating a more positive journey. However, as participants highlighted in the present research, at what point does the scale of informal-formal care provision become unbalanced? At what point is it no longer acceptable for informal care providers and community advocacy organizations to cover the fragmented holes in the formal health care system? As DeJong states ‘use of peer mentors, patient navigators, patient advocates, and other forms of patient coaching underscores many of the health system’s underlying weaknesses with respect to access, usability, and responsiveness’ (p. 50) [9].
This study stresses the importance of timely access to comprehensive primary health care. For certain conditions, such as pressure sores, persons with SCI need to have timely and efficient access to services from preventative services such as cushion assessments to wound management. In the present research, there were several examples of how long wait-times ranging from occupational therapy assessment to community-based nursing care contributed to individuals with SCI being re-admitted to acute care facilities for wound management. While home care services in Ontario currently have a priority list, this research suggests that persons with SCI are not getting appropriate treatment in a timely manner that prevents the negative sequence of adverse events for highly sensitive conditions. Due to rigid policies, participants with SCI in this study spoke of long wait-times to see their GPs to initiate a home care service referral and then another delay in receiving home care services. The costs to the person as well as the health system are significant for pressure sore management. For example, the annual costs to home care services in Ontario (Community Care Access Centres [CCACs]) for wound care management of approximately 30,000 persons is $240 million (CND) [49]. Specific to SCI, persons with pressure ulcer history have significant decrease in life expectancy [50] and the cost to the system is estimated to be over $100,000 USD per pressure ulcer case in the acute care setting [51]. A better triage priority system needs to be implemented across the continuum of care for persons with SCI in the community for these highly sensitive medical conditions.
Previous efforts to minimize SHCs have largely focused on the person with SCI and at the provider level [9]. Results from this research suggest that in order to effectively reduce SHCs, we need to start thinking bigger and more holistically in addressing triggers of SHCs rather than fragmented efforts to ‘put out the fires’. DeJong recently noted three key solutions to improving health care for person with SCI in the community: (i) patient education and health behavior change, (ii) better transitions from inpatient rehabilitation to community care, (iii) new systems of health care delivery. Most efforts have previously focused the first solution [9] and the present findings suggest that individuals with SCI are knowledgeable about their injury and SHCs; however, there seemed to be a need for improved knowledge dissemination as to how to navigate through the fragmented health care system. Documents reviewed for this study supported the notion that information on funding sources for durable medical equipment and assistive devices are not easily accessible to individuals. Informal care providers and community advocacy organizations (regional service coordinators within the CPA for example) were assisting as knowledge brokers to address this challenge with knowledge transfer.
Our research findings support DeJong’s second suggestion to improve transition to the community but especially to provide innovative new systems for health care delivery [9]. The first and second solutions assume that that the community-based health system environment is agreeable to foster optimal care; however, the struggles identified in the present study suggest that we need to re-think the payment systems, delivery of services, and models of care.
Our current publicly funded health care system in Ontario, as exemplified by these findings, is a broken system for persons with SCI. Ontario policy-makers need to start innovatively thinking of strategies to minimize these barriers for persons with SCI living in the community. For example, perhaps there needs to be accountability and accreditation across the continuum of care [52,53]. It is not acceptable for health care institutions or as Michael Porter calls ‘focused factories’ to be working in silos with minimal feedback for care provision [52]. We need to start thinking innovatively as to how best to provide timely, efficient, effective, comprehensive individualized care for persons with SCI and on a larger scale, for persons with any complex chronic condition.
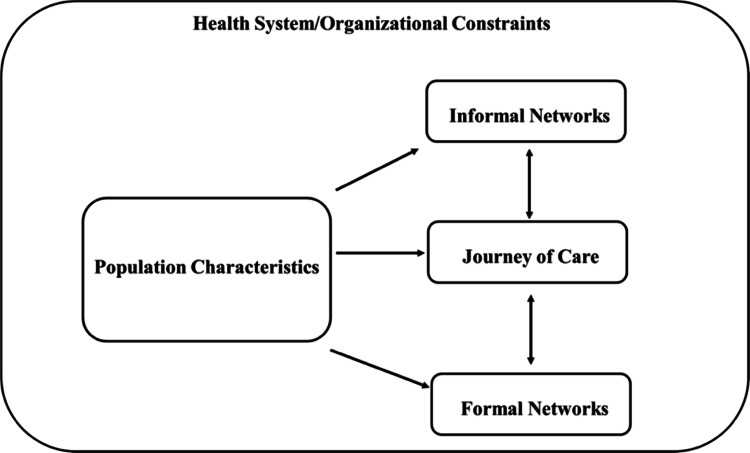
It is our understanding, that to date, the NEM has not been applied beyond mental health and the present research has highlighted it is a useful model for other complex conditions, such as SCI. This model was useful in guiding the research inquiry, as it helped with the conceptualization of key areas related to the journey of care (e.g. network characteristics and environmental components). Based on the present research findings, a few modifications to the NEM are recommended in its application to understanding the journey of care related to SHCs for persons with SCI. A key modification would be to recognize the magnitude of the health system and environmental influence on the overall journey, networks of care as well as the individual experience. Thus, the proposed change would be to place the other domains within the macro health system (see Figure 4), as this acknowledges the critical influence the health system environment has on the other domains.
Figure 4. .
Revised Network Episode Model based on research findings.
Limitations of research
There are several limitations to this work that should be noted. Firstly, this research reflects the micro, meso and macro levels of Ontario as this province was selected for the case of inquiry. Given that health care services are provincially operated in Canada, these research findings may not be generalizable to these different contexts. Future research, such as a multiple case study, would be warranted in the examination of the journeys of care with other provinces. Comparisons of these case findings would be beneficial, especially in the context of different health system structures. As with all convenience sampling approaches, there is a potential for responder bias. However, considerable efforts were made to use purposeful sampling such that there was a broad representation across persons with SCI as well as the other stakeholder groups.
Implications for future research
This study highlighted several important themes, particularly with respect to health system and environmental factors that relate to the journey of care for SHCs. In using case study methodology and the NEM as a conceptual guide, findings from this study suggest the need for future research to investigate the associations between themes identified and health outcomes. Further, future research is warranted in examining more specifically how Porter’s outcome measures hierarchy framework fits within the context of SCI and SHCs.
Conclusions
This study focused on an in depth examination of the journey of care related to SHCs for persons with SCI living in Ontario. Findings from this case study suggest that the journey is challenging and an uphill struggle for persons with SCI, care providers, and community-based advocates. Results suggest that if we are to make significant gains in minimizing the incidence and severity of SHCs and improve the overall value of health care, we need to tailor innovative interventions at the health system level, rather than our current trend of fragmented interventions at the individual or health provider level.
Acknowledgements
The authors also acknowledge the support of the Toronto Rehabilitation Institute (TRI), which receives funding under the Provincial Rehabilitation Research Program from the Ministry of Health and Long-Term Care (MOHLTC) in Ontario. The views expressed do not necessarily reflect those of the Ministry. Ms. Guilcher’s doctoral training has been supported throughout the years by the Canadian Institute for Health Research, Women’s College Research Institute, Ontario Neurotrauma Foundation, TRI, Community University Research Alliance, and Ontario Training Collaborative Program in Health Services and Policy Research. Dr. Jaglal is the TRI Chair at the University of Toronto in Health Services Research.
Declaration of Interest: The authors declare no conflict of interest.
Appendix A: Example list of documents collected and reviewed
Documents
Canadian Paraplegic Association Websites
2010 Federal Disability Report
Community Care Access Center Website
Home and Vehicle Modification Program Guidelines
Ontario Travel Grants
Assistive Devices Program
Ontario Community Support Association
Centre for Independent Living Toronto
Financial Services Commission of Ontario: Auto Insurance
Slide decks from National Case Management Network
Codes of Ethics and Standards of Practice for Case Management
References
- 1.Strauss DJ, Devivo MJ, Paculdo DR, Shavelle RM. Trends in life expectancy after spinal cord injury. Arch Phys Med Rehabil. 2006;87:1079–1085. doi: 10.1016/j.apmr.2006.04.022. [DOI] [PubMed] [Google Scholar]
- 2.Paker N, Soy D, Kesiktas N, Nur Bardak A, Erbil M, Ersoy S, Ylmaz H. Reasons for rehospitalization in patients with spinal cord injury: 5 years’ experience. Int J Rehabil Res. 2006;29:71–76. doi: 10.1097/01.mrr.0000185953.87304.2a. [DOI] [PubMed] [Google Scholar]
- 3.Savic G, Short DJ, Weitzenkamp D, Charlifue S, Gardner BP. Hospital readmissions in people with chronic spinal cord injury. Spinal Cord. 2000;38:371–377. doi: 10.1038/sj.sc.3101019. [DOI] [PubMed] [Google Scholar]
- 4.Anson CA, Shepherd C. Incidence of secondary complications in spinal cord injury. Int J Rehabil Res. 1996;19:55–66. doi: 10.1097/00004356-199603000-00006. [DOI] [PubMed] [Google Scholar]
- 5.Noreau L, Proulx P, Gagnon L, Drolet M, Laramée MT. Secondary impairments after spinal cord injury: a population-based study. Am J Phys Med Rehabil. 2000;79:526–535. doi: 10.1097/00002060-200011000-00009. [DOI] [PubMed] [Google Scholar]
- 6.Hitzig SL, Tonack M, Campbell KA, McGillivray CF, Boschen KA, Richards K, Craven BC. Secondary health complications in an aging Canadian spinal cord injury sample. Am J Phys Med Rehabil. 2008;87:545–555. doi: 10.1097/PHM.0b013e31817c16d6. [DOI] [PubMed] [Google Scholar]
- 7.Dryden DM, Saunders LD, Rowe BH, May LA, Yiannakoulias N, Svenson LW, Schopflocher DP, Voaklander DC. Utilization of health services following spinal cord injury: a 6-year follow-up study. Spinal Cord. 2004;42:513–525. doi: 10.1038/sj.sc.3101629. [DOI] [PubMed] [Google Scholar]
- 8.Chiodo AE, Scelza WM, Kirshblum SC, Wuermser LA, Ho CH, Priebe MM. Spinal cord injury medicine. 5. Long-term medical issues and health maintenance. Arch Phys Med Rehabil. 2007;88:S76–S83. doi: 10.1016/j.apmr.2006.12.015. [DOI] [PubMed] [Google Scholar]
- 9.DeJong G, Hoffman J, Meade M, Bombardier C, Deutsch A, Nemunaitis G, Roach M, et al. Postrehabilitative Health Care for Individuals with SCI: Extending Health Care into the Community. Top Spinal Cord Inj Rehabil. 2011;17((2)):46–58. [Google Scholar]
- 10.Cox RJ, Amsters DI, Pershouse KJ. The need for a multidisciplinary outreach service for people with spinal cord injury living in the community. Clin Rehabil. 2001;15:600–606. doi: 10.1191/0269215501cr453oa. [DOI] [PubMed] [Google Scholar]
- 11.Grant K, Amaratunga C, Armstrong P, Boscoe M, Pederson A, Willson K. Aurora, Ontario: Garamond Press, Ltd.; 2004. Caring for/caring about women, home care, and unpaid caregiving. 23 pp. [Google Scholar]
- 12.Kemp L. Why are some people’s needs unmet? Disabil Soc. 2002;17(2):205–218. [Google Scholar]
- 13.Munce SE, Guilcher SJ, Couris CM, Fung K, Craven BC, Verrier M, Jaglal SB. Physician utilization among adults with traumatic spinal cord injury in Ontario: a population-based study. Spinal Cord. 2009;47:470–476. doi: 10.1038/sc.2008.173. [DOI] [PubMed] [Google Scholar]
- 14.Jaglal SB, Munce SE, Guilcher SJ, Couris CM, Fung K, Craven BC, Verrier M. Health system factors associated with rehospitalizations after traumatic spinal cord injury: a population-based study. Spinal Cord. 2009;47:604–609. doi: 10.1038/sc.2009.9. [DOI] [PubMed] [Google Scholar]
- 15.Guilcher SJ, Munce SE, Couris CM, Fung K, Craven BC, Verrier M, Jaglal SB. Health care utilization in non-traumatic and traumatic spinal cord injury: a population-based study. Spinal Cord. 2010;48:45–50. doi: 10.1038/sc.2009.78. [DOI] [PubMed] [Google Scholar]
- 16.Gontkovsky ST, Russum P, Stokic DS. Perceived information needs of community-dwelling persons with chronic spinal cord injury: findings of a survey and impact of race. Disabil Rehabil. 2007;29:1305–1312. doi: 10.1080/09638280600964364. [DOI] [PubMed] [Google Scholar]
- 17.Donnelly C, McColl MA, Charlifue S, Glass C, O’Brien P, Savic G, Smith K. Utilization, access and satisfaction with primary care among people with spinal cord injuries: a comparison of three countries. Spinal Cord. 2007;45:25–36. doi: 10.1038/sj.sc.3101933. [DOI] [PubMed] [Google Scholar]
- 18.Oshima S, Kirschner KL, Heinemann A, Semik P. Assessing the knowledge of future internists and gynecologists in caring for a woman with tetraplegia. Arch Phys Med Rehabil. 1998;79:1270–1276. doi: 10.1016/s0003-9993(98)90274-x. [DOI] [PubMed] [Google Scholar]
- 19.van Loo MA, Post MW, Bloemen JH, van Asbeck FW. Care needs of persons with long-term spinal cord injury living at home in the Netherlands. Spinal Cord. 2010;48:423–428. doi: 10.1038/sc.2009.142. [DOI] [PubMed] [Google Scholar]
- 20.Manns PJ, May LA. Perceptions of issues associated with the maintenance and improvement of long-term health in people with SCI. Spinal Cord. 2007;45:411–419. doi: 10.1038/sj.sc.3101973. [DOI] [PubMed] [Google Scholar]
- 20.McColl MA, Aiken A, McColl A, Smith K. Primary Care for People with SCI. In: Eng JJ, Teasell RW, Miller WC, Wolfe DL, Townson AF, Hsieh JTC, Connolly SJ, Noonan V, Mehta S, Sakakibara BM, Boily K, . Spinal Cord Injury Rehabilitation Evidence. Volume 4.0. Vancouver; 2012. In. editors. pp 1–28. Available at. Accessed on 8 September 2012. [Google Scholar]
- 22.McColl M, Shortt S. Another way to look at high service utilization: the contribution of disability. J Health Serv Res Policy. 2006;11:74–80. doi: 10.1258/135581906776318848. [DOI] [PubMed] [Google Scholar]
- 23.McColl MA, Forster D, Shortt SE, Hunter D, Dorland J, Godwin M, Rosser W. Physician experiences providing primary care to people with disabilities. Healthc Policy. 2008;4:e129–e147. [PMC free article] [PubMed] [Google Scholar]
- 24.Kroll T, Jones GC, Kehn M, Neri MT. Barriers and strategies affecting the utilisation of primary preventive services for people with physical disabilities: a qualitative inquiry. Health Soc Care Community. 2006;14:284–293. doi: 10.1111/j.1365-2524.2006.00613.x. [DOI] [PubMed] [Google Scholar]
- 25.Hammell KR. Spinal cord injury rehabilitation research: patient priorities, current deficiencies and potential directions. Disabil Rehabil. 2010;32:1209–1218. doi: 10.3109/09638280903420325. [DOI] [PubMed] [Google Scholar]
- 26.Guilcher SJ, Craven BC, McColl MA, Lemieux-Charles L, Casciaro T, Jaglal SB. Application of the Andersen’s health care utilization framework to secondary complications of spinal cord injury: a scoping review. Disabil Rehabil. 2012;34:531–541. doi: 10.3109/09638288.2011.608150. [DOI] [PubMed] [Google Scholar]
- 27.Godleski M, Jha A, Coll J. Exploring access to and satisfaction with health services. Top Spinal Cord Inj Rehabil. 2007;12(3):56–65. [Google Scholar]
- 28.Bussing R, Zima BT, Gary FA, Mason DM, Leon CE, Sinha K, Garvan CW. Social networks, caregiver strain, and utilization of mental health services among elementary school students at high risk for ADHD. J Am Acad Child Adolesc Psychiatry. 2003;42:842–850. doi: 10.1097/01.CHI.0000046876.27264.BF. [DOI] [PubMed] [Google Scholar]
- 29.Pescosolido BA, Gardner CB, Lubell KM. How people get into mental health services: stories of choice, coercion and “muddling through” from “first-timers”. Soc Sci Med. 1998;46:275–286. doi: 10.1016/s0277-9536(97)00160-3. [DOI] [PubMed] [Google Scholar]
- 30.Pescosolido BA, Wright ER, Alegría M, Vera M. Social networks and patterns of use among the poor with mental health problems in Puerto Rico. Med Care. 1998;36:1057–1072. doi: 10.1097/00005650-199807000-00012. [DOI] [PubMed] [Google Scholar]
- 31.Pescosolido BA, Wright ER. The view from two worlds: The convergence of social network reports between mental health clients and their ties. Soc Sci Med. 2004;58:1795–1806. doi: 10.1016/S0277-9536(03)00398-8. [DOI] [PubMed] [Google Scholar]
- 32.Pescosolido BA. Of pride and prejudice: the role of sociology and social networks in integrating the health sciences. J Health Soc Behav. 2006;47:189–208. doi: 10.1177/002214650604700301. [DOI] [PubMed] [Google Scholar]
- 33.Bonin JP, Fournier L, Blais R. Predictors of mental health service utilization by people using resources for homeless people in Canada. Psychiatr Serv. 2007;58:936–941. doi: 10.1176/ps.2007.58.7.936. [DOI] [PubMed] [Google Scholar]
- 34.Carpentier N, Pomey MP, Contreras R, Olazabal I. Social care interface in early-stage dementia: practitioners’ perspectives on the links between formal and informal networks. J Aging Health. 2008;20:710–738. doi: 10.1177/0898264308321025. [DOI] [PubMed] [Google Scholar]
- 35.Pescosolido BA. Advances in medical sociology. Volume 2. Greenwich, CT, USA: JAI Press; 1991. Illness careers and network ties: a conceptual model of utilization and compliance. pp. 161–184. [Google Scholar]
- 36.DeVivo MJ, Farris V. Causes and costs of unplanned hospitalizations among persons with spinal cord injury. Top Spinal Cord Inj Rehabil. 2011;16(4):53–61. [Google Scholar]
- 37.Walker JA. Caring for patients with a diagnosis of cancer and spinal metastatic disease. Nurs Stand. 2002;16:41–44. doi: 10.7748/ns2002.07.16.42.41.c3224. [DOI] [PubMed] [Google Scholar]
- 38.Yin R. Sage Publications Inc. Thousand Oaks, CA, USA: 2009. Case study research: design and methods. [Google Scholar]
- 39.Statistic Canada. 2011 Census Population. http://www12.statcan.gc.ca/census-recensement/index-eng.cfm. Available at. Accessed on 23 February 2012. [Google Scholar]
- 40.Patton MQ. Thousand Oaks, CA, USA: Sage Publications Inc.; 2001. Qualitative evaluation and research methods. [Google Scholar]
- 41.Lincoln YS, Guba EG. Beverly Hills, CA: Sage Publications Inc.; 1985. Naturalistic Inquiry. [Google Scholar]
- 42.Thorne S, Reimer Kirkham S, O’Flynn-Magee K. The analytic challenge in interpretive description. Int J Qual Methods. 2004;3(1):1–11. [Google Scholar]
- 43.Miles MB, Huberman M. Thousand Oaks, CA, USA: Sage Publications Inc.; 1994. Qualitative data analysis – an expanded sourcebook. [Google Scholar]
- 44.King N. Template analysis. In: Symon C, editor. Qualitative methods and analysis in organisational research: a practical guide. London: Sage; 1998. (ed). [Google Scholar]
- 45.Lawn S, McMillan J, Pulvirenti M. Chronic condition self-management: expectations of responsibility. Patient Educ Couns. 2011;84:e5–e8. doi: 10.1016/j.pec.2010.07.008. [DOI] [PubMed] [Google Scholar]
- 46.Meade M, Carr L, Ellenbogen P, Barrett K. Perceptions of provider education and attitude by individuals with spinal cord injury: implications for health care disparities. Top Spinal Cord Inj Rehabil. 2011;17(2):25–37. [Google Scholar]
- 47.Landry MD, Deber RB, Jaglal S, Laporte A, Holyoke P, Devitt R, Cott C. Assessing the consequences of delisting publicly funded community-based physical therapy on self-reported health in Ontario, Canada: a prospective cohort study. Int J Rehabil Res. 2006;29:303–307. doi: 10.1097/MRR.0b013e328010badc. [DOI] [PubMed] [Google Scholar]
- 48.Olesen VL. Caregiving, ethical and informal: emerging challenges in the sociology of health and illness. J Health Soc Behav. 1989;30:1–10. [PubMed] [Google Scholar]
- 49.Care MoHaL-T. Ontario’s Integrated Client Care Project. 2011. Institute for Clinical Evaluative Sciences. Slide deck. http://www.ices.on.ca/file/ICCP_Overview_Slide_Presentation.pdf. Available at. Accessed on 8 September 2012. [Google Scholar]
- 50.Krause JS, Saunders LL. Health, secondary conditions, and life expectancy after spinal cord injury. Arch Phys Med Rehabil. 2011;92(11):1770–1775. doi: 10.1016/j.apmr.2011.05.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Stroupe KT, Manheim L, Evans CT, Guihan M, Ho C, Li K, Cowper-Ripley D, et al. Cost of treating pressure ulcers for veterans with spinal cord injury. Top Spinal Cord Inj Rehabil. 2011;16(4):62–73. [Google Scholar]
- 52.Porter ME. What is value in health care? N Engl J Med. 2010;363:2477–2481. doi: 10.1056/NEJMp1011024. [DOI] [PubMed] [Google Scholar]
- 53.Porter ME. A strategy for health care reform – toward a value-based system. N Engl J Med. 2009;361:109–112. doi: 10.1056/NEJMp0904131. [DOI] [PubMed] [Google Scholar]