Figure 1.
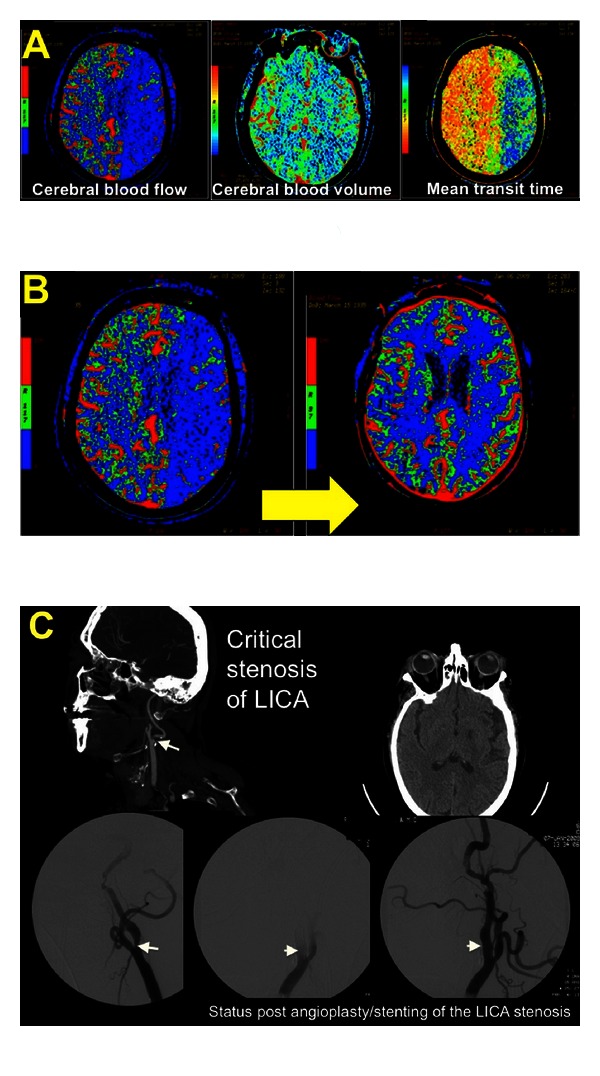
A 73 year-old woman underwent intramedullary fixation of a fractured right femur. She received 2 doses of Hydralazine for elevated BPs the evening after surgery, resulting in a decline in her SBP from 190 mm Hg to 110 mm Hg. The following morning, she was noted to be confused, nonverbal, and paretic in her right arm. An inpatient stroke code was called, and a CT/CTA/CTP was obtained. The perfusion imaging revealed a prolonged MTT, decreased CBF, and relatively preserved CBV within the left hemisphere suggestive of ischemia within this territory (A). She was transferred to the ICU for further management. (B) diagrams the resolution of these perfusion deficits with a marked improvement in CBF following aggressive intravenous fluid resuscitation, blood transfusion for anemia, and BP augmentation with pressors. This was accompanied by a significant clinical improvement as well. Her CTA neck revealed the etiology of her stroke to be a critical stenosis of her left internal carotid artery (C); she underwent angioplasty and stent placement and ultimately had minimal residual symptoms in the form of naming and paraphasic errors. There was no hemorrhagic transformation post-induced hypertension or postprocedurally.
