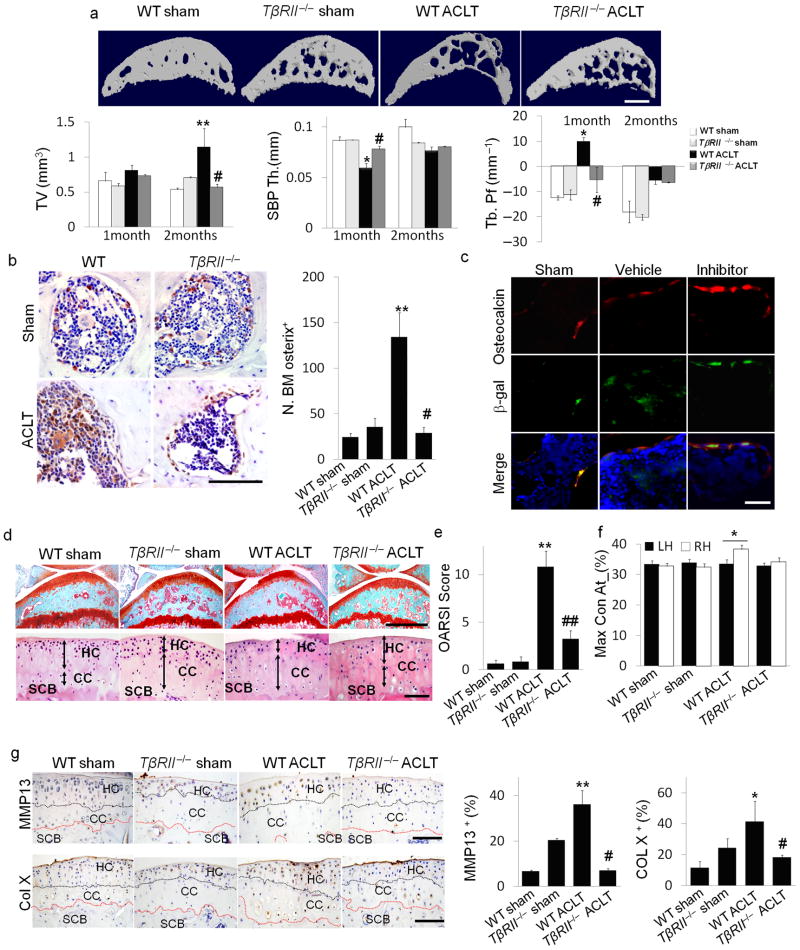
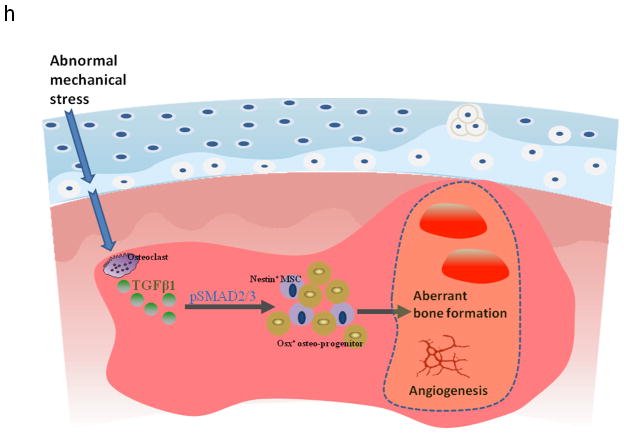
Figure 6. Inducible knockout of TβRII in nestin+ cells reduced the changes in subchondral bone and articular cartilage in ACLT mice.
(a) Three–dimensional μCT images of tibia subchondral bone medial compartment (sagittal view) in wild–type (WT) or Nestin–CreTMER::TβRIIfl/fl (TβRII−/ −) mice 2 months after undergoing sham or ACLT surgery. Scale bar, 500 μm, and quantitative analysis of structural parameters of subchondral bone by μCT analysis: subchondral bone tissue volume (TV), thickness of subchondral bone plate (SBP), and trabecular pattern factor (Tb. Pf). (b) Immunohistochemical and quantitative analysis of osterix (brown). Scale bar, 100 μm. (c) Double–immunofluorescent analysis of osteocalcin (red) and β–gal (green) in subchondral bone of Nestin–CreTMER:: Rosa26–LacZfl/fl mice that underwent sham or ACLT operation and were treated with vehicle– or TβRI inhibitor. Scale bar, 40 μm. (d) Sanfranin O–fast green and H&E staining of the sagittal sections of tibia medial compartment. Scale bar, 100 μm. (e) OARSI scores. (f) Max_contact_at(%) of the gait analysis in mice. (g) Immunohistochemical and quantitative analysis of MMP13 and type X collagen (both stain brown). HC = hylane cartilage; CC = calcified cartilage; SCB = subchondral bone. n = 8; *P < 0.05, **P < 0.01 vs. wild type sham, #P < 0.05, ##P < 0.01 vs. wild type ACLT group. Scale bars, 100 μm. (h) Model of elevated active TGF–β1 in the subchondral bone at the onset of OA. TGF–β1 is activated in the subchondral bone in response to abnormal mechanical loading. The accumulated high concentrations of active TGF–β1 stimulate increases in MSCs and osteoprogenitors in the marrow, which lead to aberrant bone formation and angiogenesis for OA progression.