Abstract
Background
Vitamin B12 deficiency may have deleterious effects on end stage renal disease (ESRD) patients on maintenance hemodialysis, and may increase erythropoietin stimulating agent (ESA) resistance, yet little is known about its prevalence in this population.
Methods
Serum vitamin B12 and methylmalonic acid (MMA) levels were drawn from ESRD patients prior to hemodialysis. All patients with MMA levels greater than 800 nmol/L had peripheral smears evaluated for B12 deficiency. Those with confirmatory smears were considered to be deficient and received intramuscular vitamin B12 injections for 4 months. Post-treatment MMA levels and smears were obtained. Erythropoietin dosages were monitored throughout the treatment period.
Results
There was a 58% (60/103) prevalence of vitamin B12 deficiency as defined by a positive MMA level and a positive blood smear. Out of 52 patients with positive smears, 36 (69.2%) were negative on repeat analysis after B12 treatment. Mean Epogen® (EPO) dosages significantly decreased by 16,572 ± 41,902 units per month from baseline to the post-B12 t reatment period (P = 0.0082, Wilcoxon signed-rank test). Three months prior to treatment, the mean monthly EPO dose was 82,067 ± 47,906 and post, the mean EPO usage was 65,495 ± 39,691. Post treatment hemoglobin levels were not significantly different from baseline.
Conclusion
Vitamin B12 supplementation was associated with a decrease in the mean dose of ESA administration while maintaining a stable hemoglobin level. Maintaining serum vitamin B12 levels improves functionality, and may allow a decrease in the use of ESA’s, avoiding their toxicities and significant costs.
Keywords: ESRD, end stage renal disease, chronic kidney disease, anemia, vitamin deficiency, erythropoietin, dialysis
Introduction
Anemia is a major comorbidity of chronic kidney disease (CKD) and in patients with end stage renal disease (ESRD) on renal replacement therapy. Untreated dialysis patients were often symptomatic and dependent on blood transfusions with their innate morbidity until the advent of erythropoietin stimulating agents (ESA), which transformed anemia management in this population. ESA effectively increase hemoglobin and improve quality of life in patients on dialysis.1 Currently, while effective, the cost burden of ESA is enormous. It is estimated that Medicare costs in the US for ESA are approximately two billion US dollars per year. Additionally, recent reports have shown that ESA are associated with strokes at high hemoglobin levels.2 While ESA address the deficiency in innate erythropoietin production, numerous other factors contribute to anemia as well as resistance to these agents in patients on dialysis. Inflammation, iron deficiency, chronic infections, bone marrow failure, and hyperparathyroidism are among these factors. B12 deficiency is a well described etiology of anemia, classically producing megaloblastic anemia. It is likely due to inhibition of DNA synthesis, thought to be caused by the “methylfolate trap,” or alternatively, the “formate starvation hypothesis”.2 While intuitively, the diagnosis of B12 deficiency should be confirmed by serum B12 levels, this turns out to be neither sensitive nor specific for B12 deficiency. Serum homocysteine levels have superior sensitivity and specifity to serum B12 levels, but elevated methylmalonic acid (MMA) levels have been shown to be the most sensitive and specific marker in the general population.3,4 The diagnosis can be confirmed with a peripheral smear showing hypersegmented neutrophils in addition to macrocytosis.
B12 deficiency has not been well studied in CKD and dialysis patients. Dialysis patients generally have poor nutritional intake,5 predisposing them to B12 deficiency. In addition, foods that are high in B12 typically contain high concentrations of electrolytes harmful to dialysis patients, limiting them to low B12 foods. Furthermore, B12 is a classic middle size molecule, which is cleared well with modern high flux dialyzers, providing an additional reason for hemodialysis (HD) patients to be B12 deficient.
In dialysis patients, B12 deficiency presents a diagnostic challenge. B12 levels, homocysteine, and MMA have not been studied as markers of B12 deficiency in this population. While studies have suggested that serum MMA levels are increased in CKD,6 ESRD and uremia, it is not known whether this is a result of B12 deficiency, or an independent effect of uremia.7,8 Although MMA levels are elevated in patients with renal insufficiency,9 levels are presumed not to exceed 800 nmol/L as a consequence of renal insufficiency.6 Similarly, low serum B12 and high homocysteine levels with a subsequent reversal after B12 therapy have been reported in HD patients, but again, these levels have not been validated as a diagnostic tool in this population. In addition there have been reports of erythropoietin resistance secondary to vitamin B12 deficiency which reversed after supplementation.10,11
In this study, our goals were to determine the incidence of vitamin B12 deficiency in HD patients. In addition we investigated the effect of B12 supplementation on erythropoietin alpha requirements and on quality of life in B12 deficient patients.
Study design
The study was approved by the hospital institutional board review of Staten Island University Hospital, (Staten Island, NY, USA) and all patients provided written informed consent prior to enrolling in the study. In a single center dialysis unit, 132 out of 171 ESRD patients (age 18–80) who were on maintenance hemodialysis for at least 6 months consented and were screened for vitamin B12 deficiency. Three months prior to treatment, the mean monthly EPO dose was 82,067 ± 47,906 and post treatment, the mean EPO usage was 65,495 ± 39,691.
Each patient had a thorough review of his or her past medical history and current medications. Inclusion criteria included HD duration of at least 6 months, age greater than 18 years, and the ability to provide written informed consent. Exclusion criteria included factors known to affect vitamin B12 stores, including: a history of hematological cancer, methotrexate use, alcohol ingestion of more than two drinks per day, vegetarian diet, previous gastric surgery, inflammatory bowel disease, pernicious anemia, recent blood transfusion, or patients receiving B12 supplementation.
Screening began with measurement of serum vitamin B12 concentrations and plasma levels of MMA. All laboratory values were drawn prior to the first HD session of the week and prior to initiation of HD. Those with an MMA level greater than 800 nmol/L had smears of their peripheral blood examined to assess for characteristic findings that are consistent with vitamin B12 deficiency, and the patients with levels less than 800 nmol/L were excluded. Peripheral blood smears were examined by trained hematologists for the presence of oval macrocytic red blood cells (ie, mean corpuscular volume > 100 mL) or the presence of hypersegmented neutrophils (>5 percent of neutrophils with ≥5 lobes or ≥1 neutrophil with ≥6 lobes) as the marker for B12 deficiency. Of the patients screened, 60 were confirmed to be vitamin B12 deficient by smear and high MMA levels, three refused treatment, leaving 57 enrolled in the study.
The enrolled patients were treated with 1000 mcg of intramuscular vitamin B12 weekly for the first month and then monthly for 3 consecutive months. All injections were given in the deltoid muscle prior to the initiation of the hemodialysis session. All patients underwent adjustment of erythropoietin alpha dosing by the treating nephrologist on a bi-weekly basis based on the hemoglobin/hematocrit concentration, as was done for all patients in the unit. The nephrologists were not blinded as to which patients were receiving vitamin B12 supplementation. Other parameters for ESA resistance were addressed which included: iron stores, elevated parathyroid hormone levels, inflammation or infection, and thyroid function.
Enrolled patients were asked to complete a KDQOL-36™ (Kidney Disease Quality of Life Instrument adopted for quality of life assessment for patients with kidney disease) prior to vitamin B12 therapy and were asked to complete the same questionnaire post treatment.
The questionnaire was used to assess if vitamin B12 therapy improved any aspects in quality of life.
Following therapy, serum B12, MMA levels, percent iron saturation, pararthyroid levels, and peripheral blood smears were repeated, and compared to the previous values and blood smears.
Vitamin B12 was analyzed on the Chemiluminescent Immunoassay System (Immulite, Johnson and Johnson, New Brunswick, NJ, USA) and the MMA levels on GC-MS analyzer (DXI, Beckman Coulter Life Science, Indianapolis, IN, USA).
Results
The mean age of the 57 subjects who received vitamin B12 therapy was 63.43 ± 14.6 years. Of those, 33 (58.9%) were females and 23 (41.1%) were males (Table 1). The mean prestudy hemoglobin level was 11.39 g/dL ± 1.28 g/dL (range from 8.5 g/dL to 14.2 g/dL) and the mean poststudy hemoglobin level was 11.48 g/dL ± 1.11 g/dL (8.8 g/dL to 13.5 g/dL) which was not statistically different.
Table 1.
Pre- versus post-KDQOL-36™ (version 1.3)
| Pre-test | Post-test | Change from pre to post | P-value | |
|---|---|---|---|---|
| Symptom/problem list | 76.62 ± 18.60 | 75.69 ± 19.98 | −3.13 ± 14.72 | 0.688 |
| Effects of kidney disease | 52.29 ± 26.08 | 54.58 ± 26.96 | 2.29 ± 9.99 | 0.772 |
| Burden of kidney disease | 43.75 ± 31.25 | 37.50 ± 29.60 | −6.25 ± 17.52 | 0.301 |
| Work status | 26.67 ± 32.00 | 16.67 ± 30.86 | −10.00 ± 20.70 | 0.250 |
| Cognitive function | 71.11 ± 28.91 | 72.44 ± 29.26 | 1.33 ± 28.75 | 0.895 |
| Quality of social interaction | 70.67 ± 26.04 | 79.11 ± 18.15 | 8.44 ± 25.63 | 0.281 |
| Sexual function | 87.50 ± 17.68 | 100.00 ± 0.00 | – | – |
| Sleep | 51.00 ± 23.81 | 51.33 ± 24.03 | 0.33 ± 20.81 | 1.00 |
| Social support | 77.78 ± 32.53 | 77.78 ± 29.99 | 0.00 ± 39.34 | 1.00 |
| Dialysis staff encouragement | 83.33 ± 15.43 | 82.50 ± 16.90 | −0.83 ± 21.89 | 0.943 |
| Overall health | 54.67 ± 24.46 | 60.00 ± 27.77 | 5.33 ± 19.95 | 1.00 |
| Patient satisfaction | 71.11 ± 22.24 | 62.22 ± 17.21 | −8.89 ± 15.26 | 0.090 |
| Physical functioning | 39.33 ± 30.41 | 37.00 ± 27.37 | −2.33 ± 17.10 | 0.391 |
| Role – physical | 28.33 ± 38.81 | 40.00 ± 40.97 | 11.67 ± 43.16 | 0.438 |
| Pain | 55.83 ± 36.57 | 65.83 ± 33.54 | 10.00 ± 36.29 | 0.424 |
| General health | 36.92 ± 17.97 | 44.33 ± 24.56 | 7.42 ± 15.81 | 0.169 |
| Emotional well-being | 68.00 ± 21.43 | 64.00 ± 20.51 | −4.00 ± 23.71 | 0.858 |
| Role – emotional | 35.56 ± 44.48 | 55.56 ± 46.58 | 20.00 ± 46.80 | 0.156 |
| Social function | 56.67 ± 29.07 | 67.50 ± 24.91 | 10.83 ± 19.40 | 0.047 |
| Energy/fatigue | 40.33 ± 27.48 | 48.00 ± 17.61 | 7.67 ± 21.29 | 0.084 |
| SF-12 physical composite | 34.06 ± 8.81 | 36.12 ± 9.44 | 2.06 ± 8.63 | 0.583 |
| SF-12 mental composite | 41.88 ± 11.45 | 44.83 ± 11.18 | 2.94 ± 9.84 | 0.358 |
Abbreviations: KDQOL, Kidney Disease Quality of Life Instrument; SF-12, short form health survey.
Table 1 shows the mean pre- and post-KDQOL-36™ results, along with the corresponding mean absolute difference and P-values using the Wilcoxon signed-rank test. Of the 22 items, only Social function significantly increased from baseline (56.7 ± 29.1) to post-treatment (67.50 ± 24.91); the mean difference (10.8 ± 19.4) was statistically significantly different from zero (P = 0.047).
Although some of the item scores increased or decreased qualitatively, these changes were not statistically significant.
The definitive diagnosis of vitamin B12 deficiency in our study was based on characteristic findings on peripheral blood smear. Low serum vitamin B12 concentration (vitamin B12 < 180 mg/mL) alone was observed in 0.76% (1/132) of the total patients. Using serum MMA levels (.800 mg/dL) as a marker, we found 92.42% (122/132) of the patients were B12-deficient. However, peripheral smears indicated that 58.25% (60/103) of the patients had characteristic findings of vitamin B12 deficiency in the population where MMA was elevated.
Prior to treatment there was no relationship between MMA and blood smears, where only 58.25% of patients had MMA levels > 800. After treatment with vitamin B12 injections, MMA levels and smears were reevaluated. We found that 63.5% (33/52) were B12-deficient using MMA values as the criterion, while 31% (16/52) were B12-deficient by the smear criterion after therapy. There was no agreement between the two tests (P < 0.0011) (Table 2).
Table 2.
Parameters variation over time
| Patients | June | July | Aug | Sep | Oct | Nov | Dec | Jan |
|---|---|---|---|---|---|---|---|---|
| Average | ||||||||
| Hb | 11.0004 | 11.1028 | 11.1662 | 11.3801 | 11.2372 | 11.5596 | 11.3173 | 11.433 |
| Hct | 34.2002 | 34.4475 | 33.9919 | 35.1682 | 34.8405 | 35.5798 | 35.2231 | 35.4144 |
| Iron level | 57.4028 | 54.2587 | 50.3166 | 57.1152 | 52.4026 | 63.7367 | 58.9734 | 68.9288 |
| Sat | 28.0183 | 24.9145 | 23.5426 | 26.4711 | 23.5328 | 30.1345 | 27.4087 | 28.7979 |
| Retic Ct | 11.7142 | 11.7768 | 11.792 | 12.1741 | 11.9566 | 12.461 | 12.1573 | 12.3793 |
Abbreviations: Hb, hemoglobin; Hct, hematocrit; Sat, saturation; Retic Ct, reticulocyte count.
In the B12-treated group, the average decrease in mean erythropoietin alpha dose from 3 months prior to treatment compared to 3 months after treatment was 16,572 units ± 41,902 units per month. This mean change was statistically significantly different from zero, P = 0.0082 by the Wilcoxon signed-rank test (Figure 1).
Figure 1.
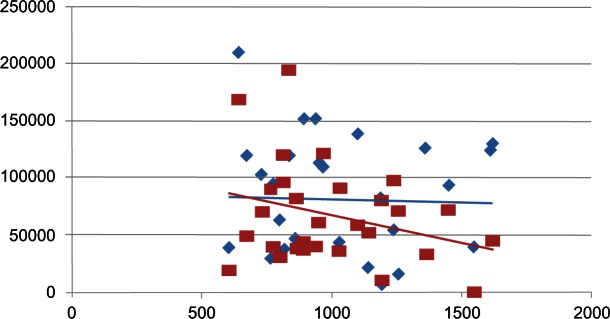
Average decrease in mean erythropoietin alpha dose.
Notes: The average decrease in mean erythropoeitin alpha dose between the losanges (blue), before treatment with vitamin B12 and the squares (red), after treatment with vitamin B12, with the corresponding trendlines.
Several categories on the quality of life questionnaires were assessed for change before and after treatment. While several categories were compared, only social function was found to be significantly different, P = 0.047.
Discussion
Anemia continues to be one of the significant factors affecting the ESRD population; it is common and has a substantial effect on morbidity and mortality. In addition, it places a significant economic burden; the cost to Medicare for ESA alone is estimated at two billion US dollars per year.
The prevalence of vitamin B12 deficiency in this population has not been determined in the past and is likely due to the lack of adequate and interpretable tests.8 The gold standard, bone marrow biopsy, is very invasive, and no other tests have been examined in this population where serum biomarkers can vary so greatly from that of the general population. In our study, a serum vitamin B12 level was not specific for vitamin B12 deficiency, as even patients with very high levels were found to be deficient. There were too few patients with low levels to determine sensitivity. In the general population, MMA is a superior marker for vitamin B12 deficiency. In patients with renal dysfunction it has been reported to be elevated, but presumed not to exceed levels greater than 800 nmol/L.6 In our data, a high MMA level was not specific for B12 deficiency, and since we did not check peripheral smears on patients whose MMA levels were low, we are unable to draw conclusions about sensitivity.
We used peripheral blood smears as our gold standard for deficiency and we found the prevalence in our population to be 58%. All the patients who were treated did experience a drop in MMA levels measured after treatment, likely further signifying that B12 stores improved.
There are numerous factors that can influence anemia and erythropoietin alpha dosing, including vitamin supplementation.10 In our study we were able to determine that the addition of vitamin B12 may help in lowering the overall erythropoietin alpha requirements in HD patients independent of other factors. We were able to determine that a short duration of vitamin B12 supplementation was able to reduce the cumulative monthly erythropoietin alpha requirement by 16,572 units ± 41,902 units which was significantly different from the group not treated (P = 0.014). Further, we noticed that at a certain period after cessation of the vitamin B12 dosing, the patients who were confirmed to be vitamin B12 deficient began to require more erythropoietin alpha. The effect of vitamin B12 is likely to be short lived in this population. In addition to restricted food products allowable in our population, vitamin B12 is actively removed by hemodialysis with high flux membranes. In addition, we had several patients (16/52) who were confirmed to continue to be vitamin B12 deficient by smear criterion. This is felt to be a result of the limited time frame of the study, and we would expect those patients to improve with continued supplementation as body stores are more fully repleted. The mean hemoglobin levels in the patients remained the same after vitamin B12 supplementation. This indicates that the decrease in erythropoietin alpha, was truly a decrease in the erythropoietin alpha requirement.
Patients on dialysis suffer from numerous factors that impact upon their daily life and overall function. We administered the KDQOL-36™ questionnaire to our patients to determine if there is any benefit on their overall daily life with supplementation of vitamin B12 and lower erythropoietin alpha dosing. The only significant improvement we observed was in social function (P = 0.047). While the decrease in erythropoietin alpha dose would not be expected to affect the quality of social function, this may be due to other salutary effects of vitamin B12 repletion in a deficient population. Further, the limited time frame may have influenced the lack of impact upon quality of life and function.
Conclusion
Our study showed a reduction in erythropoietin alpha dosing with B12 in the patients we determined to be deficient. Importantly, there were no side effects or toxicities associated with the vitamin B12 injections aside from local site pain. While this was only a short pilot study, longer treatment might improve anemia, ESA sensitivity and overall quality of life in patients on HD. Decreasing ESA dosing could decrease strokes and would certainly improve a significant financial burden. While further research is needed, we believe our study indicates that vitamin B12 deficiency needs to be addressed in the HD population and particularly those requiring high doses of ESA.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Foley RN, Curtis BM, Parfrey PS. Erythropoietin therapy, hemoglobin targets, and quality of life in healthy hemodialysis patients: a randomized trial. Clin J Am Soc Nephrol. 2009;4(4):726–733. doi: 10.2215/CJN.04950908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tefferi A, Pruthi RK. The biochemical basis of cobalamin deficiency. Mayo Clin Proc. 1994;69(2):181–186. doi: 10.1016/s0025-6196(12)61046-5. [DOI] [PubMed] [Google Scholar]
- 3.Stabler SP, Lindenbaum J, Allen RH. The use of homocysteine and other metabolites in the specific diagnosis of vitamin B-12 deficiency. J Nutr. 1996;126(4):1266S–1272S. doi: 10.1093/jn/126.suppl_4.1266S. [DOI] [PubMed] [Google Scholar]
- 4.van Guldener C. Why is homocysteine elevated in renal failure and what can be expected from homocysteine-lowering? Nephrol Dial Transplant. 2006;21(5):1161–1166. doi: 10.1093/ndt/gfl044. [DOI] [PubMed] [Google Scholar]
- 5.Khoueiry G, Waked A, Goldman M, et al. Dietary intake in hemodialysis patients does not refect a heart healthy diet. J Ren Nutr. 2011;21(6):438–447. doi: 10.1053/j.jrn.2010.09.001. [DOI] [PubMed] [Google Scholar]
- 6.Herrmann W, Schorr H, Geisel J, Riegel W. Homocysteine, cystathionine, methylmalonic acid and B-vitamins in patients with renal disease. Clin Chem Lab Med. 2001;39(8):739–746. doi: 10.1515/CCLM.2001.123. [DOI] [PubMed] [Google Scholar]
- 7.Moelby LK, Rasmussen K, Rasmussen H. Serum methylmalonic acid in uraemia. Scand J Clin Lab Invest. 1992;52(4):351–354. doi: 10.1080/00365519209088369. [DOI] [PubMed] [Google Scholar]
- 8.Moelby L, Rasmussen K, Ring T, Nielsen G. Relationship between methylmalonic acid and cobalamin in uremia. Kidney Int. 2000;57(1):265–273. doi: 10.1046/j.1523-1755.2000.00831.x. [DOI] [PubMed] [Google Scholar]
- 9.Hvas AM, Juul S, Gerdes LU, Nexo E. The marker of cobalamin deficiency, plasma methylmalonic acid, correlates to plasma creatinine. J Intern Med. 2000;247(4):507–512. doi: 10.1046/j.1365-2796.2000.00632.x. [DOI] [PubMed] [Google Scholar]
- 10.Johnson DW, Pollock CA, Macdougall IC. Erythropoiesis-stimulating agent hyporesponsiveness. Nephrology (Carlton) 2007;12(4):321–330. doi: 10.1111/j.1440-1797.2007.00810.x. [DOI] [PubMed] [Google Scholar]
- 11.Zachee P, Chew SL, Daelemans R, Lins RL. Erythropoietin resistance due to vitamin B12 deficiency. Case report and retrospective analysis of B12 levels after erythropoietin treatment. Am J Nephrol. 1992;12(3):188–191. doi: 10.1159/000168443. [DOI] [PubMed] [Google Scholar]


