Abstract
Background
In order to improve adherence to treatment guidelines and performance indicators advocating tight control of disease activity in rheumatoid arthritis (RA), it is important to gain insight into the factors influencing rheumatologists’ decisions whether or not to escalate care.
Objective
To determine the influence of specific attributes relative to a validated measure of disease activity (DAS) on rheumatologists’ decision to escalate care.
Methods
We used a computer-based choice-based conjoint (CBC) analysis survey to determine the relative importance of six attributes on rheumatologists’ decisions related to escalation of care in RA. We administered the survey in a convenience sample of rheumatologists attending the 2008 ACR national meeting. Utilities were calculated using hierarchical Bayes modeling and these results were used to calculate the relative importance of each attribute.
Results
Rheumatologists assigned the most importance to the DAS score (relative importance of 30.7%) in their decision to escalate care. The age of the patient (21.5%) and erosions (20.5%) were rated as equally important in this decision. The decision to escalate care was least influenced by change in symptoms reported by the patient (11.1%), current treatment (8.9%) and disease duration (7.4%).
Conclusion
Our findings suggest that rheumatologists endorse the DAS as a means to guide decision making in RA. We also found that age and erosions are important influences on rheumatologists’ decision to escalate care in RA. Our results add to the literature supporting age bias in RA and suggest that further research is needed to determine how age affects quality of care in clinical practice.
Keywords: Rheumatoid Arthritis, preferences, choice based conjoint analysis, treatment options
INTRODUCTION
Current guidelines advocate intensive care with disease modifying anti-rheumatic drugs (DMARDs) in order to achieve and maintain tight control of disease activity in rheumatoid arthritis (RA). This recommendation is based on studies demonstrating that tight control of disease activity improves long-term outcomes (1–5). As a result, it is now recommended that rheumatologists use validated measures to monitor disease activity over time and adjust treatment as required (6–8). Despite the widespread endorsement of this approach, data suggest that many RA patients are not effectively treated with DMARDs (1). This finding persists even among insured patients under the care of a rheumatologist, indicating that factors over and above access to services may adversely affect quality of care in RA (9).
A recent study by Wolfe and Michaud (10) highlighted the potential effect of patient-related factors in clinical practice. In this study, the authors found that 71% of RA patients were satisfied with their current care and would not want to change medications despite objective findings of active disease. Other studies have found that physician-related factors also play an important role. In one study, where treatment was escalated in only 14% to 18% of patients with moderate to high disease activity who had been on their current DMARD regimen for at least three months, rheumatologists’ explained that they wanted to continue to wait until the maximum potential effect of current DMARDs could been obtained or that they felt the patient’s RA disease activity to be too low to warrant escalation of care despite a DAS score indicating moderate to severe disease activity (1;11).
In order to improve adherence to treatment guidelines and performance indicators advocating complete suppression of inflammation in RA, it is important to gain further insight into the factors influencing rheumatologists’ decisions on whether or not to escalate care. The objective of this study was to determine the influence of specific factors relative to a validated measure of disease activity (DAS) on rheumatologists’ decision to escalate care.
In order to quantify the impact of specific factors on physicians’ decision making, we used a computer-based choice-based conjoint (CBC) analysis survey. CBC assesses preferences by asking respondents to choose a preferred option from a set of hypothetical choices described by a predefined list of attributes. Subsequent analyses based on each respondent’s choices generate a set of conjoint "utilities" from which the relative importance of each attribute can be quantified. CBC is favored by many researchers over other preference measures, because choosing from a small number of alternative items is a simple and natural task that reflects what consumers actually do when deciding between multiple choices (12;13).
METHODS
Subjects
We conducted a survey of a convenience sample of rheumatologists attending the 2008 American College of Rheumatology meeting in San Francisco, California. Subjects were approached by one of two medical research scientists (WK, LvH) and asked to complete a CBC survey on a laptop computer. Eligibility criteria included: currently actively practicing adult rheumatology and able to read and understand English.
CBC Survey
The CBC survey was designed, conducted and analyzed using Sawtooth software, Choice Based Conjoint, version 6.0 (Sawtooth Software, Sequim, WA). The objective of the study was to examine the relative influence of a specified set of attributes on physicians’ decision making. Five attributes were initially selected by expert opinion (LF and PvR) to be included in the survey: patient age, change in symptoms, change in erosions, disease activity score as measured by the DAS-28, and current treatment (Table 1). Age was included because it has been previously shown to influence treatment decisions in RA (14). Current treatment was included based on the investigators’ hypothesis that rheumatologists’ would be more likely to escalate care for patients with multiple remaining options (for example, a patient who had failed their first biologic) than for patients with fewer remaining options (for example a patient who had failed two or more biologics). Six practicing rheumatologists from the Radboud University Nijmegen Medical Centre pilot tested the designed survey and confirmed that these five attributes were those most relevant to practicing rheumatologists’ decision making in RA. Some suggested adding disease duration to the attribute list, which was complied with by the investigators. Each attribute was described using three levels (or estimates) as shown in Table 1.
Table 1.
Attributes and levels included in the CBC survey
| Attribute | Level |
|---|---|
| Age | 1. 80 years old; |
| 2. 50 years old; | |
| 3. 25 years old | |
| Disease duration | 1. RA diagnosed 2 years ago; |
| 2. RA diagnosed 5 years ago; | |
| 3. RA diagnosed 10 years ago | |
| Clinical symptoms | 1. Pain, swelling, stiffness somewhat better than previous visit |
| 2. Pain, swelling, stiffness the same as previous visit | |
| 3. Pain, swelling, stiffness somewhat worse than previous visit | |
| Joint damage | 1. No erosions on recent x-rays |
| 2. No progression of erosions over the past year | |
| 3. Some progression of erosions over the past year | |
| Disease activity | 1. DAS today is 2.0 (low); |
| 2. DAS today is 3.0 (moderate); | |
| 3. DAS today is 3.8 (high) | |
| Current treatment | 1. On first TNF inhibitor |
| 2. On second TNF inhibitor; | |
| 3. Failed all TNF inhibitors now on abatacept |
Respondents were asked to respond to eight CBC choice sets. Given the number of attributes (six) and the number of possible levels per attribute (three), the total number of possible combinations was 36=729. We therefore used the software’s complete enumeration strategy to construct the eight choice sets. This strategy constructs options by randomly assigning levels to each option. The complete enumeration method conforms to three main principles:
Minimal Overlap: Each level is shown as few times as possible in a single task.
Level Balance: Each level is shown approximately an equal number of times across the choice tasks.
Orthogonality: The level of one characteristic is chosen independently of the levels of other characteristics, so that each characteristic level’s effect can be reliably estimated.
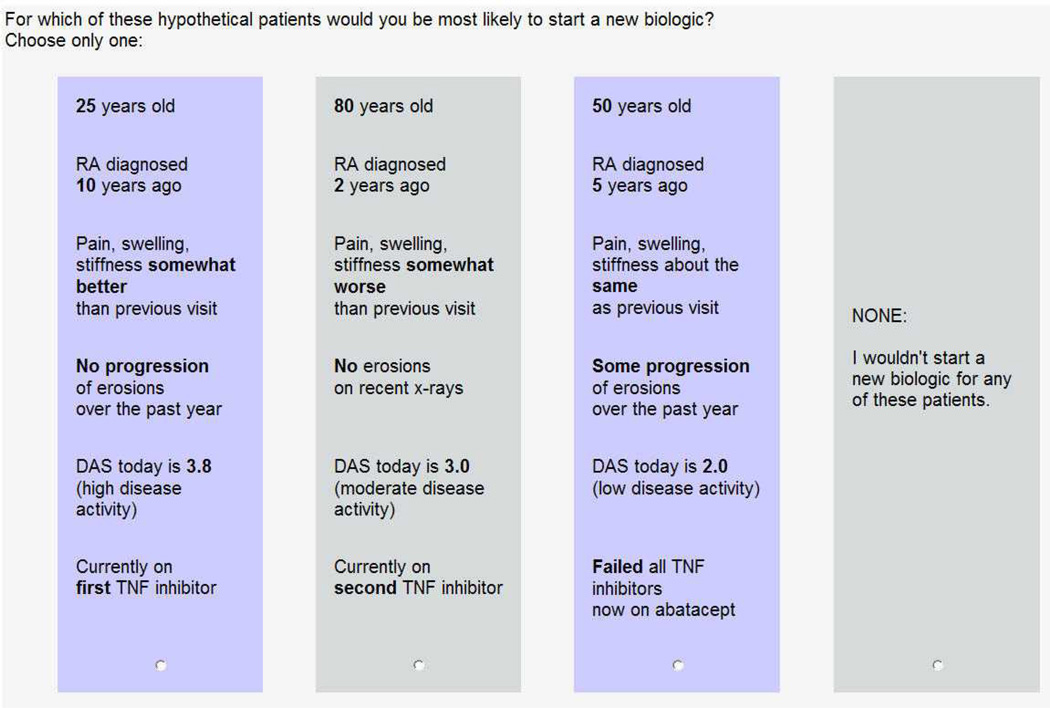
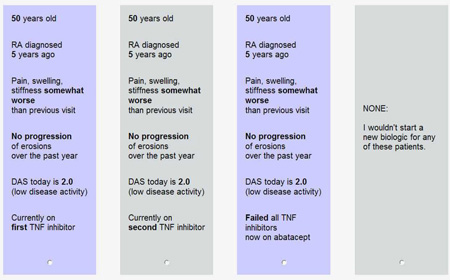
An example of one of the choice sets is shown in Figure 1. Before starting the task, respondents read the following introduction:
Figure 1.
An example of one of the choice sets
Thank you very much for taking the time to help us. We are interested in learning about how rheumatologists make decisions. In order to answer the following questions, imagine that you are seeing a patient with seropositive rheumatoid arthritis. The patient has failed traditional DMARDS and is now been on maximum doses of methotrexate and a TNF inhibitor for 6 months.
The patient has:
no other medical conditions
no trouble performing activities of daily living (such as bathing / dressing)
a little difficulty doing moderate activities (such as pushing a vacuum cleaner / bowling)
a little difficulty performing work and other activities outside of the house
In order to define a specific clinical scenario for which the therapeutic options would be limited, we specified that the patient was on a TNF inhibitor for 6 months after having failed traditional DMARDs, so that escalation of care would be limited to starting a new biologic. The question for each choice set was: “For which of these hypothetical patients would you be most likely to start a new biologic? Choose only one.” Each choice set included three hypothetical patients and a “None” option. In choosing the CBC settings we first specified the “None” option and then generated a design for 300 versions of the survey. The efficiencies reported were all greater than 0.99.
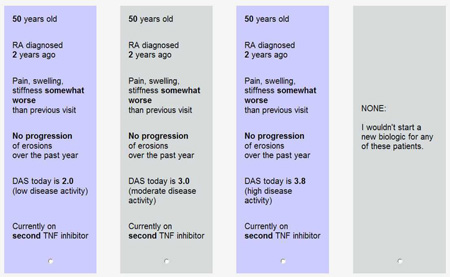
In addition to the eight CBC choice sets where attributes were randomly assigned as per the above described strategy, we included two fixed tasks in which the investigators defined the three options in the choice set. The first (Appendix A) included a dominant choice, to enable the investigators to determine whether or not the respondents were paying careful attention to the information presented. The second was composed to examine the effect of current therapy on likelihood of escalation of care (Appendix B).
After the respondents completed the CBC survey, we collected data on physician age, years of experience, gender, location (continent) and majority of time spent (patient care, clinical research, basic research or administration).
Statistical Analysis
For each respondent, utilities (values) were calculated for each level of each attribute using hierarchical Bayes (HB) modeling (Sawtooth CBC/HB system for hierarchical Bayes estimation version 4.0). HB modeling has the advantage that it can better incorporate heterogeneity between respondents’ choices (15–17). In HB modeling the samples averages (prior information) are used to update the individual utilities in a number of iterations until the samples averages stop changing between iterations. After this convergence the cycle is run a few thousand more times and the estimates of each iteration are saved and averaged. The iterations started with a made-up sample mean of 0 for all levels (15–17). Utilities were entered in SAS software, version 8.2 (SAS Institute, Cary, NC) and merged with the respondents’ characteristics. We calculated the percentage of importance that respondents assigned to each attribute by dividing the range of utilities for each attribute by the sum of the ranges and multiplying by 100.
We first report the distribution of subject’s relative importance and characteristics using descriptive characteristics. To test possible relationships between respondents’ characteristics and the relative importances assigned to specific attributes, we performed Pearson correlations for continuous data and t-test or general linear modeling for dichotomous or categorical data, respectively. An assumption underlying the calculation of the utilities per attribute is that there is a linear relationship between the utilities for each level and the level itself. This assumption was tested by plotting the mean utilities per level for each attribute. The levels with the lowest and highest utilities for the escalation of care were grouped together for this plot.
RESULTS
Respondents
In total, 135 rheumatologists completed the CBC survey. The mean (SD) age of the sample was 48 (11) years and 63% were men. Respondents reported a mean (SD) of 17 (10) years of experience treating patients. Most spent the majority of their time in clinical practice (77%), whereas 14% spent the majority of their time in clinical research, 7% in basic science research, and 2% in administration. The majority of respondents (53%) were from North America, 33% were from Europe, 8% were from South America, 5% were from Asia and 1% were from Africa.
When presented with the dominant choice (Appendix A), where only the DAS score was varied, 112 (83%) out of the 135 respondents chose to escalate care for the patient having the highest DAS score (the dominant option), 19 (14%) chose the “None” option, and four (3%) did not choose the dominant option.
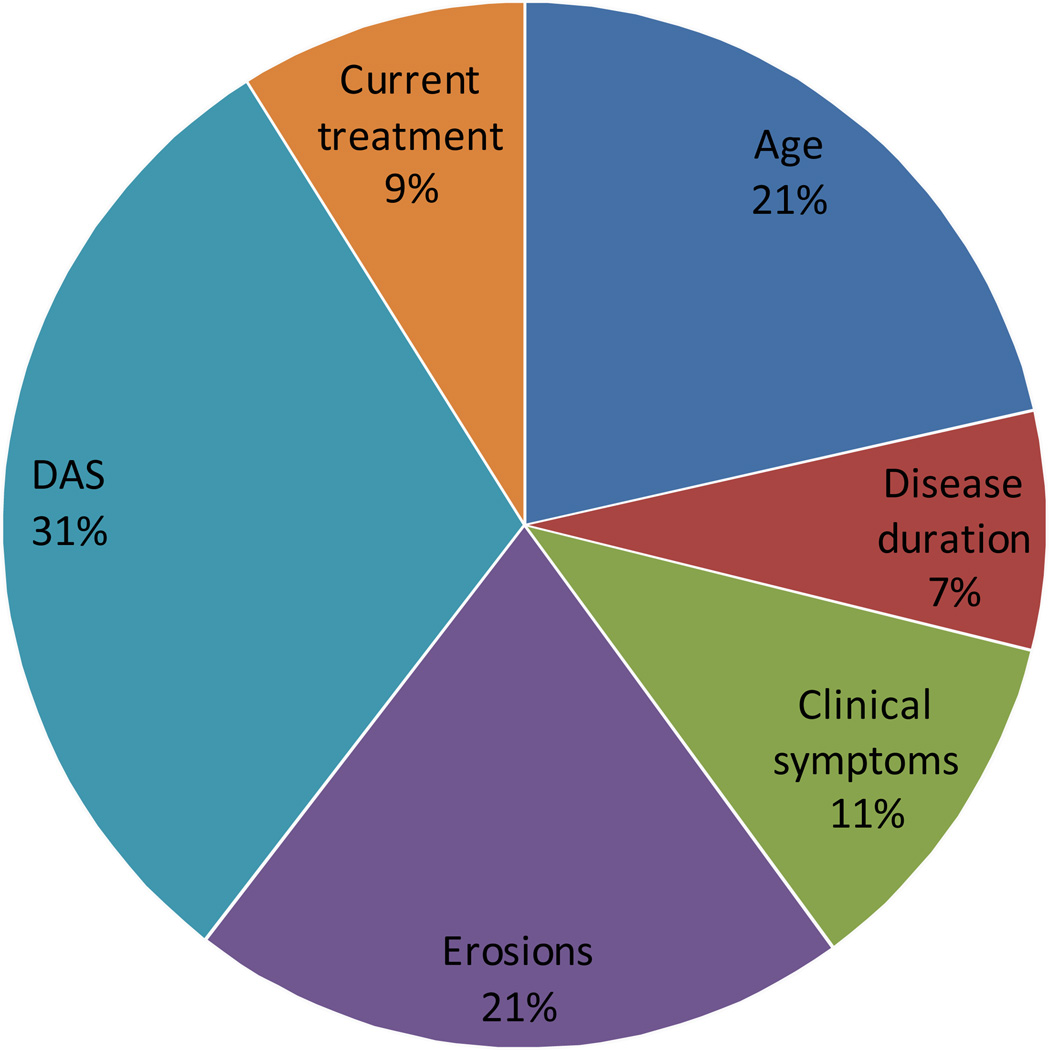
Relative Importance of Attributes
The relative importance of each attribute on rheumatologists’ decision making is reported in Figure 2. Rheumatologists’ decision to escalate care was most strongly influenced by the DAS score (relative importance of 30.7%). The importance of the patient’s age (relative importance of 21.5%) and erosions (relative importance of 20.5%) were similar. Of the attributes included in the CBC survey, the decision to escalate care was least influenced by change in symptoms reported by the patient, current treatment and disease duration.
Figure 2.
Relative importances of all 6 attributes
When presented with the fixed task displayed in Appendix B, in which only current therapy was varied, 31 (23 %) respondents chose the first option (currently on first TNF inhibitor), 5 (4%) the second (currently on second TNF inhibitor) and 10 (7%) the third (failed all TNF inhibitors now on abatacept). Most (89 (66%)) respondents chose not to escalate care for any of the three choices.
Associations between Rheumatologists’ Characteristics and Relative Importances
We found no relationship between physician age (p-value range 0.4–0.8) or years of experience (p-value range 0.3–0.9) and the relative importances (data not shown). However, North-American rheumatologists assigned a higher importance to ‘erosions’ than European rheumatologists and male rheumatologists assigned a higher importance to ‘current treatment’ than female rheumatologists (Table 2). Rheumatologists that spent most of their time in clinical practice assigned a higher importance to erosions and rheumatologists that spent most of their time in research or administration tasks assigned higher importances to the DAS.
Table 2.
Relative importance (means and (sd) values) in different subgroups of rheumatologists
| Attribute | Europe | North- America |
p | Male | Female | p | Clinical practice |
Other | P |
|---|---|---|---|---|---|---|---|---|---|
| Age | 22.5 (8.2) | 20.5 (6.5) | 0.2 | 21.5 (7.6) | 21.5 (6.7) | 1.0 | 19.5 (6.0) | 22.1 (7.5) | 0.09 |
| Disease duration | 7.4 (5.1) | 6.8 (4.1) | 0.5 | 7.6 (4.8) | 6.9 (4.3) | 0.4 | 6.8 (4.8) | 7.5 (4.6) | 0.4 |
| Clinical symptoms | 10.3 (5.2) | 11.9 (6.1) | 0.1 | 10.6 (5.8) | 12.1 (5.6) | 0.1 | 12.8 (6.1) | 10.7 (5.6) | 0.07 |
| Joint damage | 18.9 (7.9) | 23.0 (9.9) | 0.02 | 19.2 (8.6) | 22.5 (10.1) | 0.05 | 17.3 (8.4) | 21.4 (9.4) | 0.03 |
| DAS score | 32.5 (10.1) | 29.1 (9.6) | 0.07 | 31.5 (10.4) | 29.4 (9.0) | 0.2 | 34.2 (8.4) | 29.7 (10.1) | 0.03 |
| Current treatment | 8.5 (3.9) | 8.7 (5.2) | 0.8 | 9.6 (5.1) | 7.6 (4.0) | 0.02 | 9.4 (4.6) | 8.7 (4.9) | 0.5 |
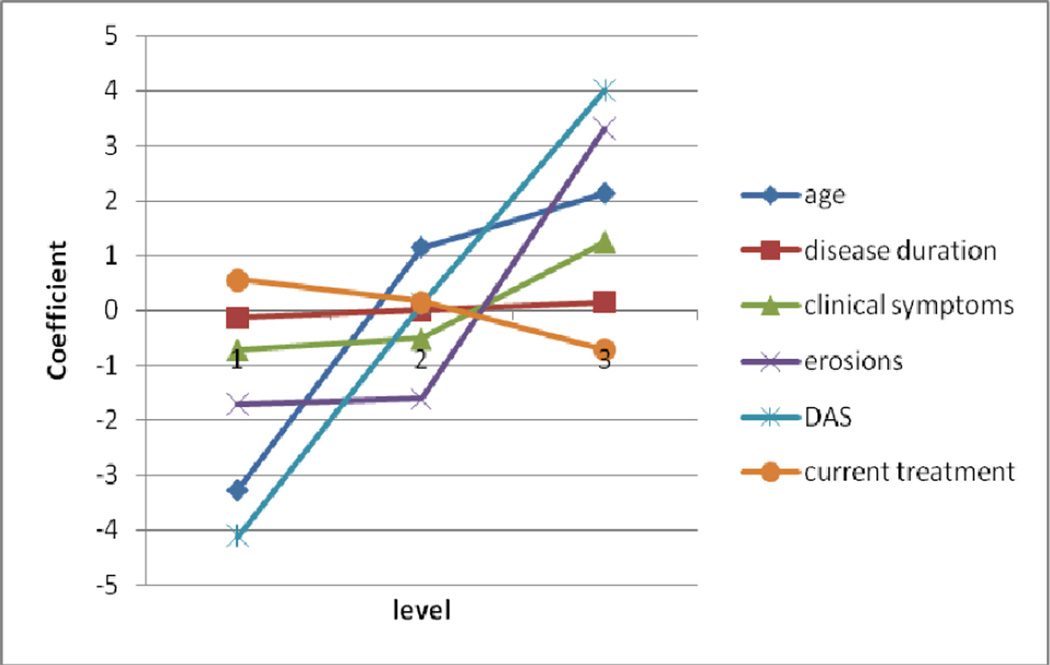
Linearity of Utilities
Figure 3 plots rheumatologists’ utilities for each level of each attribute. The importance assigned to each attribute is reflected by the range of the levels illustrated in the graph. Rheumatologists were less likely to escalate care for the 80 year old patient, but did not distinguish between the 25 and 50 year old patient. The graph also demonstrates that although rheumatologists were strongly influenced by the progression of erosions, they did not differentiate between the absence of erosions and the presence of stable erosions. In contrast, to the preceding non-linear relationships, rheumatologists assigned incremental value to each level of the DAS.
Figure 3.
Relationship between the utilities per level per attribute and the actual level
Age: 1=80 years old; 2=50 years old; 3= 25 years old
Disease duration: 1=RA diagnosed 2 years ago; 2=5 years ago; 3=10 years ago
Clinical symptoms: 1=Pain, swelling, stiffness about somewhat better than previous visit; 2=the same as previous visit; 3= somewhat worse than previous visit (level 1 and 2 are switched for this graph)
Erosions: 1= No erosions on recent x-rays; 2= No progression of erosions over the past year; 3= Some progression of erosions over the past year
DAS: 1= DAS today is 2.0 (low); 2= DAS today is 3.0 (moderate); 3= DAS today is 3.8 (high)
Current treatment: 1=On first TNF inhibitor; 2= On second TNF inhibitor; 3=Failed all TNF inhibitors now on abatacept
DISCUSSION
In this study, we found that the disease activity defined by the DAS score was the most important attribute in rheumatologists’ decision to escalate care relative to the other attributes included in the CBC survey. However age and change of erosions were also influential. We found a reluctance to escalate care for patients 80 years of age and a strong preference to be more aggressive in patients with progression of erosions.
The relationship of age and decision making in RA is consistent with previous studies demonstrating a possible age bias in RA (14;18). Fraenkel et al performed a scenario-based survey which demonstrated that, all else being exactly equal, rheumatologists were more likely to prefer aggressive DMARD treatment for a younger RA patient (28 years of age) than an older RA patient (82 years of age) (14). Analyses based on data from a large clinical practice registry showed that older RA patients (greater than 65 years of age) were less likely to receive anti-TNFα treatment within an equal period of time compared to younger patients, after controlling for disease activity, disease duration and co-morbidities (18). The results suggest that rheumatologists weigh the risks and benefits of potential treatment differently in older compared to adults with RA. Further research into the potential age bias in RA is warranted given that TNFα-antagonists have substantial efficacy in older adults with RA (19–22), and, for many, the expected benefits will most likely outweigh the potential increased risks of adverse events (20–23).
We found that progression of erosions also strongly influenced rheumatologists’ decision to escalate care. This finding is not surprising, because there is a strong relationship between disease activity, progression of erosions and long-term outcomes (24;25). However, what is more surprising is the relative lack of influence of the change in patients’ symptoms on rheumatologists’ decision to escalate care as demonstrated both by the relative importances generated by the random tasks and responses to the first fixed choice task. In the latter, all hypothetical patients were set to have ‘somewhat worsening of pain, swelling and stiffness’ and ‘no progression in erosions’. The DAS score varied from low disease activity to high disease activity. A substantial percentage (14%) of respondents chose not to escalate care in any of the patients, which supports that a high disease activity in combination with worsening of clinical symptoms, but less objective evidence of disease progression, is not sufficient for some rheumatologists to escalate care. This may be justified given recent studies demonstrating a discrepancy between objective and subjective measures of disease activity (26–28). Moreover, the benefits of escalating care based on subjective reports which are not supported by objective clinical findings and/or validated disease activity measures are not known.
Clinical experience suggests that it may be easier to escalate care when multiple options are available than when the patient has already failed several biologics and has fewer options left (29). In this study, the number of remaining treatment options did influence rheumatologists’ choices, although current therapy had less influence on decision making than other attributes. Furthermore, in the second fixed task examining the effect of current therapy on likelihood of escalation of care, most respondents chose not to escalate care for any of the three choices, which can be explained by the low disease activity in all three choices. The fact that some respondents chose to escalate care in patients with fewer remaining treatment options (choice 2 and 3) may be due to that number of biologicals failed acting as a surrogate for disease activity.
The second objective of this study was to explore possible differences in relative importance between groups of physicians. We found that North-American rheumatologists and the rheumatologists that spent most of their time in clinical practice assigned a higher relative importance to erosions than the European rheumatologists or rheumatologists that spent most of their time in research or administration, respectively. This finding is likely due to differences between rheumatologists in diverse work settings. For reasons which are not clear, male rheumatologists assigned a higher importance to ‘current treatment’ than female rheumatologists. We found no other associations between the relative importances and physicians’ characteristics. This lack of variability supports the generalizability of our results.
To the best of our knowledge, this is the first paper to quantify the relative importance of salient attributes on rheumatologists’ decisions to escalate care in RA. CBC is a well-established method and has been used to elicit preferences in a variety of domains in health care (12). An important advantage of CBC is that it minimizes bias associated with the context in which the decisions are made. However, there are several important limitations of this study. First, as with other studies involving scenarios, stated preferences cannot be assumed to reflect decisions made in clinical practice which involve many other important issues. A comparison of stated versus revealed preferences should be examined in future studies. Furthermore, the implications of our findings are limited to the specific attributes included in the choice task. Future research should examine other factors that might impact on escalation of care in clinical practice. In addition,, because we were not able to obtain information on non-participants, we were not able to determine whether there were any significant differences between the rheumatologists who agreed to complete the survey versus those who refused or those who were not asked. Next, although the efficiencies reported after generation of the design were high, both the generalizability and stability of our estimates would have been greater had we been able to recruit a greater number of physicians. Finally, the order of attributes as displayed did not differ between the choice sets. Therefore we cannot exclude whether the strong influence of age is the results of the fact that it was always shown as the first attribute. However, the influence of age on prescribing patterns is consistent with other published studies (14;18).
In conclusion, we found that in addition to disease activity as measured by the DAS, age and erosions are also important influences on rheumatologists’ decision to escalate care in RA in hypothetical patients. These findings suggest that rheumatologists endorse the DAS as a means to guide decision making in RA. Our results also add to the literature supporting age bias in RA and suggest that further research is needed to determine how age affects quality of care in clinical practice.
Acknowledgment
This research was supported by a grant from the Dutch Society for Rheumatology (Rheumatology Grant 2008)
Appendix A
First fixed choice set
Appendix B
Second fixed choice set
REFERENCE LIST
- 1.Fransen J, Moens HB, Speyer I, Van Riel PLCM. Effectiveness of systematic monitoring of rheumatoid arthritis disease activity in daily practice: a multicentre, cluster randomised controlled trial. Annals of the Rheumatic Diseases. 2005;64(9):1294–1298. doi: 10.1136/ard.2004.030924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Goekoop-Ruiterman YPM, de Vries-Bouwstra JK, Allaart CF, van Zeben D, Kerstens PJSM, Hazes JMW, et al. Clinical and radiographic outcomes of four different treatment strategies in patients with early rheumatoid arthritis (the BeSt study) - A randomized, controlled trial. Arthritis and Rheumatism. 2005;52(11):3381–3390. doi: 10.1002/art.21405. [DOI] [PubMed] [Google Scholar]
- 3.Grigor C, Capell H, Stirling A, McMahon AD, Lock P, Vallance R, et al. Effect of a treatment strategy of tight control for rheumatoid arthritis (the TICORA study): a single-blind randomised controlled trial. Lancet. 2004;364(9430):263–269. doi: 10.1016/S0140-6736(04)16676-2. [DOI] [PubMed] [Google Scholar]
- 4.Makinen H, Kautiainen H, Hannonen P, Mottonen T, Leirisalo-Repo M, Laasonen L, et al. Sustained remission and reduced radiographic progression with combination disease modifying antirheumatic drugs in early rheumatoid arthritis. Journal of Rheumatology. 2007;34(2):316–321. [PubMed] [Google Scholar]
- 5.Verstappen SMM, Jacobs JWG, van der Veen MJ, Heurkens AHM, Schenk Y, ter Borg EJ, et al. Intensive treatment with methotrexate in early rheumatoid arthritis: aiming for remission. Computer Assisted Management in Early Rheumatoid Arthritis (CAMERA, an open-label strategy trial) Annals of the Rheumatic Diseases. 2007;66(11):1443–1449. doi: 10.1136/ard.2007.071092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Choy EH, Khoshaba B, Cooper D, MacGregor A, Scott DL. Development and validation of a patient-based disease activity score in rheumatoid arthritis that can be used in clinical trials and routine practice. Arthritis & Rheumatism-Arthritis Care & Research. 2008;59(2):192–199. doi: 10.1002/art.23342. [DOI] [PubMed] [Google Scholar]
- 7.Pincus T, Sokka T. Quantitative measures for assessing rheumatoid arthritis in clinical trials and clinical care. Best Pract Res Clin Rheumatol. 2003;17(5):753–781. doi: 10.1016/s1521-6942(03)00077-9. [DOI] [PubMed] [Google Scholar]
- 8.Prevoo MLL, VantHof MA, Kuper HH, Vanleeuwen MA, VandePutte LBA, Vanriel PLCM. Modified Disease-Activity Scores That Include 28-Joint Counts - Development and Validation in A Prospective Longitudinal-Study of Patients with Rheumatoid-Arthritis. Arthritis and Rheumatism. 1995;38(1):44–48. doi: 10.1002/art.1780380107. [DOI] [PubMed] [Google Scholar]
- 9.Schmajuk G, Schneeweiss S, Katz JN, Weinblatt ME, Setoguchi S, Avorn J, et al. Treatment of older adult patients diagnosed with rheumatoid arthritis: improved but not optimal. Arthritis & Rheumatism-Arthritis Care & Research. 2007;57(6):928–934. doi: 10.1002/art.22890. [DOI] [PubMed] [Google Scholar]
- 10.Wolfe F, Michaud K. Resistance to changing therapy: Discordance between RA activity and patients' treatment choices. Arthritis and Rheumatism. 2006;54(9):S425–S426. doi: 10.1002/art.22719. [DOI] [PubMed] [Google Scholar]
- 11.Creemers M, Fransen J, Welsing P, Kievit W, van Riel P. Assessment of the DAS28 in rheumatoid arthritis patients in daily clinical practice: Is monitoring enough to reach low disease activity? Arthritis and Rheumatism. 2005;52(9):S116–S117. [Google Scholar]
- 12.Ryan M, Gerard K, Amya-Amaya M. Using Discrete Choice Experiments to Value Health and Health Care. 1 ed. Springer; 2008. [Google Scholar]
- 13.Ryan M, Farrar S. Using conjoint analysis to elicit preferences for health care. British Medical Journal. 2000;320(7248):1530–1533. doi: 10.1136/bmj.320.7248.1530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fraenkel L, Rabidou N, Dhar R. Are rheumatologists' treatment decisions influenced by patients' age? Rheumatology. 2006;45(12):1555–1557. doi: 10.1093/rheumatology/kel144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Howell J. CBC/HB for beginners. Sawtooth Software research paper series. 2009 Ref Type: Serial (Book,Monograph) [Google Scholar]
- 16.Orme B. Hierarchical Bayes: Why alll the Attention? Sawtooth Software research paper series. 2000 Ref Type: Serial (Book,Monograph) [Google Scholar]
- 17.Sawtooth Software. The CBC/HB System for hierarchical Bayes estimation version 4.0 technical paper. Sawtooth Software research paper series. 2009 Ref Type: Serial (Book,Monograph) [Google Scholar]
- 18.Radovits BJ, Fransen J, Eijsbouts A, Riel van P, Laan RF. Missed opportunities in the treatment of elderly patients with rheumatoid arthritis. Rheumatology (Oxford) 2009;48(8):906–910. doi: 10.1093/rheumatology/kep129. [DOI] [PubMed] [Google Scholar]
- 19.Radovits BJ, Kievit W, Fransen J, van der Laar MA, Jansen TL, van Riel PL, et al. Influence of age on the outcome of anti-TNF{alpha}therapy in rheumatoid arthritis. Ann Rheum Dis. 2008 doi: 10.1136/ard.2008.094730. [DOI] [PubMed] [Google Scholar]
- 20.Bathon JM, Fleischmann RM, van der HD, Tesser JR, Peloso PM, Chon Y, et al. Safety and efficacy of etanercept treatment in elderly subjects with rheumatoid arthritis. J Rheumatol. 2006;33(2):234–243. [PubMed] [Google Scholar]
- 21.Schiff MH, Yu EB, Weinblatt ME, Moreland LW, Genovese MC, White B, et al. Long-term experience with etanercept in the treatment of rheumatoid arthritis in elderly and younger patients: patient-reported outcomes from multiple controlled and open-label extension studies. Drugs Aging. 2006;23(2):167–178. doi: 10.2165/00002512-200623020-00006. [DOI] [PubMed] [Google Scholar]
- 22.Genevay S, Finckh A, Ciurea A, Chamot AM, Kyburz D, Gabay C. Tolerance and effectiveness of anti-tumor necrosis factor alpha therapies in elderly patients with rheumatoid arthritis: a population-based cohort study. Arthritis Rheum. 2007;57(4):679–685. doi: 10.1002/art.22688. [DOI] [PubMed] [Google Scholar]
- 23.Fleischmann R, Baumgartner SW, Weisman MH, Liu T, White B, Peloso P. Long term safety of etanercept in elderly subjects with rheumatic diseases. Ann Rheum Dis. 2006;65(3):379–384. doi: 10.1136/ard.2005.035287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Welsing PM, van Gestel AM, Swinkels HL, Kiemeney LA, van Riel PL. The relationship between disease activity, joint destruction, and functional capacity over the course of rheumatoid arthritis. Arthritis Rheum. 2001;44(9):2009–2017. doi: 10.1002/1529-0131(200109)44:9<2009::AID-ART349>3.0.CO;2-L. [DOI] [PubMed] [Google Scholar]
- 25.Welsing PM, Landewe RB, van Riel PL, Boers M, van Gestel AM, van der LS, et al. The relationship between disease activity and radiologic progression in patients with rheumatoid arthritis: a longitudinal analysis. Arthritis Rheum. 2004;50(7):2082–2093. doi: 10.1002/art.20350. [DOI] [PubMed] [Google Scholar]
- 26.Harrington JT. The Uses of Disease Activity Scoring and the Physician Global Assessment of Disease Activity for Managing Rheumatoid Arthritis in Rheumatology Practice. Journal of Rheumatology. 2009;36(5):925–929. doi: 10.3899/jrheum.081046. [DOI] [PubMed] [Google Scholar]
- 27.Kievit W, Welsing PMJ, Adang EMM, Eijsbouts AM, Krabbe PFM, Van Riel PLCM. Comment on the use of self-reporting instruments to assess patients with rheumatoid arthritis: The longitudinal association between the DAS28 and the VAS general health. Arthritis & Rheumatism-Arthritis Care & Research. 2006;55(5):745–750. doi: 10.1002/art.22225. [DOI] [PubMed] [Google Scholar]
- 28.Wolfe F, Michaud K. Proposed Metrics for the Determination of Rheumatoid Arthritis Outcome and Treatment Success and Failure. Journal of Rheumatology. 2009;36(1):27–33. doi: 10.3899/jrheum.080591. [DOI] [PubMed] [Google Scholar]
- 29.Yazici Y, Krasnokutsky S, Barnes JP, Hines PL, Wang J, Rosenblatt L. Changing Patterns of Tumor Necrosis Factor Inhibitor Use in 9074 Patients with Rheumatoid Arthritis. Journal of Rheumatology. 2009;36(5):907–913. doi: 10.3899/jrheum.080592. [DOI] [PubMed] [Google Scholar]