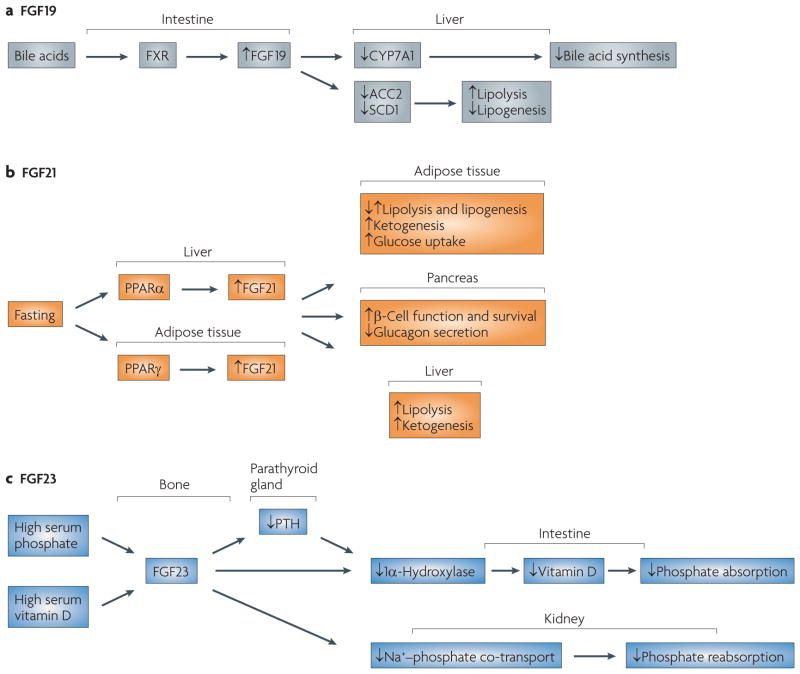
Figure 4. The physiology of fibroblast growth factor 19 (FgF19), FgF21 and FgF23.
a | Bile acids activate the FXR receptor in the intestine, leading to expression of FGF19 in the ileum. FGF19 circulates to the liver, where it acts through FGF receptor 4 (FGFR4) to inhibit bile acid synthesis and lipogenesis. b | FGF21 mediates the fasting response and is regulated by peroxisome proliferator-activated receptor-α (PPARα) and PPARγ in liver and adipose tissue, respectively. The biology of FGF21 in model systems and humans is still being elucidated, but among its many functions are increasing glucose uptake in adipose tissue, improving β-cell function, inhibiting glucagon secretion, increasing ketogenesis and regulating lipolysis and lipogenesis in a complex manner. FGF21 is expressed in liver, adipose and pancreatic tissue. It acts primarily on adipose tissue. The effects of FGF21 on liver function are probably accomplished through indirect mechanisms as it does not signal through FGFR4. c | FGF23 production is upregulated in bone in response to high serum phosphate and vitamin D levels. FGF23 then circulates to the parathyroid gland, intestine and kidney. In the intestine, FGF23 downregulates 1α-hydroxylase so as to reduce the levels of activated vitamin D, thereby inhibiting absorption of phosphate from the diet. The repression of parathyroid hormone (PTH) by FGF23 also helps to downregulate 1α-hydroxylase. In the kidney, FGF23 inhibits Na+–phosphate ion co-transport and thus increases excretion of phosphate. CYP7A1, cytochrome P450 7A1; SCD1, stearoyl CoA desaturase 1.