Abstract
Cardiac rehabilitation exercise prescriptions should be based on exercise stress tests; however, limitations in performing stress tests in this setting typically force reliance on subjective measures like the Duke Activity Status Index (DASI). We developed and evaluated a treadmill-based exercise tolerance test (ETT) to provide objective physiologic measures without requiring additional equipment or insurance charges. The ETT is stopped when the patient's Borg scale rating of perceived exertion (RPE) reaches 15 or when any sign/symptom indicates risk of an adverse event. Outcomes of the study included reasons for stopping; maximum heart rate, systolic blood pressure, and rate pressure product; and adverse events. We tested equivalence to the DASI as requiring the 95% confidence interval for the mean difference between DASI and ETT metabolic equivalents (METs) to fall within the range (–1, 1). Among 502 consecutive cardiac rehabilitation patients, one suffered a panic attack; no other adverse events occurred. Most (80%) stopped because they reached an RPE of 15; the remaining 20% were stopped on indications that continuing risked an adverse event. Mean maximum systolic blood pressure, heart rate, and rate pressure product were significantly (P < 0.001) below thresholds of the American Association of Cardiovascular and Pulmonary Rehabilitation. Two patients’ heart rates exceeded 150 beats per minute, but their rate pressure products remained below 36,000. The mean difference between DASI and ETT METs was −0.8 (−0.98, −0.65), indicating equivalence at our threshold. In conclusion, the ETT can be performed within cardiac rehabilitation, providing a functional capacity assessment equivalent to the DASI and objective physiologic measures for developing exercise prescriptions and measuring progress.
Maximal exercise testing on entry into cardiac rehabilitation (CR) offers the opportunity to identify the metabolic equivalents (METs) (1) that a patient is capable of achieving, which would enable easy determination of a patient's starting MET level. However, lacking the resources to perform maximal exercise tests, most CR programs must determine the starting MET level from the Duke Activity Status Index (DASI) questionnaire or the 6-minute walk test. The 6-minute walk test is an objective measure of exercise tolerance in patients with lung disease and in low-functioning cardiac patients (2), but is not the most challenging test for the majority of patients enrolled in CR. And, while METs can be estimated based on a calculation from the patient's DASI score, our experience shows that some patients overestimate their ability because they were able to perform the tasks queried prior to surgery and, without having attempted that task since surgery, feel that they should still be able to do it, while others underestimate their postsurgery capability. A third alternative, relying on standardized approaches not based on measurements of current exercise capacity to determine exercise intensity (e.g., achieving a heart rate of 20 beats per minute above the resting rate), potentially minimizes the benefit patients derive from exercise training and slows patient progress (3). We, therefore, concluded there was a need for a test that could be easily performed in most CR settings and would provide both a challenge to the majority of patients and physiologic performance data. We sought to develop such a tool to accurately assess the level at which to start each patient's exercise program. As the CR patient population covers a wide range of functional levels, it was important that the tool incorporate the flexibility to meet all needs. This was achieved by providing individualized options and concomitant, appropriate goals for completion of rehabilitation. Here, we evaluate the protocol—the Exercise Tolerance Test (ETT)—developed for both exercise prescription outcomes and effectiveness, comparing it to the DASI scale. This study was approved by the Baylor Research Institute institutional review board.
METHODS
The CR department at The Heart Hospital Baylor Plano opened in January 2007. The program is primarily staffed by three registered nurses and four exercise physiologists, but chaplains and a registered dietician are also involved in patient education. Patients are typically in the program 6 to 8 weeks following hospital discharge and attend classes on each Monday, Wednesday, and Friday. In 2012, the outpatient program Phase II volume was just under 6800 visits. The department also offers inpatient and maintenance programs.
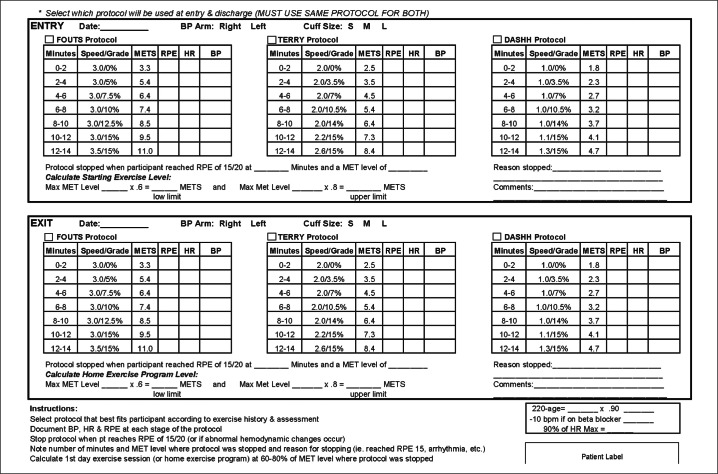
We modified existing stress test protocols to meet the specific needs of the CR setting, developing three different treadmill-based protocols to determine exercise functional capacity (Figure). The ETT was administered in the CR department. The stopping point for all three of the protocols was based on the patient's rating of perceived exertion (RPE) of 15 on the Borg scale (2) or the occurrence of any abnormal hemodynamic changes such as arrhythmia, chest pain, dizziness, decreased blood pressure with increasing exercise, very high blood pressure, extreme shortness of breath, or any other symptom that outweighs the benefit of continuing exercise. As an added precaution, we also calculated the patient's maximum “allowed” heart rate using the %HRmax method (4) (with an additional 10 beats per minute subtracted for patients on beta-blockers) and stopped the patient if 90% of this maximum heart rate was reached.
Figure.
Three different treadmill-based protocols to determine exercise functional capacity.
At each stage of the relevant protocol, blood pressure (measured every 2 minutes), heart rate (based on three-lead electrocardiogram tracing), and RPE were documented. Oxygen saturation and peak oxygen uptake were not monitored. The most challenging protocol moved incrementally from 3.0 mph/0% grade to 3.5 mph/15% grade; the least physically challenging went from 1.0 mph/0% grade to 1.3 mph/15% grade. Patients were assigned METs for every stage for which they completed any portion.
We determined which protocol to use for each patient based on information gathered during the initial patient interview: familiarity with treadmills, age, orthopedic issues, prior/current exercise routine, and height/leg length. From this we chose the most difficult protocol we felt the patient could safely perform for at least 2 minutes. If the interview information was insufficient to make this determination, we started the patient on the treadmill and increased the speed until the patient reported it as a “fast walk” and then started the appropriate protocol from there.
Patients were instructed on the purpose and process of the exercise evaluation test before the protocol was started. The 6–20 Borg RPE scale (5) was reviewed prior to starting the test, and patients were told the test would stop when they reached an RPE of 15 or at any time they felt the need to stop.
For our demonstration of ETT's validity, we considered all patients who entered our CR program between October 30, 2008, and December 29, 2010, and were able to walk on the treadmill. The institutional review board waived informed consent for this study under 45 C.F.R. § 46.116(d).
We examined the rate pressure products patients reached during the ETT to ensure they remained below the threshold of 36,000 (corresponding to a maximum systolic blood pressure of 240 mm Hg and a peak heart rate of 150 beats per minute, both consistent with the American Association of Cardiovascular and Pulmonary Rehabilitation guidelines [2]) (6). The validity of this threshold may be challenged since many CR patients are on beta-blockers, resulting in decreased heart rates. Nevertheless, we believe this endpoint is appropriate: whether a patient's rate pressure product remains ≤36,000 because the ETT is stopped when it reaches that level or because the beta-blockers prevent the maximum being reached, a potentially hazardous level of myocardial work is avoided.
We also examined the reasons for stopping the ETT protocol to determine what proportion of patients stopped for reasons other than reaching the target RPE of 15. The ability of few to reach this target would indicate a need to revise this aspect of the protocol.
Finally, we compared the patients’ MET levels measured by the DASI test to those measured by the ETT to determine whether the ETT provides an estimate of functional capacity that is at least equivalent to this commonly used measure.
Patient demographic data and primary diagnosis prompting referral to the CR program were obtained from administrative records. The remaining data were collected during the initial patient assessment, with patients completing both a DASI questionnaire and one of the three ETT protocols, administered by exercise physiologists and registered nurses. MET levels were calculated from the ETT protocols as shown in the Figure and from the DASI score using the following formula:
Estimated peak oxygen uptake in mL/min = (0.43 × DASI score) + 9.6
MET level = 3.5 × estimated peak oxygen uptake in mL/min
Data were prospectively collected but retrospectively analyzed.
Outcomes were examined using one-sample t tests, comparing mean values for maximum systolic blood pressure, peak heart rate, and the rate pressure product to the thresholds (240 mm Hg, 150 beats per minute, and 36,000, respectively). We used a matched pair equivalence test to determine whether DASI and the ETT could be considered equivalent measurements (7). Based on our knowledge of exercise physiology and experience working with METs and the common methods of assessing functional ability in the CR population, we defined the difference interval as “mean DASI MET ±1” (which was expected to translate into a 25% to 30% interval, depending on the exact mean DASI MET level) as the range of equivalence. We then calculated the 95% confidence interval for the observed difference between the DASI and ETT METs. A confidence interval that fell entirely within the (−1, 1) range was considered to demonstrate equivalence. All analyses were done using SAS 9.2 (Cary, NC).
RESULTS
From October 30, 2008, to December 29, 2010, 504 patients entered our CR program. Two patients were missing necessary data for this study and so were excluded, leaving a final study population of 502 patients. Table 1 shows the demographic characteristics of these patients and the primary diagnoses for which they were referred to CR. Most patients were white men, mean age 62 years. Most had had coronary artery bypass grafting, percutaneous coronary intervention, valve surgery, or combinations of these procedures.
Table 1.
Characteristics of the study population (N = 502)
| Characteristic | |
|---|---|
| Male | 383 (76.3%) |
| Race | |
| White | 428 (85.3%) |
| Hispanic | 15 (3.0%) |
| Black | 13 (2.6%) |
| Asian | 13 (2.6%) |
| Other | 33 (6.6%) |
| Age (mean ± standard deviation; years) | 62 ± 11 |
| Height (mean ± standard deviation; cm) | 168 ± 4 |
| Weight (mean ± standard deviation; kg) | 87.4 ± 8.6 |
| Primary diagnosis | |
| Coronary artery bypass graft | 243 (48.4%) |
| Percutaneous coronary intervention | 120 (23.9%) |
| Valve surgery | 107 (21.3%) |
| Myocardial infarction | 18 (3.6%) |
| Other | 14 (2.8%) |
We observed mean ± standard deviation values for maximum systolic blood pressure, peak heart rate, and rate pressure product of 143 ± 22 mm Hg, 109 ± 21 beats per minute, and 15,717 ± 4308, respectively, in our study population. All mean values were significantly lower than their respective threshold (P < 0.001), and the maximum systolic blood pressure (220 mm Hg) and rate pressure product (31,020) likewise fell below the thresholds of 240 mm Hg and 36,000. Although we did observe heart rates higher than the threshold of 150 beats per minute in two patients (the highest was 160 beats per minute), peak rate pressure products for both these patients were below the 36,000 threshold.
Table 2 shows the reasons patients stopped the ETT protocols. For 80% of the patients, the protocol was stopped because they had reached the target endpoint of an RPE of 15. With the exception of one patient, who suffered a panic attack, the protocol was stopped for the remaining 20% when warning signs indicated that continuing the protocol carried a risk of triggering an adverse event. Other than the panic attack, we observed no adverse events.
Table 2.
Reasons for stopping the Exercise Evaluation Tool protocol among 502 cardiac rehabilitation patients
| Reason for stopping* | n (%) |
|---|---|
| RPE of 15 reached | 412 (82.1%) |
| 90% of heart rate maximum reached | 18 (3.5%) |
| Dyspnea | 14 (2.8%) |
| Orthopedic issues | 12 (2.4%) |
| Drop in blood pressure | 11 (2.2%) |
| Electrocardiogram changes | 10 (2.0%) |
| Chest pain | 6 (1.2%) |
| Increased blood pressure | 6 (1.2%) |
| Patient request | 5 (1.0%) |
| Dizziness/lightheadedness | 3 (0.6%) |
| Reached a maximum allowed heart rate defined by the patient's physician and documented in the patient's chart | 2 (0.4%) |
| Panic attack | 1 (0.2%) |
| Decreased oxygen saturation | 1 (0.2%) |
| Patient completed protocol | 1 (0.2%) |
Target stopping point was a patient's rating of perceived exertion (RPE) of 15. Other reasons for stopping were warning signs that continuing the protocol may carry more risk than benefit.
The mean ± standard deviation MET levels in our population were 6.5 ± 1.8 METs as measured by DASI and 5.7 ± 1.8 METs as measured by the ETT protocols. The mean difference (95% confidence interval) in MET score between the two tests was −0.8 (−0.98, −0.65). Since both the lower and upper confidence bounds were within our predefined equivalence interval (−1, 1), by our criteria, the ETT and DASI are statistically equivalent tests.
DISCUSSION
We developed an ETT to meet the needs of CR programs that, like ours, are unable to routinely perform cardiovascular stress tests for all patients entering the program. Our tool does not require a physician to perform the test but, like the cardiovascular stress test, provides objective, physiological measures from which to accurately assess the patient's functional capacity and so develop an exercise program that is challenging enough to ensure the patient reaps the full benefits of CR.
Based on our observations applying this tool to >500 patients over 2 years, our tool provides an assessment of functional capability at least equivalent to the validated and commonly used DASI questionnaire. In our study population, 80% of patients continued the ETT protocol to reach the target stopping point of an RPE of 15. In the remaining 20%, we stopped the protocol at early indications that an adverse event may be triggered by continuing; the only adverse event we observed was a panic attack experienced by one patient. We also evaluated patients’ peak rate pressure products during protocol administration: the mean maximum value of 15,717 we observed was significantly below the recognized threshold of 36,000, and the highest rate pressure product we observed (31,020) was likewise well below the recognized threshold. An important aspect of our ETT is its provision of three graded protocols, which gives the flexibility needed to test each patient at an appropriately challenging level on program entry, rather than attempting a “one size fits all” model that would require more intense supervision to avoid overextending patients who arrive in poorer physical condition.
The second major aspect of our evaluation of the ETT was to compare it to the DASI as a measure of functional capability in CR patients. We chose the DASI for this evaluation both because it was the method previously used in our program and because the DASI score can be readily converted to a MET level (2) (to which we could compare the ETT results) and has previously been shown to be at least modestly correlated with METs achieved during exercise testing in cardiac patients (r = 0.31, P = 0.0002) (8) and with peak oxygen uptake during exercise testing (Spearman correlation coefficient = 0.58, P < 0.0001) (9). Our analysis showed that the ETT was statistically equivalent to the DASI in assessing functional capability, as defined by the equivalence range we chose: the 95% confidence interval surrounding the mean ETT MET level (5.5 to 5.8) fell well within the predetermined range of equivalence (mean DASI MET ±1 = 5.5 to 7.5). While there is room for debate that the (−1, 1) equivalence range we selected was too broad, we believe it to be appropriate—particularly in light of the subjective nature of the questions from which the DASI score (and associated MET level) is calculated. Given that the mean DASI MET in our study population was 6.5, the (−1, 1) equivalence range translated into an approximately 30% interval—i.e., the mean ETT score needed to be less than 15% higher or lower than the DASI mean to be considered equivalent.
One benefit that we have observed working with the ETT is that it enables us to more effectively assess patients’ signs and symptoms, tailoring their exercise prescriptions accordingly. Additionally, since the same protocol can be used at program exit to assess the patient's gain in functional capability, in the future we can assess our program, which can in turn be used to guide and evaluate initiatives we may implement to increase program effectiveness. Our results, showing a higher mean MET level based on DASI score than ETT protocol, although not significant, also suggest that patients might be overestimating their capabilities on program entry. The ETT can help both patients and CR staff better assess what activities patients can realistically perform and give them confidence in performing these activities so that they neither endanger their own safety nor impose needless limitation on themselves.
One limitation of our study was our inability to compare the ETT to the gold standard of a full exercise stress test. Such an evaluation would be valuable and, assuming positive results, would increase confidence in our method. Some might also consider the use of an RPE of 15 as a termination point for the ETT to be a limitation, as it is both a subjective measure and makes the ETT a submaximal test. However, for our purposes—using a protocol that provides the desired physiological measures for development of a beneficial exercise prescription yet does not require physician involvement, insurance charges, or equipment not typically found in CR programs and demonstrating that this protocol is feasible and provides at least equivalent information to commonly used alternatives—neither comparison to a full exercise stress test, nor a maximal stress test, was necessary. Perceptually regulated exercise testing has been shown to be a valid means of producing consistent, acceptable, and recommended increments in intensity in healthy individuals (10). Future research should investigate its validity in the CR patient population, as CR is a good example of a context in which maximal testing is not always feasible or appropriate, but a valid measure of exercise intensity is needed.
Acknowledgments
The authors thank the staff of the Baylor Heart and Vascular Hospital cardiac rehabilitation program for their contributions in developing the testing protocols, the staff of The Heart Hospital at Baylor Plano cardiac rehabilitation program for their work collecting data used in this study, and Briget da Graca, MS, ELS, for her help with the literature review and writing this paper.
References
- 1.Brooks GA, Fahey TD, Baldwin KM. Exercise Physiology: Human Bioenergetics and Its Applications. Boston, MA: McGraw-Hill; 2005. [Google Scholar]
- 2.American Association of Cardiovascular and Pulmonary Rehabilitation. Guidelines for Cardiac Rehabilitation and Secondary Prevention Programs. Champaign, IL: Human Kinetics; 2004. [Google Scholar]
- 3.Mezzani A, Hamm LF, Jones AM, McBride PE, Moholdt T, Stone JA, Urhausen A, Williams MA. Aerobic exercise intensity assessment and prescription in cardiac rehabilitation: a joint position statement of the European Association for Cardiovascular Prevention and Rehabilitation, the American Association of Cardiovascular and Pulmonary Rehabilitation, and the Canadian Association of Cardiac Rehabilitation. J Cardiopulm Rehabil Prev. 2012;32(6):327–350. doi: 10.1097/HCR.0b013e3182757050. [DOI] [PubMed] [Google Scholar]
- 4.American College of Sports Medicine. ACSM's Guidelines for Exercise Testing and Prescription. Philadelphia, PA: Wolters Kluwer Health; 2009. [DOI] [PubMed] [Google Scholar]
- 5.Borg G. Physical Performance and Perceived Exertion. Lund, Sweden: Gleerup; 1962. [Google Scholar]
- 6.Adams J, Cline MJ, Hubbard M, McCullough T, Hartman J. A new paradigm for post-cardiac event resistance exercise guidelines. Am J Cardiol. 2006;97(2):281–286. doi: 10.1016/j.amjcard.2005.08.035. [DOI] [PubMed] [Google Scholar]
- 7.Jones B, Jarvis P, Lewis JA, Ebbutt AF. Trials to assess equivalence: the importance of rigorous methods. BMJ. 1996;313(7048):36–39. doi: 10.1136/bmj.313.7048.36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bairey Merz CN, Olson M, McGorray S, Pakstis DL, Zell K, Rickens CR, Kelsey SF, Bittner V, Sharaf BL, Sopko G. Physical activity and functional capacity measurement in women: a report from the NHLBI-sponsored WISE study. J Womens Health Gend Based Med. 2000;9(7):769–777. doi: 10.1089/15246090050147745. [DOI] [PubMed] [Google Scholar]
- 9.Hlatky MA, Boineau RE, Higginbotham MB, Lee KL, Mark DB, Califf RM, Cobb FR, Pryor DB. A brief self-administered questionnaire to determine functional capacity (the Duke Activity Status Index) Am J Cardiol. 1989;64(10):651–654. doi: 10.1016/0002-9149(89)90496-7. [DOI] [PubMed] [Google Scholar]
- 10.Eston R, Evans H, Faulkner J, Lambrick D, Al-Rahamneh H, Parfitt G. A perceptually regulated, graded exercise test predicts peak oxygen uptake during treadmill exercise in active and sedentary participants. Eur J Appl Physiol. 2012;112(10):3459–3468. doi: 10.1007/s00421-012-2326-8. [DOI] [PubMed] [Google Scholar]