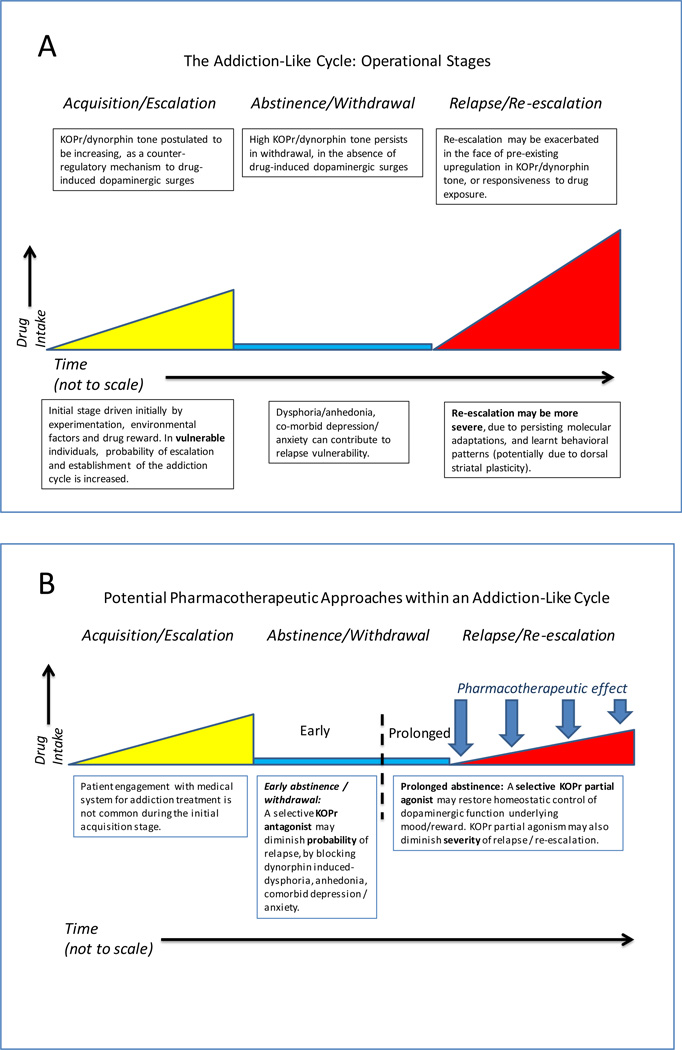
Figure Legend 1. Different stages of the addiction cycle and potential KOPr-directed pharmatherapeutic opportunities.
(a) Operational stages of the addiction-cycle to cocaine, heroin or illicitly used prescription opioids. Individual trajectory (e.g., severity of escalation, withdrawal, or risk of relapse) is thought to depend on major interacting factors: extent of drug exposure, concomitant stresses, co-morbid psychiatric / psychological status and genetic predisposition (e.g., in OPRK1/PDYN or OPRM1 genes) [16, 27, 41, 57, 66, 76, 98–100]. Each of these factors may be hypothesized to have particular impact at a specific operational stage. For example, a particular SNP may exacerbate either acquisition/escalation, severity of withdrawal-induced dysphoria, or probability of relapse. (b) Proposed pharmacotherapeutic approaches for addictions and neuropsychiatric co-morbidity (panel B), based on appropriate modulation of KOPr/dynorphin tone with selective antagonists or partial agonists. Selective KOPr antagonists (including recently reported compounds with durations of action that are within the range of most therapeutically used compounds [90]) may reduce relapse probability in the early stages of withdrawal/abstinence, by decreasing anhedonia, dysphoria, stress responsivity or comorbid psychiatric signs that may be secondary to upregulated KOPr/dynorphin tone [14, 15, 46, 50, 51, 90]. It is hypothesized that selective KOPr partial agonists (not currently available, due to lack of KOPr>MOPr selectivity in known ligands) [93, 95, 101] may be beneficial in promoting more prolonged abstinence, as well as decreasing the severity of relapse episodes. More specifically, a selective KOPr partial agonist can be hypothesized to provide a degree of homeostatic tone in the KOPr system, via blocking dynorphin-induced hyper-activation in the system (a factor in relapse; see panel (a)), as well as limiting excessive dopamine surges due to relapse-related exposure to cocaine or heroin/prescription opioids.