Fig. 3.
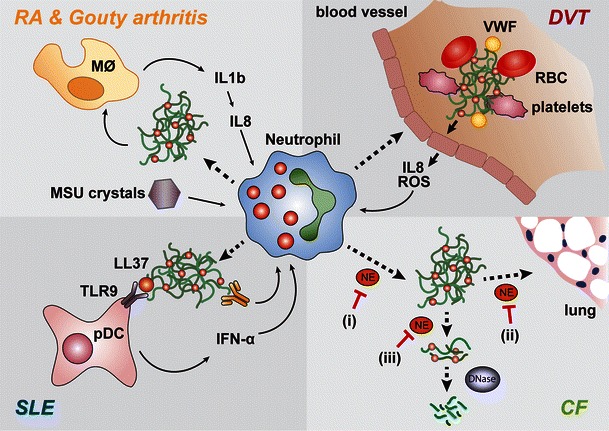
NETs are implicated in the onset of inflammatory and autoimmune diseases. (clockwise) Gouty arthritis: deposition of MSU needles in the SF leads to release of IL-1β by monocytes and induction of IL-8, with subsequent neutrophil recruitment. MSU needles induce release of NETs that stimulate a feedback loop of IL-1β production by monocytes. Deep vein thrombosis: fibrin and von Willebrand factor (vWF) promote blood clotting and deposition of thrombi in the blood vessels. Activated endothelial cells release IL-8 and ROS, thereby recruiting neutrophils and triggering NET formation. NETs act as scaffolds for thrombi in the circulation by interacting with coagulation factors, platelets, and red blood cells (RBC). Systemic lupus erythematosus (SLE): a subset of low-density granulocytes has been shown to spontaneously release NETs in SLE patients. The NET component LL-37 enhances the ability of naked DNA to activate plasmacytoid dendritic cells (pDC) via toll-like receptor 9 (TLR9). pDCs subsequently secrete IFN-α that primes neutrophils to recognize autoimmune complexes of antinuclear antibodies (ANA) and DNA and release NETs. This feedback loop further activates pDCs and may contribute to SLE progression. Cystic fibrosis (CF): NETs form into the sputum in an NE-dependent manner. i Inhibiting NE in intact neutrophils would prevent NET release, but NE is also important in decondensing chromatin extracellularly, which enhances sputum solubilization by therapeutic DNases. ii NE inhibition extracellular would prevent tissue damage iii but would also interfere with sputum solubilization
