Abstract
Membership of indigenous local community groups was protective against HIV for women, but not for men, in eastern Zimbabwe during the period of greatest risk reduction (1999–2004). We use four rounds of data from a population cohort to investigate: (1) the effects of membership of multiple community groups during this period; (2) the effects of group membership in the following five years; and (3) the effects of characteristics of groups hypothesised to determine their effect on HIV risk. HIV incidence from 1998 to 2003 was 1.18% (95% CI: 0.78–1.79%), 0.48% (0.20–1.16%) and 1.13% (0.57–2.27%), in women participating in one, two and three or more community groups at baseline versus 2.19% (1.75–2.75%) in other women. In 2003–2005, 36.5% (versus 43% in 1998–2000) of women were members of community groups, 50% and 56% of which discussed HIV prevention and met with other groups, respectively; the corresponding figures for men were 24% (versus 28% in 1998–2000), 51% and 58%. From 2003 to 2008, prior membership of community groups was no longer protective against HIV for women (1.13% versus 1.29%, aIRR = 1.25;p = 0.23). However, membership of groups that provided social spaces for dialogue about HIV prevention (0.62% versus 1.01%, aIRR = 0.54; p = 0.28) and groups that interacted with other groups (0.65% versus 1.01%, aIRR = 0.51; p = 0.19) showed non-significant protective effects. For women, membership of a group with external sponsorship showed a non-significant increase in HIV risk compared to membership of unsponsored groups (adjusted odds ratio = 1.63, p = 0.48). Between 2003 and 2008, membership of community groups showed a non-significant tendency towards higher HIV risk for men (1.47% versus 0.94%, p = 0.23). Community responses contributed to HIV decline in eastern Zimbabwe. Sensitive engagement and support for local groups (including non-AIDS groups) to encourage dialogue on positive local responses to HIV and to challenge harmful social norms and incorrect information could enhance HIV prevention.
Keywords: community response, social capital, community groups, HIV decline, Zimbabwe
Introduction
Zimbabwe has experienced not only one of the biggest HIV epidemics globally but also one of the largest most sustained declines in HIV prevalence (Zimbabwe National AIDS Council, 2011). HIV prevalence peaked around 1997 at 26.5% (plausibility bounds: 25–27.8%) before falling steadily to 14.3% (13.4–15.3%) in 2009 (Zimbabwe Ministry of Health and Child Welfare, 2010). Declines in infection rates nationally were caused, largely, by reductions in sexual risk behaviour, particularly in concurrent and other multiple sexual partnerships, mostly between 1999 and 2004 (Gregson et al., 2010; Hallett, Gregson, Mugurungi, Gonese, & Garnett, 2009). These changes, in turn, were driven by first-hand experience of AIDS illness and death amongst close friends and relatives, supported by scaled-up community-based HIV prevention programmes (Halperin et al., 2011).
Qualitative studies suggest that interpersonal communication could have played a key role in mediating the effects of these factors on behaviour (Muchini et al., 2010), a finding supported by results from an early analysis of data from our prospective cohort survey in Manicaland in eastern Zimbabwe. This initial analysis showed evidence for a causal link between the community response to the HIV epidemic, in the form of participation in local community groups (Putnam, 2000), and reductions in the incidence of HIV infection and associated risk behaviour in women (but not men) from 1998 to 2003, the period of reduction in sexual risk behaviour (Gregson et al., 2011).
Campbell and colleagues have hypothesised that such effects (including the disparate effects for women and men) could result from the role that participation in community groups plays in determining the nature and effectiveness of spontaneous and externally initiated responses to HIV prevention (Campbell et al., 2013). Potential mechanisms through which these groups influence HIV prevention include providing: (1) a forum for exchange of information; (2) opportunities to share first-hand experiences of being infected or affected by AIDS; (3) social spaces for critical dialogue about HIV/AIDS; (4) a sense of ownership of the response to HIV/AIDS – i.e., acknowledgement that community members have a role to play; not just outsiders in government and NGOs; (5) a sense of AIDS-related agency – confidence in individual and group power to make a difference; (6) a sense of solidarity (versus stigma and discrimination) with HIV-affected others; (7) opportunities to formulate action plans that take account of local culture and socio-economic constraints; and (8) opportunities for links with outside agencies (private, public and NGO sectors) with power to assist in effective responses to AIDS.
These positive psychosocial characteristics are associated with Nhamo, Campbell, and Gregson's (2010, p. 1662) conceptualisation of the “HIV-competent community”, defined as a group of people who work together to respond effectively to HIV/AIDS, through collectively renegotiating health-damaging social norms in ways that facilitate HIV prevention, care of the sick, service access and treatment adherence. Nhamo et al.'s work resonates with three influential areas of community health psychology. The first is Freire's (1973) interest in processes through which marginalised social groupings are most likely to develop critical understandings of the obstacles to their health and well-being as the first step in a reflection-action cycle in which they collectively decide to change previously health-damaging attitudes and behaviours (Rifkin & Pridmore, 2001). The second emphasises the impacts of what are varyingly called perceived self-efficacy (the extent to which one believes one can control one's behaviour, and face life challenges competently) (Bandura, 1990) and psychological empowerment (Wallerstein, 1992) on health-enhancing behaviour change, with membership of supportive groups potentially playing a key role in building the confidence of group members (Berkman & Kawachi, 2000). The third is Szreter and Woolcock's (2004) distinction between inward-looking “bonding” and outward-looking “bridging” social capital, which resonates with Nhamo et al.'s emphasis on solidarity and partnerships and the potentially positive impacts of both forms of social capital on health. Here social capital refers to community networks and norms associated with potentially health-enhancing social cohesion, with bonding social capital referring to networks and norms within a community, and bridging social capital referring to alliances between a community and supportive external partners.
Against this background, the present study has three aims. First, to elaborate on the initial findings for the period 1998–2003 by investigating whether membership of multiple community groups afforded people additional protection against HIV infection beyond that provided by single group membership. Second, to investigate whether group participation had protective effects over the following five years, as HIV prevalence continued to fall. Finally, to test whether the characteristics and internal processes of groups hypothesised to determine their effect on HIV risk behaviour showed the expected effects.
Data and methods
Manicaland HIV/STD Prevention Project
The Manicaland Project has tracked trends in HIV prevalence and incidence, AIDS mortality, sexual behaviour, community group participation and exposure to HIV/AIDS interventions in a representative open cohort of 10,000 adults in 12 locations (including small towns, tea, coffee and forestry estates, roadside settlements and subsistence farming areas) since 1998 (Gregson et al., 2006).
Zimbabwe's eastern province of Manicaland borders on Mozambique and is populated mainly by Shona people (Zimbabwe's largest ethnic group). Subsistence agriculture, based primarily on maize, generally is viable, a variety of other cash crops and vegetables are grown, and most families keep some cattle, goats and chickens. In addition, there are several tea and forestry estates run by parastatal and commercial companies. HIV prevalence was high but fell from 23% between 1998 and 2000 to 17% between 2006 and 2008, largely due to reductions in sexual risk behaviour (Gregson et al., 2006). Anti-retroviral treatment services were introduced first in the early-2000s, but, because of the national economic crisis, only became widely available towards the end of the decade.
Currently, four rounds of survey data are available covering a 10-year period from 1998 to 2008 – round 1: 1998–2000, round 2: 2001–2003, round 3: 2003–2005 and round 4: 2006–2008. Women aged 15–44 years and men aged 17–54 years were eligible for the first two rounds; from round 3, the eligible age range for both sexes was extended to 15–54 years. In each round, data were collected on socio-demographic characteristics, community group membership, self-efficacy, sexual behaviour and HIV infection status (Gregson et al., 2006, 2011).
Statistical analysis
Prospective data from the Manicaland cohort and logistic and Poisson regression models adjusted for possible confounding factors (age, location, education, employment, religion, marital status and poverty) were used to identify possible causal relationships between community participation (measured prior to and during the period of observation) and HIV risk. The main analyses were conducted for two periods – 1998–2003 (rounds 1 to 2) and 2003–2008 (rounds 3 to 4).
Community participation was defined in relation to membership of community groups including women's groups (sewing and other income-generating activities), cooperatives, farmers’ groups, rotating credit societies (savings clubs for income-generating projects), burial societies (community insurance schemes for funeral expenses), youth groups, sports clubs, AIDS groups and political parties. In the initial analysis of HIV avoidance outcomes (i.e., HIV incidence and adoption of lower-risk sexual behaviour), for consistency with previous reports (Gregson et al., 2011), individuals were taken to be participating in community groups if they were members of at least one non-church group they regarded as functioning effectively at the start of the observation period (i.e., round 1 or 3). However, in view of the short periods of group membership found particularly for men (Gregson et al., 2011), in the subsequent analyses, individuals were taken to be participating in community groups if they reported being in at least one group they regarded as functioning effectively at the start of the period of analysis and were still a member of such a group at the end of the period. Respondents were taken to have adopted safer behaviour if they had been sexually active at baseline and had reduced their number of new sexual partners or had no new partners in the last year. Self-efficacy was defined as a dichotomous variable based on responses to the question: “Do you think there are things you can do which will prevent you from becoming infected with HIV in the future?”
Analysis of the possible mediating factors between group membership and HIV-related outcomes of group characteristics was guided by Nhamo et al.'s theoretical framework on HIV competent communities as outlined above (Nhamo et al., 2010) and the operational framework and typology for analysing community responses to HIV/AIDS proposed by Rodriguez-Garcia et al. (2011).
Results
Community group membership
Participation in community groups was fairly high in 1998–2000 with 43% (N = 5149) of all women interviewed at baseline and 29% (N = 4330) of men reporting membership of at least one effective community group (Gregson et al., 2011). Burial societies (22%), rotating credit societies (18%) and women's groups (10%) were the most common forms of groups reported by women. Sports clubs (12%) were the most popular type of group for men. In the following rounds, participation fell initially (to 33% (N = 4125) for women and 21% (N = 3156) for men in 2001–2003) before recovering gradually for women (36.5% (N = 8357) in 2003–2005; 40% (N = 6215) in 2006–2008) and stabilising for men (24% (N = 5917) in 2003–2005; 21% (N = 4385) in 2006–2008); trends that reflect instability in the underlying national socio-economic and political environment.
Female community group membership was consistently highest in more rural areas (e.g., 49% (N = 1968) in villages versus 32% (N = 763) in towns in 1998–2000) whilst male participation rates were highest in the tea estates (38% (N = 804) versus 28% (N = 1241) in villages). Amongst women, in rounds 1 and 3 (baseline periods for prospective analyses), greater participation was associated with older age, marriage, secondary school education, unemployment in the formal sector and Christian religion. Similar patterns were observed amongst men except that, in round 1, men in employment were more likely than those out of work to be participating in group activities. There was no clear association between poverty and group membership for either sex.
Women who reported higher risk behaviour were less likely than other women to be members of groups at rounds 1 and 3, although there were relatively few such women and the differences were not statistically significant – e.g., at round 3, 22% (N = 22) of women who reported multiple new sexual partners in the last year were members of community groups compared to 45% (N = 1381) of women who reported one or no new partner in the last year (age-adjusted odds ratio, aOR = 0.43, p = 0.14). A similar trend was found for men – at round 3, 11% (N = 89) of men with more than one new partner in the last year participated in groups compared to 16% (N = 811) with one or no new partner (aOR = 0.76, p = 0.45). However, men who visited beer halls in the last month – a practice associated with greater sexual risk behaviour in the past (Lewis et al., 2005) – were more likely than other men to be group members (16% versus 9%, aOR = 1.47, p = 0.043).
Effects of multiple group membership, 1998–2003
Of the women who were members of at least one community group at round 1, 29% were members of two groups, 11% were in three groups and 9% in four or more groups (Figure 1). HIV incidence between rounds 1 and 2 was 1.18% (95% CI: 0.78–1.79%), 0.48% (0.20–1.16%) and 1.13% (0.57–2.27%), respectively, in women participating in one, two and three or more groups at baseline compared to 2.19% (1.75–2.75%) in women who were not participating in groups. The proportions of women reporting adopting safer behaviour between rounds 1 and 2 were 94.2% (92.1–96.2%), 98.1% (96.5–99.6%) and 98.3% (96.6–100%) for those participating in one, two and three or more community groups at baseline compared to 90.1% (88.1–92.1%) for women not participating in community groups.
Figure 1.
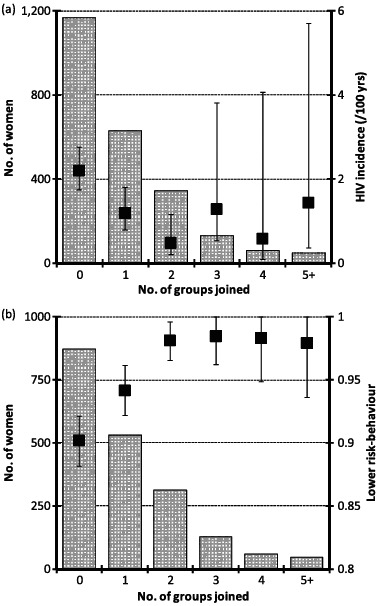
Dose effects of multiple community group membership on (a) HIV incidence and (b) reducing or maintaining low-risk behaviour, for women, 1998–2003. The scale bars in the histogram show the numbers of women by number of groups joined for each outcome. The square boxes with whiskers show the estimates and 95% confidence intervals, respectively, for HIV incidence (graph (a)) and adoption of lower risk-behaviour (graph (b)).
Twenty per cent of the men participating in community groups at round 1 were members of two groups and 6% were members of three or more groups. However, there was no evidence for differences in HIV incidence or adoption of safer sexual behaviour by number of groups joined amongst men.
Temporal effects of community group membership on HIV prevention
As reported previously (Gregson et al., 2011), women who were members of groups at round 1 (1998–2000) were less likely to acquire HIV in the following three years than other women, after adjusting for observed confounding factors, and more likely to report adopting safer sexual behaviour (Table 1). However, from 2003 to 2008, prior membership of community groups (i.e., at round 3) was no longer protective against HIV (1.13% versus 1.29%; aIRR = 1.25, p = 0.23) and was associated with only a non-significant increase in adopting safer behaviour compared to that seen in women who were not members of groups (90.4% versus 84.7%, aOR = 1.25, p = 0.07). A greater proportion of women in groups than women not in groups at round 3 believed they could avoid becoming infected with HIV (self-efficacy) three years later when interviewed in round 4.
Table 1.
Comparison of effects of community group membershipa: 2003–2008 versus 1998–2003.
| 2003–2008 |
1998–2003 |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Members |
Non-members |
Test for difference |
Members |
Non-members |
Test for difference |
|||||||
| Outcome | % | Nc | % | Nc | aORb (95% CI) | p | % | Nc | % | Nc | aORb (95% CI) | p |
| Females | ||||||||||||
| HIV incidence (aIRR) | 1.13 | 4682 | 1.29 | 4510 | 1.25 (0.87–1.80) | 0.23 | 0.97 | 3607 | 2.19 | 3424 | 0.64 (0.43–0.94) | 0.024 |
| Adoption of low-risk behaviour | 90.37 | 1671 | 84.69 | 1398 | 1.25 (0.98–1.59) | 0.07 | 96.18 | 1073 | 90.13 | 871 | 1.85 (1.21–2.83) | 0.005 |
| Self-efficacy | 82.82 | 1653 | 79.95 | 1651 | 1.39 (1.11–1.73) | 0.003 | 82.10 | 1570 | 82.51 | 1555 | 1.06 (0.88–1.28) | 0.55 |
| Males | ||||||||||||
| HIV incidence (AiRR) | 1.47 | 1228 | 0.94 | 3830 | 1.39 (0.82–2.35) | 0.23 | 2.60 | 1539 | 1.71 | 3388 | 1.46 (0.95–2.24) | 0.08 |
| Adoption of low-risk behaviour | 80.68 | 414 | 76.10 | 975 | 1.04(0.77–1.42) | 0.79 | 78.30 | 434 | 72.90 | 896 | 1.36 (1.05–1.76) | 0.020 |
| Self-efficacy | 94.67 | 450 | 93.29 | 1341 | 1.22(0.76–1.96) | 0.41 | 96.81 | 658 | 96.83 | 1420 | 0.92 (0.57–1.48) | 0.74 |
Notes: a For consistency with previous reports (Gregson et al. PDR 2011), individuals are taken to be participating in community groups if they were members of at least group they considered be functioning effectively at the start of the period of observation.
Odds ratio adjusted for age, location, education, employment, religion, marital status and poverty.
Person-years of exposure for HIV incidence.
Men participating in community groups at baseline tended to have a higher risk of having become infected at follow-up than men not in groups despite a higher proportion reporting adopting safer behaviour (Gregson et al., 2011). This anomaly could be due to differences in other behaviours (e.g., selection of fewer but more risky sexual partners or less consistent condom use with casual partners) or to differences in reporting bias. From 2003 to 2008, prior membership of community groups (at round 3) was again non-significantly associated with risk of having acquired HIV for men at follow-up (round 4). However, there were no differences between men in groups and other men in reported adoption of safer behaviour or in self-efficacy.
Characteristics of community groups associated with HIV risk
Figure 2 shows the proportions of respondents who were members of community groups at both round 3 and round 4 who reported, at round 3, that their groups had features hypothesised to influence the risk of HIV infection. Approximately half of both sexes said the groups they spent most time in discussed HIV prevention formally or informally (i.e., provided social spaces for dialogue about HIV prevention). Slightly more – with similar proportions for women and men – reported that their groups assisted or met with other groups (i.e., provided bridging social capital). A significantly greater proportion of women than men reported that their group had single sex membership (50.1% versus 33.6%, aOR = 2.10, p = 0.004), with a number of the men-only groups being sports clubs. One-third of both women and men reported that their groups received sponsorship from external sources. Churches (36%) and NGOs (17%) were the leading sources of support reported by women. Political parties (32%), churches (18%), NGOs (13%) and employers (11%) were the principal sources reported by men.
Figure 2.
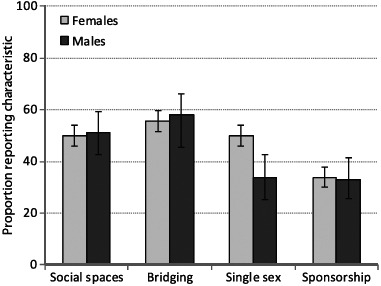
Frequencies of different group characteristics reported by members of community groups, 2003–2005. Note: Social spaces – group discusses HIV prevention; bridging – group assists or meets other groups; single sex – single sex versus mixed sex group; sponsorship – funding from an external source (e.g., NGO, employer or a government source).
Table 2 shows the effects of prior and continued participation in community groups on HIV incidence and associated risk behaviour from 2003 to 2008 in the right-hand columns. Results for each sex are broadly similar to those for the effects of prior participation alone (Table 1). For women and men who were group members at the beginning and end of the period, the effects of different group characteristics are also shown in Table 2. Fewer women in groups providing social spaces for dialogue on HIV prevention than women in groups overall acquired HIV between 2003 and 2008, but the difference was not statistically significant (HIV incidence: 0.62% versus 1.01%, aIRR = 0.54, p = 0.28). No difference was found in adoption of safer sexual behaviour between women in groups with and without dialogue on HIV prevention but women in groups that discussed HIV prevention were more likely to believe they could avoid becoming infected. The results in Table 3 show that many different types of groups provide social spaces for dialogue about HIV prevention with women in AIDS groups being the most likely to report such discussions and women in burial societies being the least likely to report discussions.
Table 2.
Characteristics of community groups associated with HIV risk, 2003–2008.
| Effects of group characteristics amongst group members |
Membersa versus non-members |
|||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Social spaces (discuss HIV prevention) |
Bridging (assist or meet with other groups) |
Single sex versus mixed sex membership |
Sponsorship |
Members |
Non-members |
Test for difference |
||||||||||||||||
| Outcome | aORb | p | % | Nc | aORb | p | % | Nc | aORb | p | % | Nc | aORb | p | % | Nc | % | Nc | % | Nc | aORb | P |
| Females | ||||||||||||||||||||||
| HIV incidence (aIRR) | 0.54 | 0.28 | 0.62 | 813 | 0.51 | 0.19 | 0.65 | 922 | 1.52 | 0.50 | 1.35 | 816 | 1.63 | 0.48 | 1.07 | 560 | 1.01 | 1683 | 1.25 | 7509 | 0.96 | 0.89 |
| Adoption of low-risk behaviour | 0.96 | 0.89 | 90.88 | 307 | 2.77 | 0.001 | 92.98 | 342 | 0.87 | 0.64 | 88.82 | 304 | 0.64 | 0.21 | 88.52 | 209 | 89.87 | 622 | 84.04 | 777 | 1.22 | 0.27 |
| Self-efficacy | 1.79 | 0.013 | 86.84 | 304 | 0.89 | 0.66 | 83.78 | 333 | 1.43 | 0.17 | 84.83 | 290 | 1.11 | 0.72 | 84.39 | 205 | 82.98 | 605 | 79.55 | 978 | 1.52 | 0.022 |
| Males | ||||||||||||||||||||||
| HIV incidence (aIRR) | 0.59 | 0.51 | 1.99 | 201 | 1.53 | 0.66 | 2.64 | 228 | 0.89 | 0.91 | 2.55 | 118 | 1.85 | 0.44 | 3.14 | 127 | 2.03 | 395 | 0.86 | 3109 | 1.88 | 0.12 |
| Adoption of low-risk behaviour | 0.69 | 0.41 | 68.57 | 70 | 0.46 | 0.22 | 64.47 | 76 | 1.03 | 0.97 | 64.71 | 34 | 0.78 | 0.73 | 65.22 | 46 | 73.53 | 136 | 76.70 | 764 | 0.68 | 0.11 |
| Self-efficacy | 1.17 | 0.90 | 94.44 | 72 | 0.56 | 0.57 | 92.68 | 82 | 6.31 | 0.32 | 92.68 | 41 | 2.18 | 0.54 | 95.74 | 47 | 93.66 | 142 | 92.82 | 1086 | 0.94 | 0.86 |
Notes: a Individuals taken to be participating groups if they were members at baseline and still at follow-up; reference group comprises individuals who were neither members at baseline nor at follow.
Odds ratio adjusted for age, location, education, employment, religion, marital status, poverty and (for effects of group characteristics) other group characteristics.
Person-years of exposure for HIV incidence.
Table 3.
Types of community groups that provide social spaces for dialogue on HIV prevention, 2003–2005.
| Females | Males | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Members reporting social spaces |
Test for difference |
Members reporting social spaces |
Test for difference |
|||||||
| Type of community group | n | N | (%) | aORa (95% CI) | p | n | N | (%) | aORa (95% CI) | p |
| Women's group | 26 | 45 | (57.8) | 1.32(0.69–2.53) | 0.40 | – | – | – | – | – |
| Co-operative | 20 | 32 | (62.5) | 1.02(0.50–2.07) | 0.96 | 1 | 2 | (50.0) | – | – |
| Farmers group | 32 | 72 | (44.4) | 0.79 (0.47–1.33) | 0.37 | 13 | 22 | (59.1) | 1.46 (0.52–4.09) | 0.47 |
| Burial society | 103 | 269 | (38.3) | 0.49 (0.36–0.69) | <0.001 | 22 | 43 | (51.2) | 0.81 (0.34–1.93) | 0.63 |
| Rotating credit society | 28 | 64 | (43.8) | 0.73 (0.42–1.26) | 0.26 | 3 | 8 | (37.5) | – | – |
| Youth group | 8 | 10 | (80.0) | 3.78 (0.67–21.20) | 0.13 | 5 | 12 | (41.7) | 0.59 (0.15–2.28) | 0.45 |
| Sports club | 9 | 16 | (56.3) | 1.21 (0.40–3.70) | 0.74 | 13 | 31 | (41.9) | 0.47 (0.15–1.43) | 0.18 |
| Political party | 15 | 33 | (45.5) | 0.88 (0.42–1.84) | 0.74 | 14 | 23 | (60.9) | 2.36 (0.83–6.72) | 0.11 |
| AIDS group | 74 | 80 | (92.5) | 13.40 (5.66–31.72) | <0.001 | 2 | 2 | (100.0) | – | – |
| Any group | 316 | 632 | (50.0) | – | – | 74 | 145 | (51.0) | – | – |
Notes: Results based on individuals reporting membership of at least one community group at baseline and again, after 3 years, at follow-up.
Odds ratio for reporting dialogue on HIV prevention for group members compared with reports from members of all other types of groups, adjusted for age, location, education, employment, religion, marital status and poverty.
Women in groups who met other groups had non-statistically significant lower HIV incidence (0.65% versus 1.01%, aIRR = 0.51, p = 0.19) and were more likely than women in other groups to report adoption of safer sexual behaviour (93.0% versus 84.0%, aOR = 2.77, p = 0.001). Women in groups with external sponsorship had greater HIV incidence and were less likely to report adoption of safer behaviour than women in other groups, but these differences were not statistically significant (Table 2).
There were fewer men than women in community groups in the study and no clear effects of group characteristics on HIV risk emerged in the analysis for men (Table 2).
Discussion
The community response to HIV, in the form of widespread female participation in community groups, appears to have played an important part in Zimbabwe's HIV decline. From the late 1990s through the early-2000s – the period of most rapid risk reduction (Hallett et al., 2009) – women who were community group members were quicker to adopt safer sexual behaviour and experienced a lower rate of new infections than other women. In this article, we provide evidence for a “dose effect,” with women who participated in multiple groups during this period being even more likely to adopt safer sexual behaviour than those who participated in a single group. This finding may reflect the effects of multiple avenues of information or greater social exposure.
By the early-2000s (2003–2008), as HIV prevalence continued to drop, the rate of new infections in women who were not members of community groups declined, with the early overall advantage gained by women participating in groups no longer apparent. However, in this period – for which more detailed data on group characteristics were available – we were able to investigate some of the mechanisms hypothesised to influence the association between group membership and reduction in HIV risk. Consistent with Nhamo et al.'s (2010) conceptualisation of “HIV Competent Communities”, more than half of the female community group members interviewed between 2003 and 2005 reported that they still discussed HIV prevention in their groups. Furthermore, we found sizeable (although non-statistically significant) reductions in the incidence of HIV infection amongst these women relative to infection rates in women who were members of groups that did not discuss HIV prevention. Women who participated in community groups expressed greater confidence that they could avoid becoming infected with HIV (Wallerstein, 1992) and the rate of new infections also was lower in women whose groups inter-acted with other groups. One-third of the women who were members of groups were in groups that received sponsorship but, after controlling for other factors, these women tended to have higher infection rates than other women in groups. Thus, external sponsorship sometimes may undermine the positive effects of membership of spontaneously formed indigenous groups.
Fewer men than women participate in community groups (Gregson et al., 2011). Amongst men, HIV incidence rates fell between 1998–2003 and 2003–2008 both for community group members and for non-members. As in the earlier period, the rate of new infections between 2003 and 2008 was non-significantly higher in men who reported participating in community groups than in those who did not join these groups. As for women, the groups that men participated in provided social spaces for dialogue about HIV. However, for men, there was no clear evidence that groups that discussed HIV prevention were more effective in helping them to avoid becoming infected. Similarly, HIV rates remained high in male group members irrespective of whether the group they were in interacted with other groups or received external sponsorship. This is consistent with findings that, in certain settings (e.g., male-dominated groups such as sports clubs and political parties), group dialogue may reinforce health-damaging macho masculinities associated with alcohol consumption and lack of sexual caution (Campbell et al., 2013; Gregson et al., 2011).
The strengths of this study include the use of longitudinal prospective data, making it possible to examine changes in community participation and their effects over time, the large overall general population sample and inclusion of HIV incidence as a hard biomedical outcome. The main quantitative findings were obtained from prospective analyses of longitudinal cohort data in which the effects on changes in outcomes, over a given study period, of prior exposure to community group activities were measured. Therefore, the observed statistical associations are more likely to be causal and to reflect effects of community group participation on the study outcomes rather than vice versa than was the case in earlier cross-sectional studies (Campbell, Williams, & Gilgen, 2002; Gregson, Terceira, Mushati, Nyamukapa, & Campbell, 2004; Pronyk et al., 2008). However, participation in community groups is an endogenous variable which is affected by self-selection. Whilst we sought to control for this by adjusting for differences in socio-demographic characteristics and sexual risk behaviour at baseline in each analysis, there may have been other unobserved characteristics that predisposed individuals with greater community engagement to reduce risk behaviour. Therefore, the results cannot be taken as fully establishing a causal link between participation in community groups and the outcomes examined in the analyses. Other limitations include the restriction to periods prior to the widespread availability of antiretroviral therapy in Zimbabwe and to primarily rural areas in the east of the country. This said, in more recent qualitative investigations in a district in Matabeleland province, we found similar patterns of community response to HIV despite substantial differences in culture, climate and socio-economic activity (Skovdal, Magutshwa-Zitha, Campbell, Nyamukapa, & Gregson, 2011).
The findings of this research are significant from a policy perspective. In 1999, the Zimbabwe National AIDS Council (NAC) was established to drive forward a multi-sectoral response to the epidemic (Muchini et al., 2010). A National HIV/AIDS Policy was established and, the next year, a National AIDS Trust Fund set up, financed through an “AIDS levy” on income tax, initially primarily to support community initiatives through NAC structures at provincial, district, ward and village levels. The scale-up of HIV/AIDS programmatic activity between 1999 and 2004 that occurred, in part, as a result of these initiatives, is believed to have contributed to reductions in risk behaviour at this time (Halperin et al., 2011). The strategy of focusing support on activities implemented by communities at village level may have enhanced the role of local community groups in promoting behaviour change during this period. In the current Zimbabwe National AIDS Strategic Plan II (Zimbabwe National AIDS Council, 2011), activities to strengthen community-based support systems are identified as a key priority. Our findings suggest this could be done, in part, by working with existing community groups (including non-AIDS groups) to encourage dialogue that allows members to conceive of positive local responses to HIV and challenge harmful social norms (including stigma and negative aspects of masculinity) and incorrect information. The HIV Competent Community concept, the theoretical basis for this analysis, could be used to improve programmes by encouraging active and meaningful participation of communities as genuine partners in HIV/AIDS management efforts, so as to build upon and enhance existing community structures, capacities and initiatives, and to avoid unintended consequences.
Acknowledgement
The authors are grateful to the Manicaland Study team and the community participants in Manicaland, Zimbabwe, for making the data available for the study, and to the World Bank and DfID for funding for the research on community response to the HIV epidemic in Zimbabwe.
References
- Bandura A. Perceived self-efficacy in the exercise of control over AIDS infection. Evaluation and Programme Planning. 1990;13(1):9–17. [Google Scholar]
- Berkman L., Kawachi I., editors. Social epidemiology. New York, NY: Oxford University Press; 2000. [Google Scholar]
- Campbell C. Williams B., Gilgen D. Is social capital a useful conceptual tool for exploring community level influences in HIV infection? An exploratory case study from South Africa. AIDS Care. 2002;14:41–54. doi: 10.1080/09540120220097928. [DOI] [PubMed] [Google Scholar]
- Campbell C. Scott K. Nhamo M. Nyamukapa C. Madanhire C. Skovdal M., Gregson S. Social capital and HIV Competent Communities: The role of community groups in managing HIV/AIDS in rural Zimbabwe. AIDS Care. 2013;25(Suppl. 1):S114–S122. doi: 10.1080/09540121.2012.748170. doi:10.1080/09540121.2012.748170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freire P. Education for critical consciousness. New York, NY: Continuum; 1973. [Google Scholar]
- Gregson S. Garnett G. P. Nyamukapa C. A. Hallett T. B. Lewis J. J. C. Mason P. R. Anderson R. M. HIV decline associated with behaviour change in eastern Zimbabwe. Science. 2006;311:664–666. doi: 10.1126/science.1121054. [DOI] [PubMed] [Google Scholar]
- Gregson S. Gonese E. Hallett T. B. Taruberekera N. Hargrove J. W. Corbett E. L. Mugurungi O. HIV decline due to reductions in risky sex in Zimbabwe? Evidence from a comprehensive epidemiological review. International Journal of Epidemiology. 2010;39(5):1311–1323. doi: 10.1093/ije/dyq055. doi:10.1093/ije/dyq055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gregson S. Mushati P. Grusin H. Nhamo M. Schumacher C. Skovdal M. Campbell C. Social capital and reduced female vulnerability to HIV infection in rural Zimbabwe. Population and Development Review. 2011;37(2):333–359. doi: 10.1111/j.1728-4457.2011.00413.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gregson S. Terceira N. Mushati P. Nyamukapa C. A., Campbell C. Community group participation: Can it help young women to avoid HIV? An exploratory study of social capital and school education in rural Zimbabwe. Social Science and Medicine. 2004;58:2119–2132. doi: 10.1016/j.socscimed.2003.09.001. [DOI] [PubMed] [Google Scholar]
- Hallett T. B. Gregson S. Mugurungi O. Gonese E., Garnett G. P. Is there evidence for behaviour change affecting the course of the HIV epidemic in Zimbabwe? A new mathematical modelling approach. Epidemics. 2009;1(2):108–117. doi: 10.1016/j.epidem.2009.03.001. [DOI] [PubMed] [Google Scholar]
- Halperin D. T. Mugurungi O. Hallett T. B. Muchini B. Campbell B. Magure T., Gregson S. A surprising prevention success: Why did the HIV epidemic decline in Zimbabwe? Public Library of Science Medicine. 2011;8(2):e1000414. doi: 10.1371/journal.pmed.1000414. doi:10.1371/journal. pmed.1000414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis J. J. C. Garnett G. P. Mhlanga S. Nyamukapa C. A. Donnelly C. A., Gregson S. Beer halls as a focus for HIV prevention activities in rural Zimbabwe. Sexually Transmitted Diseases. 2005;32(6):364–369. doi: 10.1097/01.olq.0000154506.84492.61. [DOI] [PubMed] [Google Scholar]
- Muchini B. Benedikt C. Gregson S. Gomo E. Mate R. Mugurungi O. Halperin D. T. Local perceptions of the forms, timing and causes of behaviour change in response to the AIDS epidemic in Zimbabwe. AIDS and Behaviour. 2010;15:487–498. doi: 10.1007/s10461-010-9783-z. doi:10.1007/s10461–010–9783-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nhamo M. Campbell C., Gregson S. Contextual determinants of HIV prevention programme outcomes: Obstacles to local-level AIDS competence in rural Zimbabwe. AIDS Care. 2010;22(Suppl. 2):1662–1669. doi: 10.1080/09540121.2010.521544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pronyk P. M. Harpman T. Busza J. Phetia G. Morison L. A. Hargreaves J. R. Porter J. D. H. Can social capital be intentionally generated? A randomised trial from South Africa. Social Science and Medicine. 2008;67:1559–1570. doi: 10.1016/j.socscimed.2008.07.022. [DOI] [PubMed] [Google Scholar]
- Putnam R. D. Bowling alone: The collapse and revival of American community. New York, NY: Simon and Schuster; 2000. [Google Scholar]
- Rifkin S., Pridmore P. Partners in planning: Information, participation and empowerment. London: Macmillan; 2001. [Google Scholar]
- Rodriguez-Garcia R. Bonnel R. N'Jie N. Olivier J. Pascual F. B., Wodon Q. Analyzing community responses to HIV and AIDS: Operational framework and typology. Washington, DC: World Bank; 2011. p. 40. [Google Scholar]
- Skovdal M. Magutshwa-Zitha S. Campbell C. Nyamukapa C. A., Gregson S. Similarities and differences in the community response to HIV and AIDS in Matabeleland South and Manicaland. Washington, DC: World Bank; 2011. p. 37. [Google Scholar]
- Szreter S., Woolcock M. Health by association: Social capital, social theory and the political economy of public health. International Journal of Epidemiology. 2004;33(4):650–667. doi: 10.1093/ije/dyh013. [DOI] [PubMed] [Google Scholar]
- Wallerstein N. Powerlessness, empowerment and health: Implications for health promotion programmes. American Journal of Health Promotion. 1992;6(3):197–205. doi: 10.4278/0890-1171-6.3.197. [DOI] [PubMed] [Google Scholar]
- Zimbabwe Ministry of Health and Child Welfare. Zimbabwe National HIV and AIDS estimates 2009. Harare: Zimbabwe Ministry of Health and Child Welfare; 2010. [Google Scholar]
- Zimbabwe National AIDS Council. Zimbabwe National HIV and AIDS strategic plan 2011–2015 [ZNASP II] Harare: Zimbabwe National AIDS Council; 2011. [Google Scholar]


