Figure 8.
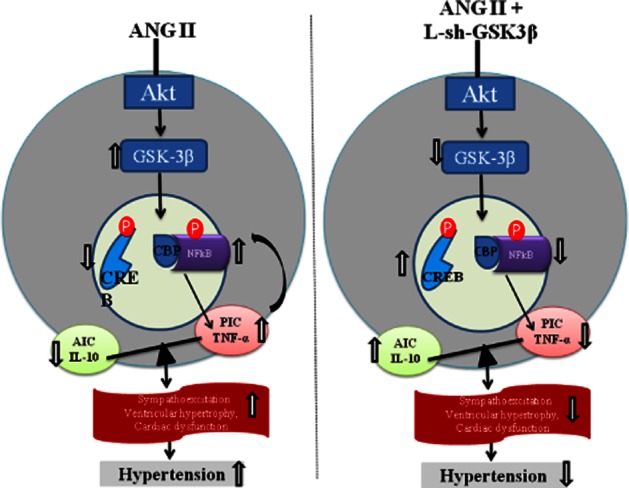
A schematic depicting the proposed pathways (right panel) of AngII-induced dysregulation in inflammatory cytokines in neuronal cells and showing the mechanisms (left panel) by which neuronal cytokines contributes to the pathogenesis of hypertension. It has become clear from the past several years of research that an increased production of PICs in response to overactivated RAS within the cardiovascular regulatory centres of the brain (such as paraventricular nucleus and rostral ventrolateral medulla) causes increased sympathetic outflow leading to increased arterial pressure and cardiac remodelling in experimental models of hypertension. At the cellular level, PICs activate reactive oxygen species which in turn can activate various intracellular signalling pathways, including that of NFκB. Activation of NFκB induces gene transcription of PICs fostering a positive feedback mechanism, and eventually leading to the progression of hypertension. A step further, the results of the present study revealed a novel molecular mechanism that AngII-induced increased phosphorylation of GSK-3β(Tyr-216) and increased p-GSK3β(Tyr-216) to p-GSK-3β(Ser-9) ratio leads to altered activity of downstream transcription factors, NFκB and CREB, in favour of NFκB-mediated gene transcription, thereby, causing an imbalance between PIC and AIC in rat neuronal cells.
