Abstract
A new era in the surgical treatment of adolescent idiopathic scoliosis (AIS) opened with the introduction of pedicle screw instrumentation, which provides 3-column vertebral fixation and allows major deformity correction on the coronal, sagittal, and axial planes. A steep learning curve can be expected for spinal surgeons to become familiar with pedicle screw placement and correction techniques. Potential complications including injury to adjacent neural, vascular, and visceral structures can occur due to screw misplacement or pull-out during correction maneuvers. These major complications are better recognized as pedicle screw techniques become more popular and may result in serious morbidity and mortality. Extensive laboratory and clinical training is mandatory before pedicle screw techniques in scoliosis surgery are put to practice. Wider application, especially in developing countries, is limited by the high cost of implants. Refined correction techniques are currently developed and these utilize a lesser number of pedicle anchors which are strategically positioned to allow optimum deformity correction while reducing the neurological risk, surgical time, and blood loss, as well as instrumentation cost. Such techniques can be particularly attractive at a time when cost has major implications on provision of health care as they can make scoliosis treatment available to a wider population of patients. Pedicle screw techniques are currently considered the gold standard for scoliosis correction due to their documented superior biomechanical properties and ability to produce improved clinical outcomes as reflected by health-related quality-of-life questionnaires. Ongoing research promises further advances with the future of AIS treatment incorporating genetic counseling and possibly fusionless techniques.
Keywords: Adolescent idiopathic scoliosis, pedicle screws, spinal fusion
PEDICLE SCREW INSTRUMENTATION
First introduced by Boucher1 and popularized by Roy-Camille,2 pedicle screws were initially used in traumatic and neoplastic conditions of the spine due to their major advantage of providing 3-column vertebral stabilization. Their use was limited in scoliosis surgery to the lumbar and thoracolumbar spine because of the presence of larger pedicles. Their safety of use in the thoracic spine was considered questionable as the pedicles are small and deformed in the presence of scoliosis, the spinal canal is smaller in size, and the cord is more susceptible to injury compared to the cauda equina.3 The first step toward a wider use of pedicle screws was the introduction of hybrid constructs using thoracic hooks and lumbar screws which achieved significant improvement in scoliosis correction when used for double major curves compared to all-hook constructs.4 Techniques using pedicle screws could produce superior deformity correction in the coronal, axial, and sagittal planes with lesser risk of nonunion, implant failure, and curve recurrence, as well as the ability to perform shorter fusions and preserve spinal mobile segments.
CLINICAL SAFETY
Initial series of hook/screw constructs reported good results in adolescent idiopathic scoliosis (AIS); however, the use of pedicle screws in the thoracic spine took longer to gain wide acceptance due to the difficulty of placement and associated risk of neurological or visceral injury.3,5 A very narrow margin of error (<1 mm translational and <5° rotational) was predicted for pedicle wall violation during thoracic screw placement with high risk of canal intrusion or anterior vertebral body penetration.6 When accurately inserted, pedicle screws should not encroach on neural elements or migrate from the bony canal during correction maneuvers.7 Gertzbein and Robbins8 reported a safe zone of 4 mm (2 mm epidural space and 2 mm subarachnoid space) for pedicle screw passage. Kim et al.9 quoted 2-4 mm of cortical breach as safe encroachment. Previous cadaveric studies showed, however, no space between the pedicle and dural sheath.10 Papin et al.11 reported right foot resting tremor and dysesthesia affecting the legs of a patient who had 2 screws within 4 mm of medial wall breach. Removal of the misplaced screws resulted in resolution of the symptoms. A 2-mm encroachment on the spinal canal, corresponding to the thickness of the blade of laminar hooks, is generally considered safe in the thoracic spine and all efforts should be made to position pedicle screws within this limit.
Despite high rates of screw malposition, there has been a low reported incidence of major neurological and vascular complications requiring revision surgery.8,12 Lateral wall breach is the most common (68%), followed by medial wall (14%) because the latter is 2-3 times thicker and offers more resistance.13,14 The lateral wall, even if breached is buttressed by the rib in the presence of intact costo-transverse ligaments.15 Belmont et al.14 reported 99% of their screws to be fully contained (either ≤ 2 mm of medial cortical breach or an acceptable lateral cortical breach). Many studies have reported safety and effectiveness of pedicle screws since the initial report by Suk et al.16 Their use was found to be safe even in severe thoracic scoliosis above 100°.17,18
PEDICLE MORPHOLOGY
Anatomical studies have documented average pedicle width and length in the normal population;19 however, pedicle characteristics differ between individuals and are significantly affected by the type and severity of deformity. Clear understanding of pedicle morphology is essential for safe screw passage.16,20 Due to frequent variation in normal morphometry, as well as the changes induced by scoliosis, a preoperative computed tomography (CT) scan may be useful in severe deformities to define pedicle anatomy. The pedicles often assume a wind-swept appearance in larger curves when the spine rotates toward the convexity of the scoliosis.15 The concave pedicles are smaller and anteriorly translated with maximum deformation across the apical levels. Medial angulation required for concave screw placement is limited by the space provided during the approach making a lateral breach more frequent and this carries the risk of visceral injuries. On the convex side, the pedicle is larger and posteriorly translated, offering a more vertical trajectory for screw insertion.15 In addition, the neural tube is shifted toward the concavity of the scoliosis with the dura placed adjacent to the medial cortex of the concave pedicles making screw placement on the convex side safer.21 Watanabe et al.22 described four types of thoracic scoliotic pedicles depending upon the width of cancellous channels: Large/adequate channel (type A), small/stenotic but cancellous channel (type B), cortical channel (type C), and slit/absent channels (type D). Convex pedicles are more likely to be type A or B compared to concave pedicles where screw positioning is easier to fail.
BIOMECHANICAL PRINCIPLES AND SCREW PLACEMENT
Pedicle screws have much greater pull-out strength when compared to hooks due to 3-column vertebral fixation. Pull-out strength depends upon the outer diameter of the screw, depth of vertebral penetration, insertion technique, as well as the patient's bone quality. A wider screw diameter increases screw pull-out strength.23 Ideal screw diameter in adults is 80% of the pedicle size.15 In adolescents, a screw up to 115% of the outside pedicle diameter can be inserted without causing pedicle fracture due to plastic deformation.24 Vertebral body penetration of 70% has been found to be optimal and avoids anterior vertebral wall breach and potential vascular or visceral injury.25
Two screw passage trajectories have been described: (a) The straight-forward technique (screw parallel to vertebral end plate), (b) the anatomical technique (screw in line with pedicle axis); the straight-forward technique has at least 39% higher maximal insertional torque than the anatomical technique.26 White et al.27 described the pedicle-rib unit which has higher transverse diameter than the pedicle alone, and can be used for safer insertion of pedicle screws by deliberately breaching the lateral wall (in-and-out technique). This can be used as salvage technique in the presence of type C/D pedicles mostly at the concave apex of severe scoliosis or at the most cephalad levels in young patients. However, this technique allows only vertebral body fixation and therefore, decreases pull-out strength by 25% increasing the risk of concave screw cut-out during correction maneuvers. Under tapping the pedicle by 1 mm usually increases maximal insertional torque by 93%.28 Implant loosening and failure can occur due to low bone mineral density (BMD). Higher resistance to axial and tangential loading was found with pedicle screws, when compared to laminar or pedicle hooks with BMD > 100 mg hydroxyapatite/ml.29
Optimal screw insertion, especially in the thoracic spine depends upon the experience of the surgeon. Even in the presence of a low margin of error, the visual and tactile feedback of the surgeon improves containment of the screws.5 The use of fluoroscopy increases the accuracy of screw insertion, although radiation exposure is high.30,31 Intraoperative CT guidance has been used effectively to reduce screw misplacement. Breach and revision rates of thoracic pedicle screws are significantly lower with the use of a navigation system. However, these systems increase the cost of surgery and are not available at most spinal centers.32 Free-hand techniques relying on anatomical landmarks have been described to minimize radiation exposure.16,20,21
We routinely place all pedicle screws through a free-hand technique with the pedicle entry point from T1 to T5 at the junction of the bisected transverse process and the lateral margin of the facet joint and from T6 to T10 at the junction of the upper to the middle third of the transverse process and the lateral margin of the facet joint. Pedicle screws at T11 and T12 are inserted with the entry point at the base of the superior facet and in the lumbar spine at the junction of the transverse process, pars interarticularis, and the superior facet. The pedicle canal is felt for bony continuity in all directions before screw placement. We confirm adequate screw positioning with anteroposterior and lateral imaging before engagement of the rods and correction maneuvers. In our experience, there is a steep learning curve for insertion of thoracic pedicle screws. Even though we do not routinely check the accuracy of screw placement with CT scans, the primary author has not had any postoperative pedicle screw-related neurological or visceral complications with approximately 10,000 pedicle screws inserted to present. Meticulous and consistent surgical technique, as well as use of intraoperative somatosensory/motor monitoring and imaging has considerably reduced the neurological complication rate.32
SCOLIOSIS CORRECTION WITH PEDICLE SCREWS
Suk et al.16 described scoliosis correction with all-pedicle screw constructs using: (a) Global rod de-rotation, which corrects the deformity in the coronal and sagittal planes (Cotrel-Dubousset maneuver CD), and (b) direct segmental vertebral de-rotation which adds axial plane correction achieving a more physiological spinal contour. The use of quadrilateral frames, vertebral column manipulators, and vertebral co-planar alignment techniques describe correction of rotational deformities by slotted rods or mounts based on the same principles.33
Initial description of such techniques suggested the use of segmental pedicle screws bilaterally across the levels of the fusion for optimum deformity correction [Figure 1]. It is now evident that such high implant density is not necessary to correct scoliosis other than probably for extreme and rigid curves.34 Strategically placed screw anchors gain popularity as these reduce the risk of neurological and visceral complications, surgical time and blood loss, implant density directly related to risk of infection, and implant cost. In our practice, we use segmental screw fixation over one side of the construct in order to achieve deformity correction, while the second rod has a supportive role and is attached to the spine through 2-level screw stabilization at the proximal and distal ends of the instrumentation. In a series of 212 consecutive patients operated by the senior surgeon (AIT), we demonstrated that the use of unilateral segmental pedicle screws over a “corrective rod” with the contralateral “supportive rod” secured to the spine through a 2-level fixation at the proximal and distal ends of the construct can achieve comparable scoliosis correction and patient satisfaction to a bilateral segmental pedicle screw technique which carries a higher neurological risk and significantly increases surgical time, intraoperative blood loss, and instrumentation cost.35 Convex screws are safer to position due to the anatomical considerations of the pedicles, as well as the concave displacement of the neural axis and in our experience, they produce comparable coronal and sagittal deformity correction to concave screws [Figure 2].
Figure 1.
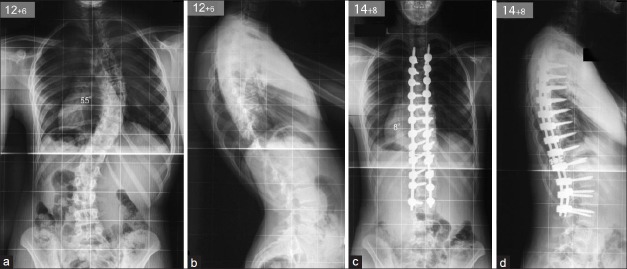
Posteroanterior (a) and lateral (b) radiographs of the spine of a female adolescent patient show a primary right thoracic compensatory left lumbar scoliosis with associated lumbar hyperlordosis. A posterior spinal fusion using bilateral segmental pedicle screw/rod instrumentation and iliac crest bone achieved good deformity correction and a balanced spine in the coronal and sagittal planes (c-d)
Figure 2.
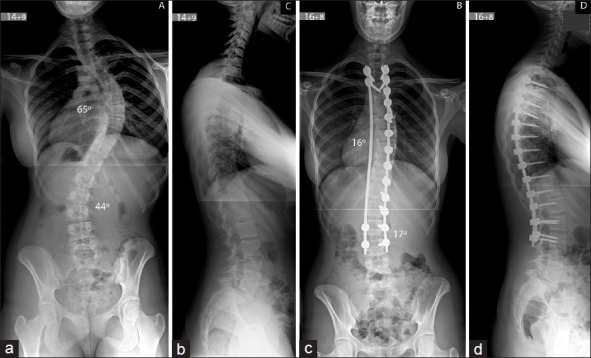
Posteroanterior (a) and lateral (b) radiographs of the spine of a female adolescent patient show a severe right thoracic and left lumbar scoliosis. The patient underwent a posterior spinal fusion using bilateral rod instrumentation with convex segmental pedicle screw fixation allowing for correction maneuvers and the concave supportive rod augmenting the construct. This produced good deformity correction and a balanced spine in the coronal and sagittal planes (c-d)
All-screw constructs have achieved superior correction in the coronal and axial planes when compared to hook instrumentation. Suk et al.16 reported major curve correction of 72% using an all-screw construct compared to 55% in all-hook instrumentation. Loss of scoliosis correction at followup was also less (1% and 6% respectively). Kim et al.4 documented significantly better major curve correction with all-screw when compared to hybrid constructs; this was associated with significant improvement in pulmonary function due to better chest alignment. Lowenstein et al. compared all pedicle screw with hybrid constructs (thoracic hooks/lumbar screws) and found a trend toward better correction with the former.36
There is controversy in terms of the ability of all-screw instrumentation to restore thoracic kyphosis due to its stiffness, which does not allow settling of the disc spaces that occurs with all-hook constructs. Kim et al.4 and Vora et al.37 found a reduction in thoracic kyphosis in patients treated with pedicle screws. Quan and Gibson34 showed that increased thoracic scoliosis correction occurred at the expense of sagittal balance resulting in hypokyphosis. There are, however, previous reports of improved thoracic kyphosis after scoliosis correction using all-pedicle screw as opposed to all-hook instrumentation.36,38,39
Besides producing good correction, all-screw constructs may save distal mobile levels. In the treatment of single thoracic curves, fusion can be limited to the neutrally rotated vertebra or the one above instead of extending to the stable vertebra (which is the vertebra most closely bisected by CSVL Central Sacral Vertical Line).40 Kim et al.4 reported saving an average of 0.8 vertebral levels with pedicle screw constructs. All-screw constructs may also prevent crankshaft phenomenon in young patients.41,42 All-hook or hybrid constructs are not stiff enough to arrest continuous anterior vertebral growth after posterior arthrodesis. The use of pedicle screw systems has limited the need for anterior spinal release even in severe and rigid curves 70-100°.17
COMPLICATIONS OF PEDICLE SCREWS
Pedicle screw-related complications may occur due to initial screw malposition or screw pull-out during correction maneuvers resulting in neurological, vascular or visceral injury, as well as loss of stability in the postoperative period. Screw misplacement is the most common complication (up to 15.7%) associated with thoracic pedicle screw passage in AIS.43 Medial, lateral, or anterior cortical breach may result in serious complications which can be life-threatening. A medial breach, reported from 1.7-14%, may lead to dural leaks and/or neurological injury, especially when this occurs at the levels of the spinal cord (1.2-3%).20,21,43,44 A lateral or anterior vertebral penetration may result in acute or delayed perforation of the aorta, inferior vena cava, iliac vessels, lumbar arteries, esophagus, lungs, ureter, and bowels.3,5,45,46,47,48,49,50,51,52,53 The risk of visceral and neural injury is highest from T4 to T7 because the pedicle channels are narrowest across these levels. Proximity of great vessels along with a narrow spinal canal increases the potential risk of injury. Despite the high risk of screw misplacement, most of the complications are sporadic and have been published as single case reports. Death after cardiac tamponade due to penetration of the coronary artery by a pedicle screw has been reported.54 One temporary neurological complication was reported among 1666 patients treated with pedicle screw constructs.21 The rate for revision for screw malposition has ranged from 0.83% to 4.3% for asymptomatic intrathoracic screw placement, pleural effusion, transient paraparesis, and penetration of the anterior vertebral body.43 This rate of complications may appear to be low and possibly does not reflect the general practice as most of the reports originate from high-volume spinal centers with experienced surgeons. The technique of scoliosis correction with pedicle screw instrumentation has a distinct learning curve and should be practiced only after proper training. Meticulous surgical technique, adequate imaging, and intraoperative monitoring are mandatory to minimize complications.
SURGICAL CONSIDERATIONS
Anterior scoliosis surgery
Anterior spinal fusion in AIS is usually indicated: (a) To arrest anterior vertebral growth in very young and skeletally immature children in order to prevent crankshaft effect, (b) increase flexibility and allow for correction of very rigid curves, and (c) reduce the number of vertebrae that need to be included in the fusion and preserve spinal mobility.
Thoracic scoliosis
Anterior release followed by posterior instrumented fusion allows better correction of severe AIS, especially if all hook or hybrid instrumentation is used. This can be performed through an open thoracotomy with complete excision of the discs and adjacent end plates across the apex of the curve back to the posterior longitudinal ligament. Simultaneous access to perform an internal thoracoplasty adds the additional benefit or removing consecutive rib heads across the apical levels of the scoliosis and improves the cosmetic outcome of the procedure. Disadvantages include increased total surgical time, blood loss, hospital and intensive care unit (ICU) stay, pulmonary compromise at least immediate postoperatively, and greater patient morbidity due to the two procedures, even when these are performed under the same anesthetic. Primary contraindication to anterior spinal surgery is inadequate pulmonary reserves which require a careful preoperative cardiopulmonary assessment.55 Betz et al.56 compared the results of anterior instrumentation with that of posterior multisegmented instrumentation for the correction of thoracic AIS and concluded equal coronal correction and balance with both. The advantages with anterior instrumentation included better correction of sagittal profile in patients with preoperative hypokyphosis less than 20° and an average saving of 2.5 lumbar levels.
Video-assisted thoracoscopy (VATS) has been promoted as an alternative to conventional thoracotomy but its theoretical advantages of better cosmesis and less surgical trauma are negated by increased operative time and ICU stay, as well as the inability to perform same extent of anterior release through a closed technique.55,57 Pulmonary function following VATS, although significantly preserved initially has been comparable to open surgery at final followup.58 In addition, this technique has a steep learning curve for the surgeon and requires instruments that are not available in every Spinal Center. In the current context of all-pedicle screw constructs, the need for anterior release has been limited as severe curves ranging 70-100° can be corrected through posterior-only approaches.17
Thoracolumbar/lumbar scoliosis
Thoracolumbar and lumbar curves of average severity can be well-corrected by an anterior instrumented fusion. Potential advantages include saving mobile spinal segments both proximally and distally, achieving better deformity correction due to more effective direct vertebral derotation once the discs across the curve apex have been excised, as well as reducing the risk of proximal junctional kyphosis [Figure 3]. Historically, anterior instrumentation introduced by Dwyer59 and Moe et al.,60 used single soft rods and had limited ability to correct the deformity while producing a kyphogenic effect and high rates of pseudoarthrosis.61 Addition of an anterior 3.2 mm threaded rod improved the derotational effect but continued to have high rates of nonunion.62 The introduction of solid rods produced good coronal correction and reduced the kyphosing effect when used in conjunction with anterior structural support including freshfrozen tricortical iliac, fibular, and femoral ring or autologous rib grafts, as well as titanium mesh cages.63 When the transvertebral anterior screws are positioned posteriorly and compressed over the rod with the intervening graft in place, the anterior disc spaces are opened and lordosis can be restored. The screws should be bicortical at all levels to maximize bone purchase. Recent addition of two solid rods enhanced coronal correction and fusion rates.64
Figure 3.
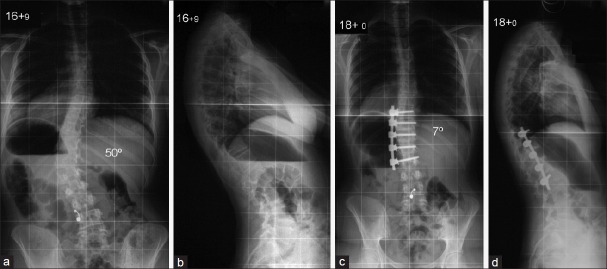
Posteroanterior (a) and lateral (b) radiographs of the spine of a female adolescent patient show a thoracolumbar scoliosis. An anterior spinal fusion using a convex rod and segmental transvertebral screws, as well as rib autograft in the disc spaces produced excellent deformity correction and a balanced spine in the coronal and sagittal planes (c and d)
Hall et al.65 introduced the concept of short fusion in very flexible curves. If the scoliosis apex is at a vertebral body, an additional body above and below are included in the fusion; when the apex is at a disc, the fusion extends to incorporate four vertebral bodies and three discs. However, the curves amenable to this treatment are few and difficult to identify. This concept may also produce kyphosing effects over the fused segments.65 Shufflebarger et al.66 described a method of wide posterior releases which include excision of the interspinous ligament, ligamentum flavum and facet joints as an alternative to anterior release along with posterior instrumentation. Better results were achieved with the use of pedicle screw instrumentation.
Thoracoplasty
The aim of thoracoplasty is to reduce the rib prominence across the convexity of major thoracic curves as the chest wall deformity remains often unacceptable even after adequate scoliosis correction has been achieved with modern techniques. The data in the literature remain contradictory with studies reporting a negative effect of thoracoplasty on pulmonary function,67 while other reports suggested superior rib hump correction and higher patient satisfaction with insignificant respiratory compromise.68 Concave rib resections have also been used in an attempt to release rigid apical scoliotic deformity and allow for better curve correction but have been associated with increased pulmonary morbidity.69 In contrast, Saleh et al.70 reported improved respiratory function following scoliosis correction when concave rib osteotomies were performed. In the authors’ experience, convex thoracoplasty can produce consistently better cosmetic results when performed anteriorly as part of an anterior spinal release as opposed to posteriorly as this allows complete resection of the rib heads and adjacent 2 cm of the apical ribs. We have experienced worst results when we performed a posterior thoracoplasty to address acutely sharp rib humps which are located far later to the spine; in some of these patients, the excised ribs healed in an even sharper angle producing a more unacceptable deformity and patient dissatisfaction.
Vertebral column resection
Circumferential Vertebral Column Resection (VCR) coupled with concave rib osteotomies and convex thoracoplasties was popularized by Bradford71 for correction of severe and rigid curves not amenable to combined anterior and posterior disc releases. This is a formidable last-resort technique associated with severe potential complications including dural tears, arachnoiditis, transient neurological weakness, wound infections, pulmonary compromise, and pneumonia.71 More recently, posterior VCR has been described and has achieved dramatic deformity corrections.72,73 Posterior VCR creates a gap in the vertebral column by excision of the posterior and anterior bony elements, as well as the intervening discs across one or more segments that needs to be reconstructed by an anterior cage and bone grafting followed by posterior instrumented fusion.72 This procedure is technically demanding and may be associated with severe neurological and medical complications. Suk et al.72 who pioneered this technique reported complete spinal cord transection in two of their patients undergoing posterior VCR; other complications included hematoma with cauda equina syndrome, nerve root injuries, wound infection, hemo- and pneumo-thorax. There were five fixation failures which required prolonged immobilization in cast.72
Selection of fusion levels
The traditional Harrington technique was based on the concept of fusing the spine within the stable zone which lies between two vertical lines drawn perpendicular to a line joining the iliac crests beginning from the lumbosacral facets.74 The fusion was recommended from one level above to 2 levels below the measured curve, if the end vertebra lied within this zone. Ferguson75 suggested fusion between vertebrae that had parallel distant surfaces. Moe76 suggested extent of fusion to include the rotationally neutral vertebrae at the proximal and distal ends of the scoliosis.
In the era of modern instrumentation which provides rigid segmental fixation, it has been possible to limit fusion levels and preserve spinal mobility. The concept of selective fusion refers to the fusion of only the structurally major curve which has a greater Cobb angle and significant vertebral rotation, is more rigid, and deviates from the midline while leaving the spinal segments along the minor curves unfused.77 Selective fusion can be performed for major thoracic scoliosis (King type 3 and 4) with an associated small and flexible compensatory lumbar curve. It can also be done for major thoracolumbar/lumbar scoliosis with a compensatory minimally rotated and correctable thoracic curve. A structural thoracic curve that imparts shoulder asymmetry, produces a sharp rib-hump deformity, and is stiffer on supine bending films should be included in the fusion. In the event of a selective fusion, slight under-correction of the primary curve across the levels of the instrumented fusion is desirable to achieve balancing of the spine over the thoracic and lumbar components of the deformity. King et al. proposed selective fusion extending to the stable vertebra distally.78 If the lumbar spine requires to be fused, the distal limit should preferably be L3 or L4 to preserve as many motion segments as possible. In double thoracic curves (King type 5), the inclusion of the proximal curve in the arthrodesis depends upon its structural characteristics. The usual curve pattern is right lower thoracic and left upper thoracic scoliosis. A higher left shoulder and inability to correct to less than 25° on supine bending films make grounds for inclusion of the proximal thoracic curve in the instrumented arthrodesis.
Lenke's classification has allowed better-defined criteria for selective fusion.77 Minor curves are included in the fusion only if these are structurally defined by inflexibility of the curve to ≥ 25° on supine bending films or hyperkyphosis ≥ 20° on a lateral view. Selective fusion can be performed predictably for type 1C, 2C, and 5C curves. For a selective thoracic fusion to be successful in type 3 scoliosis, the thoracolumbar/lumbar curve should be small, more flexible, minimally rotated, and translated from the midline. In Lenke, type 3C and 6C scoliosis where both the thoracic and thoracolumbar/lumbar curves are structural, additional radiographic criteria can be used including the ratios of Cobb angle measurements, apical vertebral translation (AVT), apical vertebral rotation (AVR), and lower instrumented vertebra angle. Selective thoracic fusion can be successful in type 3C scoliosis if the ratios of Cobb angle, AVT, and AVR measurements for thoracic: Thoracolumbar/lumbar curves are ≥ 1.2. In type 6C scoliosis, selective thoracolumbar/lumbar fusion can be successful if the same ratios for thoracolumbar/lumbar: Thoracic curves are ≥ 1.25. Ratios approaching 1 imply almost equal curves in magnitude and structural characteristics, thereby increasing the risk for a selective fusion to fail.
Spinal decompensation
Spinal decompensation after scoliosis correction can affect the coronal or the sagittal planes. Coronal decompensation can occur following short selective fusions for double curves when the thoracic and lumbar components are similar in size and structural measurements.79 In these circumstances, the minor curve may not adapt after fusion of the major scoliosis leading to progressive deformity and decompensation. Other causes include overcorrection of the major curve, which the minor curve is unable to compensate for. King type 2 and double major scoliotic patterns are especially prone to produce decompensation after selective fusion due to flexibility difference between the lumbar and thoracic components of the deformity. A double thoracic scoliosis may also lead to decompensation if the structural nature of the proximal curve is underestimated. Selective fusions are less effective in skeletally immature patients, particularly those with open tri-radiate cartilage and Risser 0, as a compensatory curve can develop into a structural deformity during the remaining growing years.
Sagittal decompensation producing a flat back deformity was a common complication of the Harrington technique. The use of segmental hook or screw instrumentation can also produce decompensation in the sagittal plane in the form of junctional kyphosis.80 This can be due to: (a) Destruction of the interspinous/supraspinous ligaments and proximal facets above the most cephalad instrumented segment, (b) failure to restore normal thoracic kyphosis and stopping the arthrodesis at a level of the thoracic region which is posterior to the weight-bearing axis of the spine, (c) not including the proximal sagittally tilted end vertebra in the fusion and applying excessive compression to the last instrumented vertebra. Fusing all levels which are sagitally tilted and prevention of the instrumentation ending at apical zones both sagittal and coronal can prevent decompensation.80
Fusionless surgery
Ongoing research is focused on fusionless techniques to modulate spinal growth and avoid or delay the need for fusion. Epiphysiodesis on the convex side with stapling of the anterior vertebral growth plates is a novel method, whose effectiveness needs to be proved and guidelines for patient selection and indications need to be clearly defined.81 Growing rod techniques are widely used to delay the fusion surgery in patients with infantile or juvenile scoliosis but have very limited role in AIS.82
OUTCOME MEASURES OF SURGICAL TREATMENT
Health-related quality of life questionnaires, such as Short Form (SF)-36 have been designed to measure outcomes and efficacy of treatment methods in scoliosis. SF-36 had several psychometric shortcomings, overlapping domains, insufficient validation and was difficult for the patient to complete.83 These limitations have been addressed by the introduction of the Scoliosis Research Society-22 (SRS-22) questionnaire, which has been widely used in the analysis of clinical and functional outcomes, and patients’ satisfaction.84 The SRS-22 scale comprises of a total score, as well as five domains including function, pain, self-image, mental health and satisfaction after treatment.84
Personal satisfaction and self-esteem are important parameters of human life. Low self-esteem, depression, feeling of loneliness, increased incidence of suicidal thoughts and alcohol consumption have been reported in teenagers and young adults with AIS.85 Surgical treatment can lead to improvement in self-confidence and life satisfaction when compared to lack of management.86 An improved self-image has been found to be the greatest benefit of surgery in AIS.86 Cosmetic satisfaction following surgery has been related to better deformity correction which is maximized with the use of pedicle screw instrumentation.87
Mechanical back pain can affect up to 3/4 of adolescents with idiopathic scoliosis and this has been significantly reduced 2 years after posterior correction.88 Long term studies reported no increase in pain after posterior fusion for AIS with Harrington instrumentation.89,90,91,92,93,94 Backache and functional status 21 years following posterior scoliosis correction were found to be comparable to normal individuals.89 Cochran et al.95 recorded a co-relation between postoperative pain and distal extent of fusion; patients reported pain at a rate of 25% when the fusion stopped at L1, 30% at L2, 39% at L3, 62% at L4, and 82% at L5 compared to 53% age-matched healthy controls. Bartie et al.96 also noted that distal fusions were associated with more pain than controls. Selective fusions using pedicle screw instrumentation can save fusion levels and may reduce incidence of postoperative back pain; however, data on long term outcomes are not as yet available. An analysis of patients who underwent anterior instrumented fusion for thoracolumbar and lumbar AIS after 17 years revealed good SRS and Oswestry scores.97 The patients were able to pursue their career and family activities despite degenerative changes. Danielsson and Nachemson98 found no difference in the rate of marriage and child bearing between operated AIS patients and controls.
CONCLUSION
The surgical treatment of AIS has been revolutionized over the last few decades from the initial un-instrumented in situ fusions to the use of modern pedicle screw constructs which can achieve and maintain dramatic deformity corrections. The application of current advanced correction techniques requires extensive surgical training and a wide multidisciplinary set-up of resources in order to secure clinical safety and produce optimum results. It is important to keep in mind that for any type of scoliosis, the amount of correction reflects a measure of technical competence but does not necessarily relate to patient satisfaction which is the primary goal of surgery. Therefore, surgical results have to be assessed through outcome measures which represent patients’ perception on the success or failure of treatment. Scoliosis surgery has entered an era when spinal surgeons have to justify their practices based on outcomes as demonstrated through patient quality-of-life assessments. Cost implications have to be taken into account as health economics play increasingly a determining role in provision of care within modern health systems. The future of treatment in AIS may lie in early diagnosis of those children who are likely to develop a scoliosis through genetic counseling and those curves which carry greater risk of progression followed by instigation of early conservative or fusionless techniques. Spinal fusion will hopefully be limited only to a minority of patients who, despite all measures develop progressive severe scoliosis.
Footnotes
Source of Support: Nil
Conflict of Interest: None
REFERENCES
- 1.Boucher HH. A method of spinal fusion. J Bone Joint Surg Br. 1959;41-B:248–59. doi: 10.1302/0301-620X.41B2.248. [DOI] [PubMed] [Google Scholar]
- 2.Roy-Camille R, Saillant G, Mazel C. Internal fixation of the lumbar spine with pedicle screw plating. Clin Orthop Relat Res. 1986;203:7–17. [PubMed] [Google Scholar]
- 3.Vaccaro AR, Rizzolo SJ, Balderston RA, Allardyce TJ, Garfin SR, Dolinskas C, et al. Placement of pedicle screws in the thoracic spine. Part II: An anatomical and radiographic assessment. J Bone Joint Surg Am. 1995;77:1200–6. doi: 10.2106/00004623-199508000-00009. [DOI] [PubMed] [Google Scholar]
- 4.Kim YJ, Lenke LG, Cho SK, Bridwell KH, Sides B, Blanke K. Comparative analysis of pedicle screw versus hook instrumentation in posterior spinal fusion of adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 2004;29:2040–8. doi: 10.1097/01.brs.0000138268.12324.1a. [DOI] [PubMed] [Google Scholar]
- 5.Vaccaro AR, Rizzolo SJ, Allardyce TJ, Ramsey M, Salvo J, Balderston RA, et al. Placement of pedicle screws in the thoracic spine. Part I: Morphometric analysis of the thoracic vertebrae. J Bone Joint Surg Am. 1995;77:1193–9. doi: 10.2106/00004623-199508000-00008. [DOI] [PubMed] [Google Scholar]
- 6.Rampersaud YR, Simon DA, Foley KT. Accuracy requirements for image-guided spinal pedicle screw placement. Spine (Phila Pa 1976) 2001;26:352–9. doi: 10.1097/00007632-200102150-00010. [DOI] [PubMed] [Google Scholar]
- 7.Polly DW, Jr, Potter BK, Kuklo T, Young S, Johnson C, Klemme WR. Volumetric spinal canal intrusion: A comparison between thoracic pedicle screws and thoracic hooks. Spine (Phila Pa 1976) 2004;29:63–9. doi: 10.1097/01.BRS.0000105525.06564.56. [DOI] [PubMed] [Google Scholar]
- 8.Gertzbein SD, Robbins SE. Accuracy of pedicular screw placement in vivo. Spine (Phila Pa 1976) 1990;15:11–4. doi: 10.1097/00007632-199001000-00004. [DOI] [PubMed] [Google Scholar]
- 9.Kim YJ, Lenke LG, Cheh G, Riew KD. Evaluation of pedicle screw placement in the deformed spine using intraoperative plain radiographs: A comparison with computerized tomography. Spine (Phila Pa 1976) 2005;30:2084–8. doi: 10.1097/01.brs.0000178818.92105.ec. [DOI] [PubMed] [Google Scholar]
- 10.Ebraheim NA, Jabaly G, Xu R, Yeasting RA. Anatomic relations of the thoracic pedicle to the adjacent neural structures. Spine (Phila Pa 1976) 1997;22:1553–6. doi: 10.1097/00007632-199707150-00002. [DOI] [PubMed] [Google Scholar]
- 11.Papin P, Arlet V, Marchesi D, Rosenblatt B, Aebi M. Unusual presentation of spinal cord compression related to misplaced pedicle screws in thoracic scoliosis. Eur Spine J. 1999;8:156–9. doi: 10.1007/s005860050147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Smorgick Y, Millgram MA, Anekstein Y, Floman Y, Mirovsky Y. Accuracy and safety of thoracic pedicle screw placement in spinal deformities. J Spinal Disord Tech. 2005;18:522–6. doi: 10.1097/01.bsd.0000154448.90707.a8. [DOI] [PubMed] [Google Scholar]
- 13.Kothe R, O’Holleran JD, Liu W, Panjabi MM. Internal architecture of the thoracic pedicle. An anatomic study. Spine (Phila Pa 1976) 1996;21:264–70. doi: 10.1097/00007632-199602010-00002. [DOI] [PubMed] [Google Scholar]
- 14.Belmont PJ, Jr, Klemme WR, Dhawan A, Polly DW., Jr In vivo accuracy of thoracic pedicle screws. Spine (Phila Pa 1976) 2001;26:2340–6. doi: 10.1097/00007632-200111010-00010. [DOI] [PubMed] [Google Scholar]
- 15.O’Brien MF, Lenke LG, Mardjetko S, Lowe TG, Kong Y, Eck K, et al. Pedicle morphology in thoracic adolescent idiopathic scoliosis: Is pedicle fixation an anatomically viable technique? Spine (Phila Pa 1976) 2000;25:2285–93. doi: 10.1097/00007632-200009150-00005. [DOI] [PubMed] [Google Scholar]
- 16.Suk SI, Lee CK, Kim WJ, Chung YJ, Park YB. Segmental pedicle screw fixation in the treatment of thoracic idiopathic scoliosis. Spine (Phila Pa 1976) 1995;20:1399–405. [PubMed] [Google Scholar]
- 17.Luhmann SJ, Lenke LG, Kim YJ, Bridwell KH, Schootman M. Thoracic adolescent idiopathic scoliosis curves between 70 degrees and 100 degrees: Is anterior release necessary? Spine (Phila Pa 1976) 2005;30:2061–7. doi: 10.1097/01.brs.0000179299.78791.96. [DOI] [PubMed] [Google Scholar]
- 18.Kuklo TR, Lenke LG, O’Brien MF, Lehman RA, Jr, Polly DW, Jr, Schroeder TM. Accuracy and efficacy of thoracic pedicle screws in curves more than 90 degrees. Spine (Phila Pa 1976) 2005;30:222–6. doi: 10.1097/01.brs.0000150482.26918.d8. [DOI] [PubMed] [Google Scholar]
- 19.Zindrick MR, Wiltse LL, Doornik A, Widell EH, Knight GW, Patwardhan AG, et al. Analysis of the morphometric characteristics of the thoracic and lumbar pedicles. Spine (Phila Pa 1976) 1987;12:160–6. doi: 10.1097/00007632-198703000-00012. [DOI] [PubMed] [Google Scholar]
- 20.Kim YJ, Lenke LG, Bridwell KH, Cho YS, Riew KD. Free hand pedicle screw placement in the thoracic spine: Is it safe? Spine (Phila Pa 1976) 2004;29:333–42. doi: 10.1097/01.brs.0000109983.12113.9b. [DOI] [PubMed] [Google Scholar]
- 21.Suk SI, Kim WJ, Lee SM, Kim JH, Chung ER. Thoracic pedicle screw fixation in spinal deformities: Are they really safe? Spine (Phila Pa 1976) 2001;26:2049–57. doi: 10.1097/00007632-200109150-00022. [DOI] [PubMed] [Google Scholar]
- 22.Watanabe K, Lenke LG, Matsumoto M, Harimaya K, Kim YJ, Hensley M, et al. A novel pedicle channel classification describing osseous anatomy: How many thoracic scoliotic pedicles have cancellous channels? Spine (Phila Pa 1976) 2010;35:1836–42. doi: 10.1097/BRS.0b013e3181d3cfde. [DOI] [PubMed] [Google Scholar]
- 23.Misenhimer GR, Peek RD, Wiltse LL, Rothman SL, Widell EH., Jr Anatomic analysis of pedicle cortical and cancellous diameter as related to screw size. Spine (Phila Pa 1976) 1989;14:367–72. doi: 10.1097/00007632-198904000-00004. [DOI] [PubMed] [Google Scholar]
- 24.Cinotti G, Gumina S, Ripani M, Postacchini F. Pedicle instrumentation in the thoracic spine. A morphometric and cadaveric study for placement of screws. Spine (Phila Pa 1976) 1999;24:114–9. doi: 10.1097/00007632-199901150-00003. [DOI] [PubMed] [Google Scholar]
- 25.Krag MH, Beynnon BD, Pope MH, Frymoyer JW, Haugh LD, Weaver DL. An internal fixator for posterior application to short segments of the thoracic, lumbar, or lumbosacral spine. Design and testing. Clin Orthop Relat Res. 1986;203:75–98. [PubMed] [Google Scholar]
- 26.Lehman RA, Jr, Polly DW, Jr, Kuklo TR, Cunningham B, Kirk KL, Belmont PJ., Jr Straight-forward versus anatomic trajectory technique of thoracic pedicle screw fixation: A biomechanical analysis. Spine (Phila Pa 1976) 2003;28:2058–65. doi: 10.1097/01.BRS.0000087743.57439.4F. [DOI] [PubMed] [Google Scholar]
- 27.White KK, Oka R, Mahar AT, Lowry A, Garfin SR. Pullout strength of thoracic pedicle screw instrumentation: Comparison of the transpedicular and extrapedicular techniques. Spine (Phila Pa 1976) 2006;31:E355–8. doi: 10.1097/01.brs.0000219394.48091.d6. [DOI] [PubMed] [Google Scholar]
- 28.Kuklo TR, Lehman RA., Jr Effect of various tapping diameters on insertion of thoracic pedicle screws: A biomechanical analysis. Spine (Phila Pa 1976) 2003;28:2066–71. doi: 10.1097/01.BRS.0000084665.31967.02. [DOI] [PubMed] [Google Scholar]
- 29.Hackenberg L, Link T, Liljenqvist U. Axial and tangential fixation strength of pedicle screws versus hooks in the thoracic spine in relation to bone mineral density. Spine (Phila Pa 1976) 2002;27:937–42. doi: 10.1097/00007632-200205010-00010. [DOI] [PubMed] [Google Scholar]
- 30.Ul Haque M, Shufflebarger HL, O’Brien M, Macagno A. Radiation exposure during pedicle screw placement in adolescent idiopathic scoliosis: Is fluoroscopy safe? Spine (Phila Pa 1976) 2006;31:2516–20. doi: 10.1097/01.brs.0000238675.91612.2f. [DOI] [PubMed] [Google Scholar]
- 31.Cui G, Wang Y, Kao TH, Zhang Y, Liu Z, Liu B, et al. Application of intraoperative computed tomography with or without navigation system in surgical correction of spinal deformity: A preliminary result of 59 consecutive human cases. Spine (Phila Pa 1976) 2012;37:891–900. doi: 10.1097/BRS.0b013e31823aff81. [DOI] [PubMed] [Google Scholar]
- 32.Hicks JM, Singla A, Shen FH, Arlet V. Complications of pedicle screw fixation in scoliosis surgery: A systematic review. Spine (Phila Pa 1976) 2010;35:E465–70. doi: 10.1097/BRS.0b013e3181d1021a. [DOI] [PubMed] [Google Scholar]
- 33.Vallespir GP, Flores JB, Trigueros IS, Sierra EH, Fernández PD, Olaverri JC, et al. Vertebral coplanar alignment: A standardized technique for three dimensional correction in scoliosis surgery: Technical description and preliminary results in Lenke type 1 curves. Spine (Phila Pa 1976) 2008;33:1588–97. doi: 10.1097/BRS.0b013e3181788704. [DOI] [PubMed] [Google Scholar]
- 34.Quan GM, Gibson MJ. Correction of main thoracic adolescent idiopathic scoliosis using pedicle screw instrumentation: Does higher implant density improve correction? Spine (Phila Pa 1976) 2010;35:562–7. doi: 10.1097/BRS.0b013e3181b4af34. [DOI] [PubMed] [Google Scholar]
- 35.Tsirikos AI, Subramanian AS. Posterior spinal arthrodesis for adolescent idiopathic scoliosis using pedicle screw instrumentation: Does a bilateral or unilateral screw technique affect surgical outcome? J Bone Joint Surg Br. 2012;94:1670–7. doi: 10.1302/0301-620X.94B12.29403. [DOI] [PubMed] [Google Scholar]
- 36.Lowenstein JE, Matsumoto H, Vitale MG, Weidenbaum M, Gomez JA, Lee FY, et al. Coronal and sagittal plane correction in adolescent idiopathic scoliosis: A comparison between all pedicle screw versus hybrid thoracic hook lumbar screw constructs. Spine (Phila Pa 1976) 2007;32:448–52. doi: 10.1097/01.brs.0000255030.78293.fd. [DOI] [PubMed] [Google Scholar]
- 37.Vora V, Crawford A, Babekhir N, Boachie-Adjei O, Lenke L, Peskin M, et al. A pedicle screw construct gives an enhanced posterior correction of adolescent idiopathic scoliosis when compared with other constructs: Myth or reality. Spine (Phila Pa 1976) 2007;32:1869–74. doi: 10.1097/BRS.0b013e318108b912. [DOI] [PubMed] [Google Scholar]
- 38.Suk SI, Kim WJ, Kim JH, Lee SM. Restoration of thoracic kyphosis in the hypokyphotic spine: A comparison between multiple-hook and segmental pedicle screw fixation in adolescent idiopathic scoliosis. J Spinal Disord. 1999;12:489–95. [PubMed] [Google Scholar]
- 39.Clement JL, Chau E, Kimkpe C, Vallade MJ. Restoration of thoracic kyphosis by posterior instrumentation in adolescent idiopathic scoliosis: Comparative radiographic analysis of two methods of reduction. Spine (Phila Pa 1976) 2008;33:1579–87. doi: 10.1097/BRS.0b013e31817886be. [DOI] [PubMed] [Google Scholar]
- 40.Suk SI, Lee SM, Chung ER, Kim JH, Kim WJ, Sohn HM. Determination of distal fusion level with segmental pedicle screw fixation in single thoracic idiopathic scoliosis. Spine (Phila Pa 1976) 2003;28:484–91. doi: 10.1097/01.BRS.0000048653.75549.40. [DOI] [PubMed] [Google Scholar]
- 41.Burton DC, Asher MA, Lai SM. Scoliosis correction maintenance in skeletally immature patients with idiopathic scoliosis. Is anterior fusion really necessary? Spine (Phila Pa 1976) 2000;25:61–8. doi: 10.1097/00007632-200001010-00012. [DOI] [PubMed] [Google Scholar]
- 42.Sarlak AY, Atmaca H, Buluç L, Tosun B, Musaogğlu R. Juvenile idiopathic scoliosis treated with posterior arthrodesis and segmental pedicle screw instrumentation before the age of 9 years: A 5-year followup. Scoliosis. 2009;4:1. doi: 10.1186/1748-7161-4-1. doi: 10.1186/1748-7161-4-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Di Silvestre M, Parisini P, Lolli F, Bakaloudis G. Complications of thoracic pedicle screws in scoliosis treatment. Spine (Phila Pa 1976) 2007;32:1655–61. doi: 10.1097/BRS.0b013e318074d604. [DOI] [PubMed] [Google Scholar]
- 44.Di Silvestre M, Bakaloudis G, Lolli F, Vommaro F, Martikos K, Parisini P. Posterior fusion only for thoracic adolescent idiopathic scoliosis of more than 80 degrees: Pedicle screws versus hybrid instrumentation. Eur Spine J. 2008;17:1336–49. doi: 10.1007/s00586-008-0731-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Stewart JR, Barth KH, Williams GM. Ruptured lumbar artery pseudoaneurysm: An unusual cause of retroperitoneal hemorrhage. Surgery. 1983;93:592–4. [PubMed] [Google Scholar]
- 46.Jendrisak MD. Spontaneous abdominal aortic rupture from erosion by a lumbar spine fixation device: A case report. Surgery. 1986;99:631–3. [PubMed] [Google Scholar]
- 47.Vanichkachorn JS, Vaccaro AR, Cohen MJ, Cotler JM. Potential large vessel injury during thoracolumbar pedicle screw removal. A case report. Spine (Phila Pa 1976) 1997;22:110–3. doi: 10.1097/00007632-199701010-00018. [DOI] [PubMed] [Google Scholar]
- 48.O’Brien JR, Krushinski E, Zarro CM, Sciadini M, Gelb D, Ludwig S. Esophageal injury from thoracic pedicle screw placement in a polytrauma patient: A case report and literature review. J Orthop Trauma. 2006;20:431–4. doi: 10.1097/00005131-200607000-00012. [DOI] [PubMed] [Google Scholar]
- 49.Wegener B, Birkenmaier C, Fottner A, Jansson V, Dürr HR. Delayed perforation of the aorta by a thoracic pedicle screw. Eur Spine J. 2008;17:S351–4. doi: 10.1007/s00586-008-0715-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Watanabe K, Yamazaki A, Hirano T, Izumi T, Sano A, Morita O, et al. Descending aortic injury by a thoracic pedicle screw during posterior reconstructive surgery: A case report. Spine (Phila Pa 1976) 2010;35:E1064–8. doi: 10.1097/BRS.0b013e3181ed29c1. [DOI] [PubMed] [Google Scholar]
- 51.Clarke MJ, Guzzo J, Wolinsky JP, Gokaslan Z, Black JH., 3rd Combined endovascular and neurosurgical approach to the removal of an intraaortic pedicle screw. J Neurosurg Spine. 2011;15:550–4. doi: 10.3171/2011.7.SPINE10267. [DOI] [PubMed] [Google Scholar]
- 52.Tschoeke SK, Gahr P, Krug L, Kasper AS, Heyde CE, Ertel W. Late diagnosis of pedicle screw malplacement with perforation of the thoracic aorta after posterior stabilization in a patient with multiple myeloma: Case report. Spine (Phila Pa 1976) 2011;36:E886–90. doi: 10.1097/BRS.0b013e318202e4d1. [DOI] [PubMed] [Google Scholar]
- 53.Sandri A, Regis D, Marino MA, Puppini G, Bartolozzi P. Lumbar artery injury following posterior spinal instrumentation for scoliosis. Orthopedics. 2011;34 doi: 10.3928/01477447-20110228-24. doi: 10.3928/01477447-20110228-24. [DOI] [PubMed] [Google Scholar]
- 54.Heini P, Schöll E, Wyler D, Eggli S. Fatal cardiac tamponade associated with posterior spinal instrumentation. A case report. Spine (Phila Pa 1976) 1998;23:2226–30. doi: 10.1097/00007632-199810150-00017. [DOI] [PubMed] [Google Scholar]
- 55.Lenke LG. Anterior endoscopic discectomy and fusion for adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 2003;28:S36–43. doi: 10.1097/01.BRS.0000076896.14492.DC. [DOI] [PubMed] [Google Scholar]
- 56.Betz RR, Harms J, Clements DH, 3rd, Lenke LG, Lowe TG, Shufflebarger HL, et al. Comparison of anterior and posterior instrumentation for correction of adolescent thoracic idiopathic scoliosis. Spine (Phila Pa 1976) 1999;24:225–39. doi: 10.1097/00007632-199902010-00007. [DOI] [PubMed] [Google Scholar]
- 57.Wong HK, Hee HT, Yu Z, Wong D. Results of thoracoscopic instrumented fusion versus conventional posterior instrumented fusion in adolescent idiopathic scoliosis undergoing selective thoracic fusion. Spine (Phila Pa 1976) 2004;29:2031–8. doi: 10.1097/01.brs.0000138304.77946.ea. [DOI] [PubMed] [Google Scholar]
- 58.Lonner BS, Kondrachov D, Siddiqi F, Hayes V, Scharf C. Thoracoscopic spinal fusion compared with posterior spinal fusion for the treatment of thoracic adolescent idiopathic scoliosis. J Bone Joint Surg Am. 2006;88:1022–34. doi: 10.2106/JBJS.E.00001. [DOI] [PubMed] [Google Scholar]
- 59.Dwyer AF, Schafer MF. Anterior approach to scoliosis. Results of treatment in fifty-one cases. J Bone Joint Surg Br. 1974;56:218–24. [PubMed] [Google Scholar]
- 60.Moe JH, Purcell GA, Bradford DS. Zielke instrumentation (VDS) for the correction of spinal curvature. Analysis of results in 66 patients. Clin Orthop Relat Res. 1983;180:133–53. [PubMed] [Google Scholar]
- 61.Kohler R, Galland O, Mechin H, Michel CR, Onimus M. The Dwyer procedure in the treatment of idiopathic scoliosis. A 10-year followup review of 21 patients. Spine (Phila Pa 1976) 1990;15:75–80. doi: 10.1097/00007632-199002000-00005. [DOI] [PubMed] [Google Scholar]
- 62.Lowe TG, Peters JD. Anterior spinal fusion with Zielke instrumentation for idiopathic scoliosis. A frontal and sagittal curve analysis in 36 patients. Spine (Phila Pa 1976) 1993;18:423–6. [PubMed] [Google Scholar]
- 63.Bridwell KH. Spinal instrumentation in the management of adolescent scoliosis. Clin Orthop Relat Res. 1997;335:64–72. [PubMed] [Google Scholar]
- 64.Sweet FA, Lenke LG, Bridwell KH, Blanke KM. Maintaining lumbar lordosis with anterior single solid-rod instrumentation in thoracolumbar and lumbar adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 1999;24:1655–62. doi: 10.1097/00007632-199908150-00006. [DOI] [PubMed] [Google Scholar]
- 65.Hall JE, Millis MB, Snyder BD. Short segment anterior instrumentation for thoracolumbar scoliosis. In: Bridwell KH, DeWald RL, editors. The Textbook of Spinal Surgery. 2nd ed. Philadelphia: Lippincott-Raven; 1997. pp. 665–74. Ch. 43. [Google Scholar]
- 66.Shufflebarger HL, Geck MJ, Clark CE. The posterior approach for lumbar and thoracolumbar adolescent idiopathic scoliosis: Posterior shortening and pedicle screws. Spine (Phila Pa 1976) 2004;29:269–76. doi: 10.1097/01.brs.0000109881.63411.48. [DOI] [PubMed] [Google Scholar]
- 67.Kim YJ, Lenke LG, Bridwell KH, Kim KL, Steger-May K. Pulmonary function in adolescent idiopathic scoliosis relative to the surgical procedure. J Bone Joint Surg Am. 2005;87:1534–41. doi: 10.2106/JBJS.C.00978. [DOI] [PubMed] [Google Scholar]
- 68.Suk SI, Kim JH, Kim SS, Lee JJ, Han YT. Thoracoplasty in thoracic adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 2008;33:1061–7. doi: 10.1097/BRS.0b013e31816f2888. [DOI] [PubMed] [Google Scholar]
- 69.Mann DC, Nash CL, Jr, Wilham MR, Brown RH. Evaluation of the role of concave rib osteotomies in the correction of thoracic scoliosis. Spine (Phila Pa 1976) 1989;14:491–5. doi: 10.1097/00007632-198905000-00003. [DOI] [PubMed] [Google Scholar]
- 70.Saleh AM, Masry MA, West RM, Tsiridis E, Hawary YK. Improved pulmonary function after concave rib resection and posterior instrumentation for idiopathic scoliosis. Acta Orthop Belg. 2010;76:681–3. [PubMed] [Google Scholar]
- 71.Bradford DS, Tribus CB. Vertebral column resection for the treatment of rigid coronal decompensation. Spine (Phila Pa 1976) 1997;22:1590–9. doi: 10.1097/00007632-199707150-00013. [DOI] [PubMed] [Google Scholar]
- 72.Suk SI, Kim JH, Kim WJ, Lee SM, Chung ER, Nah KH. Posterior vertebral column resection for severe spinal deformities. Spine (Phila Pa 1976) 2002;27:2374–82. doi: 10.1097/00007632-200211010-00012. [DOI] [PubMed] [Google Scholar]
- 73.Lenke LG, O’Leary PT, Bridwell KH, Sides BA, Koester LA, Blanke KM. Posterior vertebral column resection for severe pediatric deformity: Minimum two-year followup of thirty-five consecutive patients. Spine (Phila Pa 1976) 2009;34:2213–21. doi: 10.1097/BRS.0b013e3181b53cba. [DOI] [PubMed] [Google Scholar]
- 74.Harrington PR. Technical details in relation to the successful use of instrumentation in scoliosis. Orthop Clin North Am. 1972;3:49–67. [PubMed] [Google Scholar]
- 75.Ferguson AB. The study and treatment of scoliosis. South Med J. 1930;23:116–20. [Google Scholar]
- 76.Moe JH. Methods of correction and surgical techniques in scoliosis. Orthop Clin North Am. 1972;3:17–48. [PubMed] [Google Scholar]
- 77.Lenke LG, Betz RR, Harms J, Bridwell KH, Clements DH, Lowe TG, et al. Adolescent idiopathic scoliosis: A new classification to determine extent of spinal arthrodesis. J Bone Joint Surg Am. 2001;83-A:1169–81. [PubMed] [Google Scholar]
- 78.King HA. Selection of fusion levels for posterior instrumentation and fusion in idiopathic scoliosis. Orthop Clin North Am. 1988;19:247–55. [PubMed] [Google Scholar]
- 79.West J, Boachie-Adjei O, Bradford DS, Ogilvie J. Decompensation following cotrel-dubousset instrumentation: A worrisome complication. Orthop Trans. 1989;13:78–86. [Google Scholar]
- 80.Shufflebarger HL, Clark CE. Fusion levels and hook patterns in thoracic scoliosis with Cotrel-Dubousset instrumentation. Spine (Phila Pa 1976) 1990;15:916–20. doi: 10.1097/00007632-199009000-00015. [DOI] [PubMed] [Google Scholar]
- 81.Betz RR, Kim J, D’Andrea LP, Mulcahey MJ, Balsara RK, Clements DH. An innovative technique of vertebral body stapling for the treatment of patients with adolescent idiopathic scoliosis: A feasibility, safety, and utility study. Spine (Phila Pa 1976) 2003;28:S255–65. doi: 10.1097/01.BRS.0000092484.31316.32. [DOI] [PubMed] [Google Scholar]
- 82.Akbarnia BA, Marks DS, Boachie-Adjei O, Thompson AG, Asher MA. Dual growing rod technique for the treatment of progressive early-onset scoliosis: A multicenter study. Spine (Phila Pa 1976) 2005;30:S46–57. doi: 10.1097/01.brs.0000175190.08134.73. [DOI] [PubMed] [Google Scholar]
- 83.Lai SM, Asher M, Burton D. Estimating SRS-22 quality of life measures with SF-36: Application in idiopathic scoliosis. Spine (Phila Pa 1976) 2006;31:473–8. doi: 10.1097/01.brs.0000200049.94329.f4. [DOI] [PubMed] [Google Scholar]
- 84.Asher M, Min Lai S, Burton D, Manna B. The reliability and concurrent validity of the scoliosis research society-22 patient questionnaire for idiopathic scoliosis. Spine (Phila Pa 1976) 2003;28:63–9. doi: 10.1097/00007632-200301010-00015. [DOI] [PubMed] [Google Scholar]
- 85.Payne WK, 3rd, Ogilvie JW, Resnick MD, Kane RL, Transfeldt EE, Blum RW. Does scoliosis have a psychological impact and does gender make a difference? Spine (Phila Pa 1976) 1997;22:1380–4. doi: 10.1097/00007632-199706150-00017. [DOI] [PubMed] [Google Scholar]
- 86.Zhang J, He D, Gao J, Yu X, Sun H, Chen Z, et al. Changes in life satisfaction and self-esteem in patients with adolescent idiopathic scoliosis with and without surgical intervention. Spine (Phila Pa 1976) 2011;36:741–5. doi: 10.1097/BRS.0b013e3181e0f034. [DOI] [PubMed] [Google Scholar]
- 87.Smucny M, Lubicky JP, Sanders JO, Carreon LY, Diab M. Patient self-assessment of appearance is improved more by all pedicle screw than by hybrid constructs in surgical treatment of adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 2011;36:248–54. doi: 10.1097/BRS.0b013e3181cdb4be. [DOI] [PubMed] [Google Scholar]
- 88.Landman Z, Oswald T, Sanders J, Diab M Spinal Deformity Study Group. Prevalence and predictors of pain in surgical treatment of adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 2011;36:825–9. doi: 10.1097/BRS.0b013e3181de8c2b. [DOI] [PubMed] [Google Scholar]
- 89.Dickson JH, Erwin WD, Rossi D. Harrington instrumentation and arthrodesis for idiopathic scoliosis. A twenty one-year followup. J Bone Joint Surg Am. 1990;72:678–83. [PubMed] [Google Scholar]
- 90.Connolly PJ, Von Schroeder HP, Johnson GE, Kostuik JP. Adolescent idiopathic scoliosis. Long term effect of instrumentation extending to the lumbar spine. J Bone Joint Surg Am. 1995;77:1210–6. doi: 10.2106/00004623-199508000-00011. [DOI] [PubMed] [Google Scholar]
- 91.Pérez-Grueso FS, Fernández-Baíllo N, Arauz de Robles S, García Fernández A. The low lumbar spine below Cotrel-Dubousset instrumentation: Long term findings. Spine (Phila Pa 1976) 2000;25:2333–41. doi: 10.1097/00007632-200009150-00011. [DOI] [PubMed] [Google Scholar]
- 92.Padua R, Padua S, Aulisa L, Ceccarelli E, Padua L, Romanini E, et al. Patient outcomes after Harrington instrumentation for idiopathic scoliosis: A 15- to 28-year evaluation. Spine (Phila Pa 1976) 2001;26:1268–73. doi: 10.1097/00007632-200106010-00019. [DOI] [PubMed] [Google Scholar]
- 93.Helenius I, Remes V, Yrjönen T, Ylikoski M, Schlenzka D, Helenius M, et al. Comparison of long term functional and radiologic outcomes after Harrington instrumentation and spondylodesis in adolescent idiopathic scoliosis: A review of 78 patients. Spine (Phila Pa 1976) 2002;27:176–80. doi: 10.1097/00007632-200201150-00010. [DOI] [PubMed] [Google Scholar]
- 94.Götze C, Liljenqvist UR, Slomka A, Götze HG, Steinbeck J. Quality of life and back pain: Outcome 16.7 years after Harrington instrumentation. Spine (Phila Pa 1976) 2002;27:1456–63. doi: 10.1097/00007632-200207010-00016. [DOI] [PubMed] [Google Scholar]
- 95.Cochran T, Irstam L, Nachemson A. Long term anatomic and functional changes in patients with adolescent idiopathic scoliosis treated by Harrington rod fusion. Spine (Phila Pa 1976) 1983;8:576–84. doi: 10.1097/00007632-198309000-00003. [DOI] [PubMed] [Google Scholar]
- 96.Bartie BJ, Lonstein JE, Winter RB. Long term followup of adolescent idiopathic scoliosis patients who had Harrington instrumentation and fusion to the lower lumbar vertebrae: Is low back pain a problem? Spine (Phila Pa 1976) 2009;34:E873–8. doi: 10.1097/BRS.0b013e3181aa7d53. [DOI] [PubMed] [Google Scholar]
- 97.Kelly DM, McCarthy RE, McCullough FL, Kelly HR. Long term outcomes of anterior spinal fusion with instrumentation for thoracolumbar and lumbar curves in adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 2010;35:194–8. doi: 10.1097/BRS.0b013e3181bc948e. [DOI] [PubMed] [Google Scholar]
- 98.Danielsson AJ, Nachemson AL. Childbearing, curve progression, and sexual function in women 22 years after treatment for adolescent idiopathic scoliosis: A case-control study. Spine (Phila Pa 1976) 2001;26:1449–56. doi: 10.1097/00007632-200107010-00015. [DOI] [PubMed] [Google Scholar]


