Abstract
Parental depression places offspring at elevated risk for multiple, co-occurring problems. The purpose of this study was to develop and preliminarily evaluate Project Hope, a family intervention for the prevention of both depression and substance use among adolescent-aged children (M = 13.9 years) of depressed parents. The program was created by blending two empirically supported interventions: one for depression and another for substance use. Thirty families were randomly assigned to either Project Hope (n = 16) or a wait-list control condition (n = 14). Pretests, posttests (n = 29), and 5-month follow-ups (n = 28) were conducted separately with parents and youth via phone interviews. Questions asked about the family depression experience, family interactions, family management, coping, adolescent substance use beliefs and refusal skills, adolescent depression, and adolescent substance use. Project Hope was fully developed, manualized, and implemented with a small sample of targeted families. Engagement in the program was relatively high. Preliminary outcome analyses were conducted using 2 (Group) ×3 (Time) analyses of covariance. Results provided some evidence for significant improvements among intervention compared to control participants in indicators of the family depression experience, family management, and coping, and a statistically significant decrease from pretest to posttest in alcohol quantity for intervention compared to control youth. Next steps for this program of research are discussed.
Keywords: Family, Depression, Substance use, Prevention, Co-occurrence
Introduction
Co-occurrence of emotional (e.g., depression) and behavioral (e.g., substance use) problems among at-risk youth is common (Sroufe 1997) and typically is associated with greater functional impairment relative to having a particular problem in isolation (Lewinsohn et al. 1995). Once established, co-occurring problems are difficult and costly to treat (Hoff and Rosenheck 1999). Thus, programs designed to prevent multiple problems before they emerge are needed (Biglan et al. 2004), particularly programs that target at-risk youth who struggle with one or more circumstances (e.g., poverty, child maltreatment, parental psychopathology) that place them at increased risk for a range of adverse outcomes (e.g., Compas et al. 2011).
Family intervention provides a powerful way to prevent problems among vulnerable youth (Kumpfer and Alvarado 2003). Theory and research have highlighted the central importance of the family in children's development, both in terms of the risks or protections that the family might confer as well as the opportunities for intervention that exist within the family context (Tolan and Dodge 2005). Most family-based preventive interventions primarily target a particular outcome, such as substance use (e.g., Bauman et al. 2001; Spoth et al. 1998) or conduct problems (e.g., Webster-Stratton 1998). However, family programs explicitly designed to prevent specific patterns of co-occurring emotional and behavioral problems hold promise for reducing the significant personal, social, and financial costs associated with co-occurrence; thus, there is a need to develop and evaluate such programs.
This article introduces Project Hope, a family intervention for the prevention of co-occurring depression and substance use among at-risk youth, and reports findings from a preliminary randomized evaluation of the program. Project Hope results from the adaptation of two evidence-based family programs: one for the prevention of adolescent depression (Hope, Meaning, and Continuity; Beardslee et al. 2003) and another for the prevention of adolescent substance use (Family Matters; Bauman et al. 2001). The combined intervention blends and extends materials from the component programs, and is designed for families of depressed parents with children between the ages of 12–15 years, a developmental period characterized by increased risk for emotional and behavioral problems. The goal of Project Hope is to prevent adolescent depression and substance use, as well as their co-occurrence, by strengthening parenting and family relationships and enhancing youth resilience.
Prevalence and Consequences of Parental Depression
Depression among adults is common (Kessler et al. 2005), with past-year and lifetime prevalence rates of major depressive disorder in the United States of approximately 5 and 13%, respectively (Hasin et al. 2005). Many men and women who struggle with depression are parents or care-givers of children (Weissman et al. 2006). Children of depressed parents represent a vulnerable population, experiencing elevated risk for depression (Lieb et al. 2002) and a range of additional problems (Goodman and Gotlib 1999), including substance use (Weissman et al. 1997). An estimated 12% of adolescents in the United States meet criteria for major depressive disorder (Merikangas et al. 2010), of whom between 20 and 50% have a family history of depression (Kovacs et al. 1997). Although part of the risk for depression among children of depressed parents is genetic (Rice et al. 2002), modifiable features of the environment also play a role in the intergenerational transmission of depression (Weissman et al. 2006). For example, maternal and paternal depression are associated with parenting deficits, such as negative parent–child affective quality and disrupted family management practices (Downey and Coyne 1990), which are risk factors for adolescent depression (Ge et al. 1996). These parenting deficits are also risk factors for adolescent substance use (Brook et al. 1989). Thus, family interventions that improve the parenting skills of depressed parents may help prevent depression as well as substance use among children.
Etiology and Co-occurrence of Adolescent Depression and Substance Use
Depression and substance use tend to escalate during the teen years (Hankin et al. 1998; Johnston et al. 2010; Institute of Medicine and National Research Council 2011; O'Connell et al. 2009). Earlier depressive symptoms increase risk for later depression diagnoses (Pine et al. 1998), and depression is associated with decreased relationship quality and poor physical health (Fergusson and Woodward 2002). Likewise, substance use places teens at risk for the development of substance abuse and dependence (McGee et al. 2000) and impairs psychosocial functioning (Newcomb and Bentler 1988; Institute of Medicine and National Research Council 2011; O'Connell et al. 2009).
Adolescent depression and substance use often co-occur (Rohde et al. 1996). Several explanations for such cooccurrence have been proffered. Because depression and substance use share a number of risk factors (cf. Reinherz et al. 2000), common predictors, such as family conflict and peer rejection, may explain the link between these two outcomes. Alternatively, one behavior may causally influence the other. The self-medication hypothesis suggests that individuals use substances to alleviate the symptoms of their dysphoria (Khantzian 1985); however, findings in support of this hypothesis are mixed. Consistent with self-medication, some studies report predictive effects leading from depression indicators to substance use outcomes (Clark et al. 2011; Mason et al. 2009). Other studies report predictive effects leading from substance use indictors to depression outcomes (Brook et al. 2002; Hansell and White 1991), possibly due to the impairments that result from substance involvement (Newcomb and Bentler 1988). Contemporaneous and lagged bidirectional influences also have been reported (Audrain-McGovern et al. 2009; Windle and Windle 2001).
Prevention of Adolescent Depression and Substance Use
Prevention programs can capitalize on existing knowledge of the tendency for substance use and depression to co-occur among teens, even without a complete understanding of the nature of the association. Whether by addressing common psychosocial risk factors for depression and substance use or by interrupting a causal process linking the outcomes, effective programs that explicitly address these emotional and behavioral problems may reduce depression and substance use, and their co-occur-rence, among teens. There is strong evidence that parent and family prevention programs can prevent later problem behaviors such as substance use and depression, as well as improve family relationships through strengthening positive parenting behaviors (Bauman et al. 2002; Beardslee et al. 2003; Brody et al. 2009; Catalano et al. 2004; Haggerty et al. 2007; Spoth et al. 2004). Project Hope addresses depression and substance use as distinct but related outcomes by combining two independently developed, evidence-based family programs: Hope, Meaning, and Continuity and Family Matters.
Hope, Meaning, and Continuity is a clinician-facilitated, psychoeducational intervention for families in which one or both parents experience depression and in which there is at least one child between the ages of 8–15 years (Beardslee et al. 2003). A series of studies have compared Hope, Meaning, and Continuity to a reduced, lecture-based version of the program. Randomized trials have demonstrated that the clinician-based program resulted in significantly more attitude and behavior change than the lecture-based program. For example, Beardslee et al. (1993) found that clinician-facilitated participants displayed more feelings of understanding and emotional closeness from pre- to post-intervention than lecture participants. As expected, increased parent and child knowledge about depression and risk/resilience was observed across both conditions, with no group differences; however, clinician-based program participants showed significantly more adoption of new coping strategies from pre- to post-intervention than lecture-based participants. Beardslee et al. (1993) reported that, in addition to intervention effects on parent and child attitudes and behaviors, children in both conditions showed significant decreases in depressive symptoms. Significant decreases in internalizing symptoms among youth in both conditions were reported in Beardslee et al. (2003), with effects extending 2.5 years postintervention. To date, Hope, Meaning, and Continuity effects on depression diagnoses have been more limited; both conditions in the randomized trials have reported low rates of depression.
Family Matters is a health educator-facilitated, universal preventive intervention for families of youth between the ages of 12–14 years (Bauman et al. 2001). Findings from a randomized trial conducted with a nationally representative sample of 1,326 adolescents, aged 12–14 years, and their families have demonstrated Family Matters to be an efficacious program that reduces the prevalence of tobacco and alcohol use among teens (Bauman et al. 2001). For example, Bauman et al. (2002) showed that experimental group adolescents had a lower prevalence of cigarette smoking and alcohol consumption compared to control group adolescents at 3 months and 1 year after the program. Additional evidence has suggested that reductions in the prevalence of substance use were achieved by preventing substance use onset (Bauman et al. 2002), rather than by reducing the amount of substance use among baseline users (Bauman et al. 2000). Family Matters also has been associated with improvements in global (e.g., parent–child involvement) and substance-specific (e.g., setting rules about smoking and drinking) family characteristics targeted by the program (Ennett et al. 2001).
Development of Project Hope
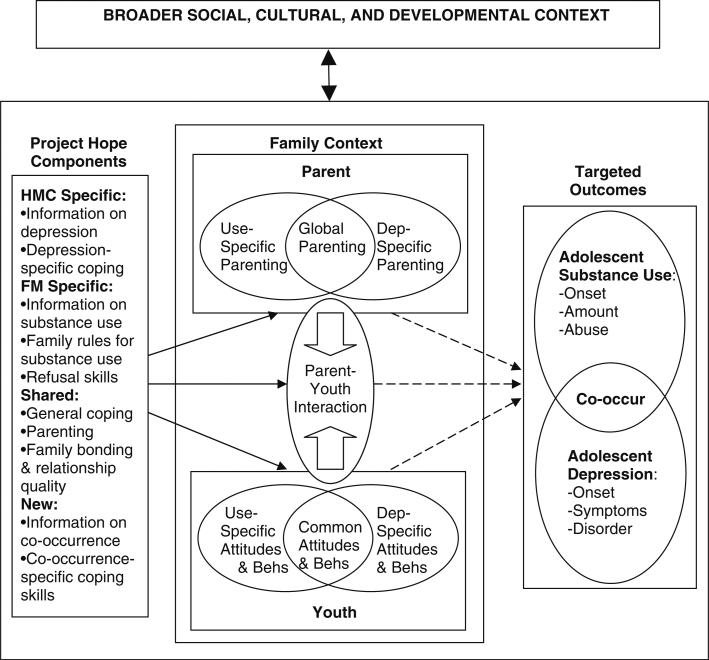
Project Hope blends and extends materials from Hope, Meaning, and Continuity and Family Matters, guided by an organizing framework that is grounded in both ecological systems theory (Bronfenbrenner 1979; Brook et al. 1989) and developmental psychopathology (Cicchetti and Rogosch 2002). Whereas ecological systems theory is concerned with multiple socializing influences and highlights the importance of family for youth development (Bronfenbrenner 1979), developmental psychopathology is concerned with understanding the origins and course of individual maladaptation and adaptation over the life span (Sroufe and Rutter 1984). The core components of Project Hope are illustrated in the leftmost rectangle of Fig. 1 (detailed program content is provided in the “Method” section). These components were selected from Hope, Meaning, and Continuity as well as Family Matters, and some were newly created to address a range of family-related risk and protective factors both common and specific to substance use and depression, as represented by the overlapping ovals within the “Parent” and “Youth” rectangles. Specifically, Project Hope targets outcomes related to the family depression experience (e.g., communication about depression), family interactions (e.g., family involvement, parent–child relationship quality, and reduced family conflict), family management (e.g., monitoring/supervision, rules, discipline), and individual functioning (e.g., coping skills, substance use refusal skills, knowledge and beliefs about adolescent depression and substance use).
Fig. 1.
Organizing framework for Project Hope. Note HMC hope, meaning, and continuity (Beardslee et al. 2003), FM family matters (Bauman et al. 2001), Dep depression, Behs behaviors
In essence, the ovals depicted within the “Family Context” rectangle represent hypothesized proximal effects of the program activities; these effects are depicted as solid, directional arrows. For example, teaching parents family management skills, such as how to reward desired behavior while redirecting inappropriate behavior in their children, is expected to reduce the use of inconsistent discipline, which is a risk factor for both depression and substance use among teens. Because there are complex pathways leading both toward and away from emotional and behavioral problems among at-risk youth, as highlighted by a developmental psychopathology framework (Cicchetti and Rogosch 2002), Project Hope seeks to reduce risk (e.g., conflict) as well as enhance protection (e.g., relationship quality) within the family context.
Overlapping ovals in the rightmost rectangle of Fig. 1 show that substance use and depression are distinct but related outcomes, which often co-occur among teens. As indicated by the dashed directional arrows, it is expected that reducing risk and enhancing protection among vulnerable youth will interrupt pathways leading toward depression, substance use, and the co-occurrence of these problems. Of course, a host of additional social, cultural, and developmental factors play a role in the etiology of adolescent depression and substance use, as suggested by ecological systems theory and illustrated by the uppermost rectangle in Fig. 1. Family intervention activities occur within a broader context that includes a complex system of influences on parents and youth. Factors such as school climate and peer socialization can have direct effects on the variables and processes specified in the large, lower rectangle. Alternatively, family intervention efforts may moderate effects from the broader context. For instance, improving parent–child relationship quality and decreasing family conflict may mitigate the effect of psychosocial risk factors, such as peer substance use, on adolescent substance use.
Hypotheses
The organizing framework in Fig. 1 conceptually illustrates hypothesized causal relations among intervention components, family-related risk and protective factors, and developmental outcomes. This represents “small intervention theory” (Lipsey 1990) applied to the case of integrating and extending two independently developed, empirically supported interventions that target distinct but related outcomes. Rather than test the full framework, the goals of this small randomized study were to develop Project Hope and test the feasibility and preliminary efficacy of the program. It was hypothesized that the intervention would decrease targeted proximal risk factors and increase targeted proximal protective factors related to improvements in the family depression experience, family interactions, family management, coping, (anti-) substance use beliefs, and refusal skills. Effects on primary outcomes, including reduced adolescent depression and substance use, also were examined, but these hypotheses were tempered due to the small sample size and short time frame of this preliminary study.
Method
Participants
Participants were parents screened for elevated depressive symptoms with an adolescent-aged child living in the home. Recruitment began in Fall 2008 via distribution of flyers in health care clinics and therapeutic centers in Seattle, WA. Due to a slow rate of recruitment contacts, expanded strategies included internet postings, magazine advertisements, targeted letters, parenting seminars, and school contacts and presentations. Over the course of a year, 51 families contacted the project either through internet postings (n = 13), schools (n = 12), clinics (n = 7), community ads (n = 7), friends (n = 5), or mail outs (n = 3); 4 contacts came from unknown sources. Five families never returned phone calls after their initial inquiry.
Of the 46 families screened, 16 were ineligible. Eligible families had a depressed parent who scored between 11 and 20 on the Quick Inventory of Depressive Symptoms-Self Report (QIDS-SR; Rush et al. 2010), where scores below 11 indicate having no or mild depression and scores above 20 indicate having very severe depression. Families also had a 12- to 15-year-old living in the home, but were excluded if youth had been diagnosed with or treated for depression or substance abuse. The 30 eligible families were pretested and randomly assigned to either Project Hope (n = 16) or a wait-list control condition (n = 14). Participating families were not aware of the experimental condition to which they had been assigned until after pretesting. Posttests were completed with 29 (Project Hope = 16; control = 13) families approximately 4 months after the pretest, and follow-up assessments were completed with 28 (Project Hope = 16; control = 12) families approximately 5 months after the posttest. Wait-list control families were invited to participate in Project Hope after the posttest assessment.
Sample characteristics and tests of baseline equivalence across conditions on sociodemographic variables are reported in Table 1. As a reflection of the study inclusion criteria, parents in both conditions reported a clinically elevated level of depressive symptoms; however, only about 20% of parents in the total sample reported receiving inpatient or outpatient treatment services. The large majority of participating parents were female, and slightly more than half were Caucasian. Approximately 20% of the parents reported an Hispanic ethnic background. Most parents reported having a spouse or partner (63% in the total sample; n = 19), although slightly more Project Hope than control participants were single. Most participating parents were either employed or unemployed but not looking for work. The average annual household income in the total sample was $58,968 (median = $46,800). The sample had slightly more adolescent male than female participants, with an average age of 13.9 years in the total sample. Most participating youth were in middle school. By adolescent report, the balance of Caucasian to minority/ multiracial youth participants was evenly split in the Project Hope condition and tipped slightly toward minority/ multiracial youth participants in the control condition. There were slightly fewer control adolescents who reported having an Hispanic ethnic background compared to Project Hope adolescents. None of the differences were large enough to be statistically significant in this small sample.
Table 1.
Baseline sociodemographic characteristics of the sample by experimental group
| Variable | Control (n = 14) |
Project Hope (n = 16) |
Baseline differences | ||
|---|---|---|---|---|---|
| M | SD | M | SD | ||
| Parent female gender | .93 | .27 | .88 | .34 | p = .63 |
| Parent minority/multiracial | .31 | .48 | .38 | .50 | p = .71 |
| Parent depressive symptoms | 30.79 | 9.01 | 32.31 | 8.48 | p = .64 |
| Parent treatment services | .29 | .47 | .13 | .34 | p = .27 |
| Parent Caucasian | .69 | .48 | .63 | .50 | p = .71 |
| Parent Hispanic | .23 | .44 | .19 | .40 | p = .78 |
| Parent single | .21 | .43 | .50 | .52 | p = .11 |
| Parent college graduate | .50 | .52 | .56 | .51 | p = .73 |
| Parent number of children | 2.29 | 1.14 | 2.38 | 1.20 | p = .96 |
| Parent unemployed-looking | .14 | .36 | .13 | .34 | p = .89 |
| Parent household income | 56,716.7 | 37,948.1 | 61,218.8 | 37,774.3 | p = .76 |
| Adolescent female gender | .43 | .51 | .44 | .51 | p = .96 |
| Adolescent age | 13.64 | 1.39 | 14.13 | 1.2 | p = .32 |
| Adolescent minority/multiracial | .64 | .50 | .50 | .52 | p = .43 |
| Adolescent Caucasian | .36 | .50 | .50 | .52 | p = .43 |
| Adolescent Hispanic | .08 | .28 | .31 | .48 | p = .12 |
| Adolescent grade 6, 7, or 8 | .86 | .36 | .69 | .48 | p = .27 |
| Adolescent grade 9 or 10 | .14 | .36 | .31 | .48 | p = .27 |
Intervention Development and Content
As noted, Project Hope was developed by blending and extending materials from two evidence-based preventive interventions. The Hope, Meaning, and Continuity program (Beardslee et al. 2003) seeks to (a) inform parents and children about depression and teach them new attitudes about the illness; (b) help parents understand risk and promote resilience in their children; (c) encourage parents and children to develop new skills for communicating in the family and for coping with adversity; and (d) promote self-understanding and reduce internalizing symptoms and depression among children. In six sessions, clinicians meet with either the parents, the target child, or the family. Family Matters (Bauman et al. 2001) seeks to reduce the prevalence of alcohol and tobacco use among teens by (a) enhancing family understanding of adolescent substance use and promoting family self-efficacy for influencing substance use attitudes and behaviors among youth, (b) improving general family management skills and family interactional dynamics, (c) developing family norms and rules against substance use, and (d) promoting substance use refusal skills and anti-substance use attitudes for effectively dealing with influences from peers and media. Families are mailed four booklets. Each booklet encourages participation in activities that reinforce the educational content and provides a forum in which to practice new skills. Two weeks after each booklet is mailed, a health educator contacts the family by telephone to check on progress, encourage completion of the activities, and answer questions.
These two programs bring several strengths to the development of Project Hope. For example, Hope, Meaning, and Continuity is sufficiently intensive for higher risk families, whereas Family Matters adopts a mode of administration that is readily adaptable. Both of these programs are fully manualized and have well-developed training and implementation protocols, and they include shared components as well as components unique to each program's targeted outcomes, as illustrated in Table 2.
Table 2.
Component programs of Project Hope
| Hope, Meaning, and Continuity | Family Matters | |
|---|---|---|
| Expected outcomes | Decreased youth depressive symptoms and disorder onset and severity | Decreased youth tobacco and alcohol onset and level of use |
| Target participants | Families of youth aged 8–15 years with one or more depressed parents | Families of youth aged 12–14 years |
| Shared components/mechanisms of change | Increased knowledge about role of parents in youth development Improved parent-youth communication |
Increased knowledge about role of parents in youth development Improved parent-youth communication |
| Increased youth coping skills | Increased youth coping skills | |
| Increased youth involvement in family and prosocial activities | Increased youth involvement in family and prosocial activities | |
| Decreased family conflict and increased family relationship quality | Decreased family conflict and increased family relationship quality | |
| Unique components/mechanisms of change | Increased parent and youth knowledge about depression and its effects on the family and development Increased recognition and treatment of youth symptoms of depression |
Increased parent and youth knowledge about substance use and its effects on the family and development Increased parental monitoring and supervision |
| Family experience linked to program material | Increased substance use rules and consequences in the family | |
| Increased youth substance-use refusal skills and prosocial beliefs | ||
| Implementation | Clinician-facilitated | Health educator-facilitated |
| Six sessions, involving: | Four booklets, involving: | |
| Parent/youth/family meetings | Family homework activities | |
| Telephone contacts | Telephone contacts |
Project Hope integrates Family Matters into the basic structure of Hope, Meaning, and Continuity. For example, rather than mail booklets for self-administered implementation with phone follow-up, Family Matters booklet materials were blended into the Hope, Meaning, and Continuity content and delivered in the homes of participating families. The Project Hope curriculum also extends materials of the component programs by, for example, including information about the tendency for depression and substance use to co-occur. The program is implemented over 10 sessions that are facilitated by trained masters-level clinicians with backgrounds in family intervention. The content of each session is briefly described in Table 3.
Table 3.
Summary of Project Hope session content
| Session | Attendees (duration) | Selected goals |
|---|---|---|
| Week 1: Introduction and sharing stories | Parents and youth (90 min) | Introduce the intervention |
| Obtain a family history of depression | ||
| Set goals for the intervention | ||
| Week 2: Youth risk and resilience | Parents and youth (90 min) | Present information about depression, substance use, and their co-occurrence |
| Review youth's current functioning | ||
| Help families plan special times together and promote positive family interactions | ||
| Present information about youth resiliency | ||
| Week 3: From the adolescent's perspective | Youth alone (60 min) | Develop rapport and determine functioning |
| Increase awareness of emotions and coping | ||
| Teach strategies for coping with problems | ||
| Week 4: Strengthening communication skills | Parents alone (60 min) | Provide an overview of adolescent development |
| Review and practice skills for improving communication and reducing family conflict | ||
| Week 5: Preparing for the family meeting-depression | Parents alone (90 min) | Prepare parents to conduct family meeting Link parents’ perception of depression with that of the youth's experience of their depression |
| Week 6: Family meeting-depression | Entire family (60 min) | Facilitate a shared understanding of depression |
| Help family members relate general information about depression to their specific experience | ||
| Week 7: Preparing for the family meeting-adolescent substance use | Parents alone (60 min) | Prepare parents to conduct family meeting Help parents to establish clear rules and consequences about youth substance use |
| Week 8: Family meeting-adolescent substance use | Entire family (60 min) | Help parents share substance use rules Help youth understand consequences of substance use |
| Week 9: Outside influences and resources | Parents and youth (75 min) | Inform parents about contextual influences, primarily with regard to peers and media |
| Teach methods to promote positive influences | ||
| Week 10: Review and hope for the future | Entire family (50 min) | Review previous sessions |
| Help families map out post-intervention goals | ||
| Recognize and celebrate the family's progress |
Intervention Exposure and Implementation
Overall, 24 of the 30 enrolled families participated in Project Hope, including 15 intervention and 9 wait-list control families. Of those 24 families, 21 completed all 10 sessions, including 13 intervention and 8 wait-list control families. One intervention family dropped out of the study prior to beginning Project Hope, and two received only a partial dose of the intervention (1 session or 4 sessions). Fewer wait-list control families participated in Project Hope because they were given the option of either completing the standard in-home program or receiving a take-home version of the program for their reference, without any staff follow-up.
Ratings of adherence to the key components of Project Hope were obtained via reports from clinical intervention specialists at the conclusion of each session using fidelity checklists. These ratings indicated that, across all sessions, greater than 90% of the key components were implemented. Ratings of the quality of program implementation in the domains of organization, enthusiasm, clarity, and responsiveness also were obtained from clinicians. These ratings were generally high. For example, on a scale ranging from 0 (minimal) to 3 (exceptional), clinicians rated their Session 2 program implementation as follows: organization (M = 1.75; SD = .50), enthusiasm (M = 2.25, SD = .50), clarity (M = 2.0, SD = .82), and responsiveness (M = 2.25, SD = .50). Keeping in mind the self-report nature of the ratings, this suggests that program implementation was acceptable.
Procedure
Families were recruited on a rolling basis beginning in Fall 2008. After obtaining parent consent and adolescent assent among participating families, parent and adolescent pre-tests were conducted separately via telephone interview. All participants were assured of the confidentiality of their responses. Each interview took approximately 30–45 min to complete. Each parent received $15 and each adolescent received $10 as compensation for their time in completing the survey. Identical procedures were used to conduct the posttest and follow-up assessments. All study procedures were approved by the Human Subjects review committee at the University of Washington.
Measures
Family Depression Experience
Six parent-report items adapted from the Semi-structured Interview about the Intervention (SII; Beardslee et al. 1997) were used to measure the family depression experience. Parents reported how comfortable they are sharing about their depression with others. Parents also were asked to indicate both the frequency and perceived helpfulness of talking with their spouses and (separately) their children about depression. Finally, parents reported how much they think that their depression has affected their children. Response options for these items ranged from 1 “Not at all” to 5 “A great deal,” except for the two frequency of talking items, which used a scale ranging from 1 “Daily” to 6 “Never.”
Family Interactions
Parent–child relationship quality was measured with a six-item scale drawn from the Project Family prevention trial (Spoth et al. 1998). Parents indicated, for example, how often they got angry with their child, let their child know they care, and acted loving and affectionate toward their child during interactions over the past month. Adolescents answered a parallel set of items in reference to their mom and (separately) dad; items were summed to compute an overall parent–child relationship quality scale, unless only one parent was present, in which case the score for that particular parent was used. Response options ranged from 1 “Always” to 5 “Never,” and items were coded and summed to compute a scale representing positive parent–child relationship quality. Alpha reliability across the assessments ranged from .78 to .84 for parent report and .73 to .90 for adolescent report.
Family conflict was measured with a three-item parent-report scale from Project Family. Parents reported how often during an average week they had had serious arguments, repeatedly discussed the same problems without finding a solution, and figured out a way to deal with problems during interactions with their child (reverse coded). Response options ranged from 1 “Always” to 5 “Never,” and items were coded and summed to compute a scale representing high family conflict. Alpha reliability across the assessments ranged from .70 to .82.
Adolescent-reported parent involvement was measured with nine items from the short-form Alabama Parenting Questionnaire (APQ; Shelton et al. 1996). Sample items include “You had a friendly talk with your mom...how about your dad?” and “Your mom asked about your school day...how about your dad?” Response options ranged from 1 “Never” to 5 “Always.” Separate scales in reference to each adolescent's mom and dad were computed and then summed into a parental involvement scale. If the adolescent had only one parent, then the scores in reference to a single parent were used. Across the assessments, alpha reliability for the parent involvement scale ranged from .79 to .86.
Family Management
The nine-item short form of the APQ was used to measure positive parenting (3 items; e.g., “You let your child know when he/she is doing a good job with something”), inconsistent discipline (3 items; e.g., “You threaten to punish your child and then do not actually punish him/her”), and poor supervision (3 items; e.g., “Your child is out with friends you don't know”). Both parents and adolescents responded to these questions on a scale ranging from 1 “Always” to 5 “Never.” Across the assessments, average alpha reliability for each scale was as follows: Positive Parenting (parent = .85; adolescent = .79), Inconsistent Discipline (parent = .43; adolescent = .44), and Poor Supervision (parent = .77; adolescent = .54).
Substance Use Rules
Three items from Project Family asked parents to indicate the degree to which they agree that they have explained the consequences of not following their rules about alcohol, tobacco, and marijuana use. Response options ranged from 1 “Strongly agree” to 5 “Strongly disagree,” and items were reverse coded and summed to compute a substance use consequences scale. Across the assessments, alpha reliability ranged from .82 to .93.
Coping Skills
Intervention-targeted parent coping skills were measured with nine two-item scales from the COPE Inventory (Carver 1997). Scales included active coping, denial (reverse coded), emotional support, instrumental support, blame (reverse coded), disengagement (reverse coded), reframing, planning, and turning to drug use (reverse coded). Response options ranged from 1 “I haven't been doing this at all” to 4 “I have been doing this a lot.” The nine scale scores were summed to compute an overall coping scale. Across the assessments, alpha reliability ranged from .66 to .81. Adolescent coping skills were measured with the Active Coping scale of the Children's Coping Strategies Checklist-Revision 1 (Ayers et al. 1996). Asked to think about how they solved recently experienced problems, adolescents responded to questions such as “You did something to make things better” and “You told yourself that things would get better” on a scale ranging from 1 “Never” to 4 “Most of the time.” Items were summed to compute a coping skills scale, with alpha reliability ranging from .93 to .96 across assessments.
Substance Use Beliefs
Substance use beliefs were measured with a three-item scale from Project Family. Items asked adolescents to indicate how much they think it hurts people to take one or two drinks a day, smoke cigarettes regularly, and smoke marijuana occasionally. Response options ranged from 1 “Not at all” to 4 “Hurts a great deal.” Items were averaged into a substance use beliefs scale. Across the assessments, alpha reliability ranged from .58 to .69.
Substance Use Refusal Skills
Intervention-targeted substance use refusal skills were measured by two items from Project Family. Adolescents were asked to consider a hypothetical offer to drink alcohol at a party and indicate how likely they would say why it would be wrong and suggest something else to do. Response options ranged from 1 “Very likely” to 5 “Very unlikely.” Each item was reverse coded to indicate a higher likelihood of using the skill. Across the assessments, alpha reliability ranged from .70 to .78.
Depression
Parent depression was measured by parent report with the 20-item Center for Epidemiological Studies Depression Scale (CES-D; Radoloff 1977). Across the assessments, alpha reliability ranged from .82 to .90. Adolescent depression was measured by adolescent report using the 33-item Mood and Feelings Questionnaire (MFQ; Angold et al. 1995). Adolescents were asked to respond how true each statement was in regard to how they've been feeling lately, with response options ranging from 0 “Not true” to 3 “True.” Sample items include “You felt miserable or unhappy” and “You hated yourself.” Items were summed to compute a depressive symptoms scale. Across the assessments, alpha reliability ranged from .90 to .95.
Adolescent Substance Use
Standard items were used to measure whether adolescents had ever used alcohol, cigarettes, or marijuana, and whether they had ever misused prescription drugs. The past-month frequency of use for each of these substances also was measured. The overall frequency of substance use was very low; thus, the lifetime measures were used to compute an index representing a count of the number of substances adolescents had used at the time of each assessment. Across the assessments, alpha reliability ranged from .76 to .78. Finally, since alcohol is the most commonly used substance among teens (Johnston et al. 2010), adolescents were asked to further indicate their typical quantity of alcohol consumption on a scale ranging from 0 “I don't drink alcohol” to 5 “More than 6 drinks.”
Covariates
Covariates for parent-report data analyses included parent gender (coded 1 for female and 0 for male) and parent educational attainment (coded 1 for college degree and 0 for less than college). Covariates for adolescent-report data analyses included adolescent gender (coded 1 for female and 0 for male) and adolescent grade.
Data Analyses
The data were analyzed with a series of 2 (Group) × 3 (Time) analyses of covariance. Analyses were conducted with SPSS Version 15. The assumption of sphericity was tested using Mauchly's test of sphericity. For analyses in which this assumption was violated, Huynh–Feldt adjusted degrees of freedom values were used to determine the statistical significance of the overall F test. Follow-up tests of within-subjects contrasts were conducted, focusing on group differences from pretest to posttest, prior to wait-list intervention. To preserve the integrity of the randomized design, an intent-to-treat strategy was adopted in which all participants were included in the analyses based on their original random assignment to conditions rather than according to their degree of engagement in Project Hope.
Results
Parent-Report Data
ANCOVA results for parent-reported proximal targets related to the family depression experience, family interactions, family management, and parental coping are reported in Table 4. Tests of baseline equivalence across these outcomes revealed only one statistically significant difference: control participants were significantly less likely to report finding it helpful to talk with their spouses about depression at pretest than Project Hope participants (p = .001). Regarding measures of the family depression experience, statistically significant results were obtained for three outcomes. Tests of within-subjects contrasts focusing on group differences from pretest to posttest showed greater increases among Project Hope compared to control participants in feeling comfortable sharing information about depression, F (1,24) = 3.5, p = .073, and finding it helpful to talk with their children about depression, F (1,20) = 6.4, p = .02. Unexpectedly, results showed greater increases among control compared to Project Hope parents in the frequency of talking with a spouse about depression, F (1,11) = 4.9, p = .049.
Table 4.
Means (standard deviations) and ANCOVA results for parent-reported proximal targets
| Outcome (control n/intervention n) | Pretest |
Posttest |
Follow-up |
Group × time F (df; p) | |||
|---|---|---|---|---|---|---|---|
| Control | Intervention | Control | Intervention | Control | Intervention | ||
| Comfortable sharing (12/16) | 2.2 (.72) | 2.2 (.98) | 2.1 (1.1) | 2.6 (1.2) | 1.8 (.83) | 2.9 (1.1) | 6.4 (2,48; p = .004) |
| Talked with spouse (7/8) | 3.6 (1.5) | 3.8 (1.6) | 4.9 (1.1) | 3.4 (1.4) | 5.1 (1.1) | 3.8 (.71) | 4.0 (2,22; p = .032) |
| Helpful to talk w/spouse (6/8) | 2.2 (.98) | 4.3 (1.0) | 3.0 (1.3) | 3.6 (1.1) | 2.7 (1.0) | 3.5 (1.2) | 2.4 (2,20; p = .120) |
| Talked with children (12/16) | 5.3 (1.3) | 4.9 (1.3) | 5.3 (.78) | 4.4 (1.3) | 4.9 (1.1) | 4.6 (1.4) | .67 (2,48; p = .515) |
| Helpful to talk w/children (10/14) | 2.4 (1.5) | 2.2 (1.5) | 1.8 (.79) | 2.9 (1.4) | 2.1 (1.2) | 2.9 (1.5) | 3.6 (2,40; p = .037) |
| Depression affect children (12/15) | 3.9 (1.0) | 3.5 (.92) | 3.0 (1.1) | 2.5 (.92) | 2.8 (1.3) | 2.3 (.72) | .01 (2,46; p = .989) |
| Relationship quality (11/16) | 3.6 (.51) | 3.8 (.75) | 3.6 (.42) | 4.2 (.55) | 3.8 (.53) | 4.1 (.57) | 2.5 (2,46; p = .096) |
| Family conflict (11/16) | 3.1 (.78) | 2.9 (.83) | 3.1 (.73) | 2.4 (.89) | 2.8 (.85) | 2.4 (.86) | 2.4 (2,46; p = .102) |
| Positive parenting (11/16) | 4.1 (.75) | 4.2 (.59) | 4.2 (.56) | 4.3 (.52) | 4.0 (.48) | 4.2 (.53) | .17 (2,46; p = .843) |
| Inconsistent discipline (11/16) | 2.7 (.60) | 2.7 (.59) | 2.6 (.73) | 2.3 (.55) | 2.5 (.67) | 2.5 (.48) | 1.5 (2,46; p = .240) |
| Poor supervision (11/16) | 1.8 (.67) | 1.9 (.90) | 1.9 (.75) | 1.6 (.58) | 1.8 (.67) | 1.6 (.53) | 3.5 (2,46; p = .040) |
| Explained consequences (11/16) | 3.5 (1.4) | 3.6 (1.3) | 3.9 (1.5) | 4.5 (.70) | 4.6 (.67) | 4.4 (.70) | 1.6 (2,46; p = .208) |
| Coping skills (12/16) | 2.8 (.45) | 2.7 (.40) | 2.8 (.48) | 3.1 (.49) | 3.1 (.34) | 3.0 (.41) | 4.4 (2,48; p = .018) |
Regarding measures of family interactions, ANCOVA results showed a trend toward group differences in parent– child relationship quality, with some evidence for greater increases among Project Hope compared to control participants from pretest to posttest, F (1,23) = 3.4, p = .08. Regarding measures of family management, one of the three APQ scales showed a statistically significant difference, with results indicating that Project Hope compared to control parents reported greater decreases in poor supervision from pretest to posttest, F (1,23) = 8.4, p = .008. Finally, results indicated statistically significant group differences in coping, with greater increases from pretest to posttest among Project Hope compared to control parents, F (1,24) = 6.4, p = .018.
Adolescent-Report Data
ANCOVA results for adolescent-reported proximal targets related to family interactions, family management, substance use beliefs, refusal skills, and adolescent coping as well as depression and substance use primary outcomes are reported in Table 5. Tests of baseline equivalence revealed no statistically significant group differences. Overall, there were few statistically significant intervention effects based on the adolescent data. Results did reveal statistically significant group differences for alcohol quantity. Whereas control adolescents experienced an increase in alcohol quantity from pretest to posttest, Project Hope adolescents experienced a slight decline over this time frame, F (1,21) = 6.5, p = .019. Note that adolescents in the intervention condition were somewhat elevated on alcohol quantity at pretest; thus, their decrease in alcohol quantity, although contrasting with the increase for control teens, resulted in comparable mean scores across conditions at posttest. Unexpectedly, there was a trend for control compared to Project Hope adolescents to report increases in coping, prior to receiving the delayed intervention (see Table 5).
Table 5.
Means (standard deviations) and ANCOVA results for adolescent-reported proximal targets, depression, and substance use
| Outcome (control n/intervention n) | Pretest |
Posttest |
Follow-up |
Group × Time F (df; p) | |||
|---|---|---|---|---|---|---|---|
| Control | Intervention | Control | Intervention | Control | Intervention | ||
| Parent involvement (12/14) | 3.31 (.50) | 3.35 (.70) | 3.39 (.61) | 3.35 (.69) | 3.20 (.54) | 3.14 (.66) | .17 (2,44; p = .845) |
| Relationship quality (12/14) | 3.74 (.43) | 3.73 (.78) | 3.74 (.79) | 3.80 (.86) | 3.80 (.54) | 3.83 (.73) | .25 (2,44; p = .780) |
| Positive parenting (11/14) | 3.94 (.42) | 3.60 (.99) | 3.94 (.71) | 3.43 (1.07) | 3.58 (1.02) | 3.52 (1.24) | .99 (2,42; p = .381) |
| Inconsistent discipline (11/14) | 2.09 (.70) | 2.33 (.63) | 2.52 (.69) | 2.17 (.68) | 2.36 (.94) | 2.31 (.73) | 1.67 (1.9,33.2; p = .201)1 |
| Poor supervision (12/13) | 1.83 (.95) | 1.90 (.53) | 2.01 (1.01) | 1.68 (.56) | 2.06 (.86) | 1.92 (.72) | .91 (2,42; p = .411) |
| Substance use beliefs (10/14) | 3.64 (.39) | 3.24 (.70) | 3.53 (.46) | 3.36 (.62) | 3.47 (.56) | 3.21 (.67) | .45 (2,44; p = .642) |
| Refusal-why wrong (12/14) | 2.58 (1.56) | 2.64 (1.60) | 3.25 (1.66) | 2.71 (1.33) | 2.75 (1.60) | 2.29 (1.07) | .48 (2,44; p = .625) |
| Refusal-suggest (11/14) | 3.73 (1.35) | 3.14 (1.61) | 3.36 (1.21) | 3.43 (.94) | 3.45 (1.04) | 3.14 (1.23) | .57 (2,42; p = .571) |
| Coping (11/13) | 61.2 (14.2) | 67.7 (14.9) | 65.7 (14.9) | 62.7 (12.5) | 61.3 (18.2) | 64.9 (14.3) | 2.82 (1.7,35.2; p = .079)1 |
| Depressive symptoms (11/13) | 11.91 (.86) | 12.1 (11.1) | 8.73 (9.90) | 8.31 (6.88) | 7.55 (11.52) | 10.3 (10.1) | .63 (2.40; p = .539) |
| Substance use count (12/14) | .42 (.79) | .79 (1.31) | .58 (.90) | .86 (1.29) | .75 (1.06) | 1.00 (1.41) | .45 (2,44; p = .641) |
| Alcohol use quantity (12/13) | .25 (.45) | 1.08 (1.66) | .75 (1.29) | .77 (1.24) | .83 (1.27) | 1.15 (1.77) | 3.24 (2,42; p = .049) |
Huyn-Feldt degrees of freedom under violation of the sphericity assumption
Discussion
Given the high prevalence and costs of adolescent depression and substance use, and the tendency for these outcomes to co-occur among youth, prevention efforts are needed. The current article introduced Project Hope, a family intervention for depressed parents of adolescent-aged children. The program was created by blending empirically supported prevention programs targeting adolescent depression (Beardslee et al. 2003) and substance use (Bauman et al. 2001). The goal of Project Hope is to prevent these adolescent problem outcomes, and their co-occurrence, by strengthening parenting and family relationships and enhancing resilience among youth. Findings from this preliminary randomized evaluation, although qualified by the small size and scope of the study, provide some evidence for hypothesized intervention effects on measures of targeted constructs related to improvements in the family depression experience, family management, coping, and reduced adolescent alcohol use, with a trend toward improved family interactions.
Feasibility of Project Hope Implementation
Before discussing the outcome findings in more detail, we note that data regarding recruitment and intervention engagement in this study provide valuable information as to the feasibility of implementing Project Hope with targeted families. Overall, recruitment unfolded slowly over the course of the study. Certain symptoms of depression, such as anhedonia and inactivity, make it particularly challenging to motivate depressed parents to participate in family intervention services and research (Grote et al. 2007). Due to the small size of this pilot trial, our recruitment efforts were limited almost exclusively to passive advertising strategies. Future studies are needed to evaluate the effectiveness of more active recruitment strategies, such as working with mental health and primary care providers to obtain direct referrals to Project Hope. Rates of engagement in the intervention once families were enrolled into the study were relatively high, particularly in comparison with engagement rates reported in family interventions that are implemented via a group-based, parenting workshop format (Spoth et al. 2007). In-home family interventions, such as Project Hope, may help to reduce some of the barriers to participation (e.g., scheduling conflicts, lack of transportation and child care) that are known to exist for parenting classes (Haggerty et al. 2006; Spoth et al. 1996). This must be weighed against the increased cost and intensity of such interventions relative to parenting classes, although increased efforts likely are needed when working with at-risk families and youth. Indeed, although the home-based approach adds cost to program implementation, this has been an important component for effective programs with high-risk families (e.g., Olds et al. 2007). Further research is needed to enhance our understanding of how to more fully engage families in home-based programs. Still, a more targeted, in-home intervention approach for at-risk families can provide effective services for those whose needs are not fully met by brief, universal public health intervention strategies and, therefore, represents an important part of the spectrum of care (O'Connell et al. 2009).
As another feasibility consideration, there was some evidence to indicate that the implementation fidelity of Project Hope was high. However, reports of adherence to the program were obtained from clinicians themselves. Although such reports have been used successfully in prior studies (Breitenstein et al. 2010), they may increase the likelihood of biased responding. The small scope of this pilot trial precluded conducting expanded assessments of the multiple dimensions of implementation fidelity (Dane and Schneider 1998). Future studies should incorporate additional methods, such as observational coding of videotaped family sessions and independent expert ratings of program quality, to ensure more reliable and complete measurement of implementation fidelity.
Parent-Reported Outcome Findings
Family interventions that result from the integration of existing prevention programs should be subjected to the same rigorous standards of evidence to which all programs are subjected, ideally being tested through randomized controlled trials. It cannot be assumed that a blended intervention will be effective merely because the component programs are empirically supported. As a first step toward this end, the current study provided a preliminary pilot test of Project Hope.
Drawing from Hope, Meaning, and Continuity (Beardslee et al. 2003), a key goal of Project Hope is to equip families to understand and manage the impact of parental depression on the family. Analyses examining changes in the family depression experience indicated that intervention parents reported increased comfort in sharing about their depression with others and finding it helpful to talk with their children about depression compared to wait-list control parents. Other targeted indicators of the family depression experience, such as the frequency of talking with children about depression, showed no intervention group differences over time. Unexpectedly, control parents reported an increased frequency of talking with their spouses (or partners) about depression, prior to receiving the delayed intervention. One explanation for this finding is that parents likely enrolled in the study when they were ready and willing to discuss their depression experience. Whereas intervention parents were provided with an outlet for doing so through a Project Hope intervention specialist, control parents were provided with no such outlet until later in the study and may have turned, instead, to their spouses in the short term. However, without additional skills, control parents did not appear to find such discussions more helpful.
Drawing from Family Matters (Bauman et al. 2001) and targeting a key risk factor for adolescent substance use (Hawkins et al. 1992), Project Hope seeks to increase parents’ skills for monitoring and supervising their adolescent-aged children in developmentally appropriate ways (see Tables 2, 3). Analyses of the parenting measures indicated that Project Hope parents reported a significantly greater decrease in poor supervision than control parents from pretest to posttest. Inconsistent discipline also is a key risk factor for the targeted problem behaviors (Hawkins et al. 1992). Although inconsistent discipline scores decreased over time for intervention parents, the group difference was not statistically significant. Similarly, no gains were shown for positive parenting, which may represent a more general and stable parenting characteristic that is relatively established by the time children reach adolescence.
There was only a trend toward improved parent–child relationship quality among Project Hope compared to control participants. Group differences on reductions in family conflict were in the expected direction, but were statistically nonsignificant. Results did show, however, a statistically significant increase in coping skills among Project Hope compared to control parents. Family interaction patterns likely are fairly established by the time children in the household reach adolescence. Still, family interventions (Spoth et al. 1998), including the component programs of Project Hope, have been shown to improve parent–child relationship quality and reduce family conflict. It is possible that the effect sizes on these more established outcomes are smaller than more malleable outcomes, resulting in an underpowered test in this small study. It is also possible that larger improvements in family interactions may require additional time to be realized. For example, short-term improvements in coping skills may lead, in turn, to reduced conflict and improved relationship quality as those skills are reinforced and become crystallized over time through a series of family interactions. Longer term studies of Project Hope with repeated assessments are needed to test this type of mediational hypothesis.
Adolescent-Reported Outcome Findings
Interestingly, far fewer statistically significant differences were observed when examining adolescent-reported outcomes. Although Project Hope is a family intervention (including parents, children, and other relevant family members), the program is weighted more heavily toward a parent-training focus. A key hypothesis of many such programs is that improvements in parenting will lead, in turn, to improvements in adolescent behaviors over time (Forehand and McMahon 1981; Kazdin 1997). For this reason, certain intervention effects on targeted adolescent outcomes may take more time to emerge than those for targeted parent outcomes. It is also possible that either parents or adolescents have a reporting bias that can operate either for or against conclusions about causal effects of the intervention. In particular, parental psycho-pathology may influence responding (Hennigan et al. 2006) and adolescents may underreport problem behaviors, such as substance use (Delaney-Black et al. 2010). Future studies of Project Hope should incorporate multi-rater, multi-method assessments of key constructs, which would permit structural equation modeling analyses that adjust for potential biases attributable to any particular rater or method (Cook and Goldstein 1993).
Among the targeted proximal adolescent outcomes, there was an unexpected tendency for control participants to report increases and intervention participants to report decreases in coping skills from pretest to posttest. It is possible that intervention participants, in the course of struggling to learn new skills, actually felt less competent after the intervention than before. Over time, some of those adolescents would be expected to become more adept with the new skills through repeated use, which might result in a rebound of self-reported skills ratings. Indeed, the average coping score increased for intervention adolescents from posttest to follow-up, although this difference did not reach statistical significance (results available on request).
Levels of adolescent depression and substance use were low, as were rates of co-occurrence, in this small sample. Low rates of emotional and behavioral problems likely are due to the relatively young age of participating adolescents, since both depression and substance use tend to increase over the teen years. A challenge for prevention studies is to incorporate a long enough follow-up period during which the targeted behaviors of interest are expected to emerge. Such follow-up was beyond the scope of this preliminary trial. Still, results showed statistically significant reductions in the reported quantity of alcohol use among Project Hope compared to control adolescents. This finding is consistent with effects of Family Matters on reduced adolescent drinking prevalence (Bauman et al. 2002), but is qualified by the fact that alcohol quantity was somewhat higher among intervention compared to control teens at pretest.
Limitations and Future Research
Limitations of this study include the small sample size and the non-probability sampling strategy. Statistical tests likely were somewhat underpowered, and questions remain about how representative enrolled families are to the broader population of depressed parents of adolescent-aged children in community settings. As noted above, the short-term follow-up period of the study is a limitation. To document prevention effects, long-term follow-up is needed. At this early stage of research, we sought to isolate potential intervention effects, whether in anticipated or unanticipated directions, by conducting a number of ANCOVAs on targeted outcomes without adjustment for the family-wise error rate. Finally, certain measures were brief and displayed lower than desired alpha reliability (e.g., inconsistent discipline from the short-form APQ). Brief scales were used to reduce the assessment burden on participants in this small trial; however, larger trials in the future should consider the use of expanded assessments with higher reliability. Although the validity of some of the brief scales is unknown, all measures were drawn from existing large-scale randomized prevention trials and have been used in prior analyses (e.g., Project Family; Spoth et al. 1998).
These limitations are important in suggesting future avenues of research for Project Hope. As suggested above, next steps should involve studies that include expanded assessments based on multiple raters (e.g., mothers, fathers, siblings, and youth) and methods (e.g., questionnaires, observations). Moreover, probability sampling is needed to ensure adequate representation of the targeted population, and longer term follow-up will permit tests of intervention effects that may take time to emerge. Future randomized trials also could compare the Project Hope condition to either Hope, Meaning, and Continuity-only or Family Matters-only conditions, to determine the degree to which the combined program brings added value to the component interventions. Further program development also may be needed. For example, more intensive intervention with participating youth, themselves, may need to be incorporated into Project Hope. Given the early stage of research on Project Hope, qualitative data collected from participants also would be valuable to obtain.
Summary and Conclusion
Project Hope was developed by blending and extending two existing, evidence-based, family interventions. The program was manualized and implemented with a relatively high degree of engagement with a small sample of targeted families and youth. Preliminary findings from this randomized pilot trial are qualified by the small size and scope of the study, but suggest important avenues for future research in the further development and evaluation of an intervention designed to prevent adolescent depression and substance use, and their co-occurrence, among families struggling with parental depression.
Acknowledgments
The project described was supported by grant # 5R21DA023687-02 from the National Institute on Drug Abuse (NIDA). The content is solely the responsibility of the authors and does not necessarily reflect the official views of NIDA. The authors would like to thank Drs. William R. Beardslee and Karl E. Bauman for their valuable contributions to the project.
Contributor Information
W. Alex Mason, National Research Institute for Child and Family Studies, Boys Town, NE 68010, USA masonwa@boystown.org.
Kevin P. Haggerty, Social Development Research Group, University of Washington, Seattle, WA 98195, USA
Andrew P. Fleming, Department of Psychology, University of Washington, Seattle, WA 98195, USA
Mary Casey-Goldstein, Social Development Research Group, University of Washington, Seattle, WA 98195, USA.
References
- Angold A, Costello EJ, Messer SC, Pickles A, Winder F, Silver D. The development of a short questionnaire for use in epidemiological studies of depression in children and adolescents. International Journal of Methods in Psychiatric Research. 1995;5:237–249. [Google Scholar]
- Audrain-McGovern J, Rodriquez D, Kassel JD. Adolescent smoking and depression: Evidence for self-medication and peer smoking mediation. Addiction. 2009;104(10):1743–1756. doi: 10.1111/j.1360-0443.2009.02617.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ayers TS, Sandler IN, West SG, Roosa MW. A dispositional and situational assessment of children's coping: Testing alternative models of coping. Journal of Personality. 1996;64:923–958. doi: 10.1111/j.1467-6494.1996.tb00949.x. [DOI] [PubMed] [Google Scholar]
- Bauman KE, Ennett ST, Foshee VA, Pemberton M, King TS, Koch GG. Influence of a family-directed program on adolescent cigarette and alcohol cessation. Prevention Science. 2000;1:227–237. doi: 10.1023/a:1026503313188. [DOI] [PubMed] [Google Scholar]
- Bauman KE, Ennett ST, Foshee VA, Pemberton M, King TS, Koch GG. Influence of a family program on adolescent smoking and drinking prevalence. Prevention Science. 2002;3:35–42. doi: 10.1023/a:1014619325968. [DOI] [PubMed] [Google Scholar]
- Bauman KE, Foshee VA, Ennett ST, Pemberton M. Family Matters: A family-directed program designed to prevent adolescent tobacco and alcohol use. Health Promotion and Practice. 2001;2:81–96. [Google Scholar]
- Beardslee WR, Gladston TRG, Wright EJ, Cooper AB. A family-based approach to the prevention of depressive symptoms in children at risk: Evidence of parental change and child change. Pediatrics. 2003;112:119–131. doi: 10.1542/peds.112.2.e119. [DOI] [PubMed] [Google Scholar]
- Beardslee WR, Salt P, Porterfield K, Rothberg PC, van de Velde P, Swatling S. Comparison of preventive interventions for families with parental affective disorder. Journal of the American Academy of Child and Adolescent Psychiatry. 1993;32:254–264. doi: 10.1097/00004583-199303000-00004. [DOI] [PubMed] [Google Scholar]
- Beardslee WR, Versage EM, Wright EJ, Salt P, Rothberg PC, Drezner K, et al. Examination of preventive interventions for families with depression: Evidence of change. Development and Psychopathology. 1997;9:109–130. doi: 10.1017/s0954579497001090. [DOI] [PubMed] [Google Scholar]
- Biglan A, Foster SL, Brennan PA, Holder HD. Helping adolescents at risk: Prevention of multiple problem behaviors. Guilford Press; New York: 2004. [Google Scholar]
- Breitenstein SM, Gross D, Garvey CA, Hill C, Fogg L, Resnick B. Implementation fidelity in community-based interventions. Research in Nursing and Health. 2010;33(2):164–173. doi: 10.1002/nur.20373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brody GH, Beach SRH, Philibert RA, Chen Y, Lei M-K, Murray VM, et al. Parenting moderates a genetic vulnerability factor in longitudinal increases in youths’ substance use. Journal of Consulting and Clinical Psychology. 2009;77(1):1–11. doi: 10.1037/a0012996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bronfenbrenner U. The ecology of human development: Experiments by nature and design. Harvard University Press; Cambridge, MA: 1979. [Google Scholar]
- Brook DW, Brook JS, Zhang C, Cohen P, Whiteman M. Drug use and the risk of major depressive disorder, alcohol dependence, and substance use disorders. Archives of General Psychiatry. 2002;59(11):1039–1044. doi: 10.1001/archpsyc.59.11.1039. [DOI] [PubMed] [Google Scholar]
- Brook JS, Nomura C, Cohen P. A network of influences on adolescent drug involvement: Neighborhood, school, peer, and family. Genetic, Social and General Psychology Monographs. 1989;115:125–145. [PubMed] [Google Scholar]
- Carver CS. You want to measure coping but your protocol's too long: Consider the Brief COPE. International Journal of Behavioral Medicine. 1997;4:92–100. doi: 10.1207/s15327558ijbm0401_6. [DOI] [PubMed] [Google Scholar]
- Catalano RF, Berglund ML, Ryan MAM, Lonczak HS, Hawkins JD. Positive youth development in the United States: Research findings on evaluations of positive youth development programs. Annals of the American Academy of Political and Social Science. 2004;591:98–124. [Google Scholar]
- Cicchetti D, Rogosch FA. A developmental psychopathology perspective on adolescence. Journal of Consulting and Clinical Psychology. 2002;70:6–20. doi: 10.1037//0022-006x.70.1.6. [DOI] [PubMed] [Google Scholar]
- Clark HK, Ringwalt CL, Shamblen SR. Predicting adolescent substance use: The effects of depressed mood and positive expectancies. Addictive Behaviors. 2011;36(5):488–493. doi: 10.1016/j.addbeh.2011.01.018. [DOI] [PubMed] [Google Scholar]
- Compas BE, Forehand RL, Thigpen JC, Keller G, Hardcastle E, Cole DA, et al. Family group cognitive-behavioral preventive intervention for families of depressed parents: 18- and 24-month outcomes. Journal of Consulting and Clinical Psychology. 2011;79(4):488–499. doi: 10.1037/a0024254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cook WL, Goldstein MJ. Multiple perspectives on family relationships: A latent variables model. Child Development. 1993;64(5):1377–1388. doi: 10.1111/j.1467-8624.1993.tb02958.x. [DOI] [PubMed] [Google Scholar]
- Dane AV, Schneider BH. Program integrity in primary and early secondary prevention: Are implementation effects out of control? Clinical Psychology Review. 1998;18(1):23–45. doi: 10.1016/s0272-7358(97)00043-3. [DOI] [PubMed] [Google Scholar]
- Delaney-Black V, Chiodo LM, Huestis MA, Ager J, Sokol RJ. Just say “I don't”: Lack of concordance between teen report and biological measures of drug use. Pediatrics. 2010;126:887–893. doi: 10.1542/peds.2009-3059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Downey G, Coyne JC. Children of depressed parents: An integrative review. Psychological Bulletin. 1990;108:50–76. doi: 10.1037/0033-2909.108.1.50. [DOI] [PubMed] [Google Scholar]
- Ennett ST, Bauman KE, Pemberton M, Foshee VA, Chuang Y-C, King TS. Mediation in a family-directed program for prevention of adolescent tobacco and alcohol use. Preventive Medicine. 2001;33:333–346. doi: 10.1006/pmed.2001.0892. [DOI] [PubMed] [Google Scholar]
- Fergusson DM, Woodward LJ. Mental health, educational, and social role outcomes of adolescents with depression. Archives of General Psychiatry. 2002;59:225–231. doi: 10.1001/archpsyc.59.3.225. [DOI] [PubMed] [Google Scholar]
- Forehand RL, McMahon RJ. Helping the noncompliant child: A clinician's guide to parent training. Guilford Press; New York: 1981. [Google Scholar]
- Ge X, Best KM, Conger RD, Simons RL. Parenting behaviors and the occurrence and co-occurrence of adolescent depressive symptoms and conduct problems. Developmental Psychology. 1996;32:717–731. [Google Scholar]
- Goodman SH, Gotlib IH. Risk for psychopathology in the children of depressed mothers: A developmental model for understanding mechanisms of transmission. Psychological Review. 1999;106:458–490. doi: 10.1037/0033-295x.106.3.458. [DOI] [PubMed] [Google Scholar]
- Grote NK, Zuckoff A, Swartz H, Bledsoe SE, Geibel S. Engaging women who are depressed and economically disadvantaged in mental health treatment. Social Work. 2007;52(4):295–308. doi: 10.1093/sw/52.4.295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haggerty KP, MacKenzie EP, Skinner ML, Harachi TW, Catlano RF. Participation in “Parents Who Care”: Predicting program initiation and exposure in two different program formats. Journal of Primary Prevention. 2006;27(1):47–65. doi: 10.1007/s10935-005-0019-3. [DOI] [PubMed] [Google Scholar]
- Haggerty KP, Skinner ML, MacKenzie EP, Catalano RF. A randomized trial of parents who care: Effects on key outcomes at 24-month follow-up. Prevention Science. 2007;8(4):249–260. doi: 10.1007/s11121-007-0077-2. [DOI] [PubMed] [Google Scholar]
- Hankin BL, Abramson LY, Moffitt TE, Silva PA, McGee R, Angell KE. Development of depression from preadolescence to young adulthood: Emerging gender differences in a 10-year longitudinal stduy. Journal of Abnormal Psychology. 1998;107:128–140. doi: 10.1037//0021-843x.107.1.128. [DOI] [PubMed] [Google Scholar]
- Hansell S, White HR. Adolescent drug use, psychological distress, and physical symptoms. Journal of Health and Social Behavior. 1991;32:288–301. [PubMed] [Google Scholar]
- Hasin DS, Goodwin R, Stinson FS, Grant BF. Epidemiology of major depressive disorder: Results from the National Epidemiologic Survey on Alcoholism and Related Conditions. Archives of General Psychiatry. 2005;62:1097–1106. doi: 10.1001/archpsyc.62.10.1097. [DOI] [PubMed] [Google Scholar]
- Hawkins JD, Catalano RF, Miller JY. Risk and protective factors for alcohol and other drug problems in adolescence and early adulthood: Implications for substance abuse prevention. Psychological Bulletin. 1992;112(1):64–105. doi: 10.1037/0033-2909.112.1.64. [DOI] [PubMed] [Google Scholar]
- Hennigan KM, O'Keefe M, Noether CD, Rinehart DJ, Russell LA. Through a mother's eyes: Sources of bias when mothers with co-occurring disorders assess their children. The Journal of Behavioral Health Services and Research. 2006;33(1):87–104. doi: 10.1007/s11414-005-9005-z. [DOI] [PubMed] [Google Scholar]
- Hoff RA, Rosenheck RA. The cost of treating substance abuse patients with and without comorbid psychiatric disorders. Psychiatric Services. 1999;50:1309–1315. doi: 10.1176/ps.50.10.1309. [DOI] [PubMed] [Google Scholar]
- Institute of Medicine and National Research Council . The science of adolescent risk-taking: Workshop report. Committe on the Science of Adolescence. The National Academies Press; Washington, DC: 2011. [PubMed] [Google Scholar]
- Johnston LD, O'Malley PM, Bachman JG, Schulenberg JE. Monitoring the Future national survey results on drug use, 1975–2009: Volume I, Secondary schools students (NIH Publication No. 10–7584) National Institute on Drug Abuse; Bethesda, MD: 2010. [Google Scholar]
- Kazdin AE. Parent management training: Evidence, outcomes, and issues. Journal of the American Academy of Child and Adolescent Psychiatry. 1997;36:1349–1356. doi: 10.1097/00004583-199710000-00016. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Chiu WT, Demler O, Walters EE. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry. 2005;62:617–627. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khantzian EJ. The self-medication hypothesis of addictive disorders: Focus on heroin and cocaine dependence. American Journal of Psychiatry. 1985;142:1259–1264. doi: 10.1176/ajp.142.11.1259. [DOI] [PubMed] [Google Scholar]
- Kovacs M, Devlin B, Pollock M, Richards C, Mukerji P. A controlled family history study of childhood-onset depressive disorder. Archives of General Psychiatry. 1997;54:613–623. doi: 10.1001/archpsyc.1997.01830190033004. [DOI] [PubMed] [Google Scholar]
- Kumpfer KL, Alvarado R. Family-strengthening approaches for the prevention of youth problem behaviors. American Psychologist. 2003;58:457–465. doi: 10.1037/0003-066X.58.6-7.457. [DOI] [PubMed] [Google Scholar]
- Lewinsohn PM, Rohde P, Seeley JR. Adolescent psychopathology III. The clinical consequences of comorbidity. Journal of the American Academy of Child and Adolescent Psychiatry. 1995;34:510–519. doi: 10.1097/00004583-199504000-00018. [DOI] [PubMed] [Google Scholar]
- Lieb R, Isensee B, Hofler M, Pfister H, Wittchen H-U. Parental major depression and the risk of depression and other mental disorders in offspring. Archives of General Psychiatry. 2002;59:365–374. doi: 10.1001/archpsyc.59.4.365. [DOI] [PubMed] [Google Scholar]
- Lipsey MW. Design sensitivity: Statistical power for experimental research. Sage; Newbury Park, CA: 1990. [Google Scholar]
- Mason WA, Hitchings JE, Spoth RL. Longitudinal relations among negative affect, substance use, and peer deviance during late adolescence. Substance Use and Misuse. 2009;44:1142–1159. doi: 10.1080/10826080802495211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGee R, Williams S, Poulton R, Moffitt TE. A longitudinal study of cannabis use and mental health from adolescence to early adulthood. Addiction. 2000;95:491–503. doi: 10.1046/j.1360-0443.2000.9544912.x. [DOI] [PubMed] [Google Scholar]
- Merikangas KR, Burstein M, Swanson SA, Avenevoli S, Cui L, Benjet C, et al. Lifetime prevalence of mental disorders in US adolescents: Results from the National Comorbidity Study-Adolescent Supplement (NCS-A). Journal of the American Academy of Child and Adolescent Psychiatry. 2010;49(10):980–989. doi: 10.1016/j.jaac.2010.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newcomb MD, Bentler PM. Consequences of adolescent drug use: Impact on the lives of young adults. Sage; Newbury Park, CA: 1988. [Google Scholar]
- O'Connell ME, Boat T, Warner KE. Preventing mental, emotional, and behavioral disorders among young people: Progress and possibilities. The National Academies Press; Washington, DC: 2009. [PubMed] [Google Scholar]
- Olds DL, Kitzman H, Hanks C, Cole R, Anson E, Sidora-Arcoleo K, et al. Effects of nurse home visiting on maternal and child functioning: Age 9 follow-up of a randomized trial. Pediatrics. 2007;120(4):832–845. doi: 10.1542/peds.2006-2111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pine DS, Cohen P, Gurley D, Brook J, Ma Y. The risk for early-adulthood anxiety and depressive disorders in adolescents with anxiety and depressive disorders. Archives of General Psychiatry. 1998;55:56–64. doi: 10.1001/archpsyc.55.1.56. [DOI] [PubMed] [Google Scholar]
- Radoloff LS. The CESD-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- Reinherz HZ, Giaconia RM, Carmola Hauf AM, Wasserman MS, Paradis AD. General and specific childhood risk factors for depression and drug disorders by early adulthood. Journal of the American Academy of Child and Adolescent Psychiatry. 2000;39(2):223–231. doi: 10.1097/00004583-200002000-00023. [DOI] [PubMed] [Google Scholar]
- Rice F, Harold G, Thapar A. The genetic aetiology of childhood depression: A review. Journal of Child Psychology and Psychiatry. 2002;43:65–79. doi: 10.1111/1469-7610.00004. [DOI] [PubMed] [Google Scholar]
- Rohde P, Lewinsohn PM, Seeley JR. Psychiatric comorbidity with problematic alcohol use in high school students. Journal of the American Academy of Child and Adolescent Psychiatry. 1996;35:101–109. doi: 10.1097/00004583-199601000-00018. [DOI] [PubMed] [Google Scholar]
- Rush AJ, Trivedi MH, Ibrahim HM, Carmody TJ, Arnow B, Klein DN, et al. The 16-item quick inventory of depressive symptomatology (QIDS), clinical rating (QIDS-C), and self-report (QIDS-SR): A psychometric evaluation in patients with chronic major depression. Biological Psychiatry. 2010;54:573–583. doi: 10.1016/s0006-3223(02)01866-8. [DOI] [PubMed] [Google Scholar]
- Shelton KK, Frick PJ, Wootton J. Assessment of parenting practices in families of elementary school-age children. Journal of Clinical Child Psychology. 1996;25:317–329. [Google Scholar]
- Spoth R, Clair S, Greenberg M, Redmond C, Shin C. Toward dissemination of evidence-based family interventions: Maintenance of community-based partnership recruitment results and associated factors. Journal of Family Psychology. 2007;21(2):137–146. doi: 10.1037/0893-3200.21.2.137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spoth R, Redmond C, Hockaday C, Shin C. Barriers to participation in family skills preventive interventions and their evaluations: A replication and extension. Family Relations. 1996;45(3):247–254. [Google Scholar]
- Spoth R, Redmond C, Shin C. Direct and indirect latent-variable parenting outcomes of two universal family-focused preventive interventions: Extending a public health-oriented research base. Journal of Consulting and Clinical Psychology. 1998;66:385–399. doi: 10.1037//0022-006x.66.2.385. [DOI] [PubMed] [Google Scholar]
- Spoth R, Redmond C, Shin C, Azevedo K. Brief family intervention effects on adolescent substance initiation: School-level growth curve analyses 6 years following baseline. Journal of Consulting and Clinical Psychology. 2004;72(3):535–542. doi: 10.1037/0022-006X.72.3.535. [DOI] [PubMed] [Google Scholar]
- Sroufe L. Psychopathology as an outcome of development. Development and Psychopathology. 1997;9:251–268. doi: 10.1017/s0954579497002046. [DOI] [PubMed] [Google Scholar]
- Sroufe L, Rutter M. The domain of developmental psychopathology. Child Development. 1984;55:17–29. [PubMed] [Google Scholar]
- Tolan PH, Dodge KA. Children's mental health as a primary care and concern. American Psychologist. 2005;60:601–614. doi: 10.1037/0003-066X.60.6.601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Webster-Stratton C. Preventing conduct problems in head start children: Strengthening parent competencies. Journal of Consulting and Clinical Psychology. 1998;66:715–730. doi: 10.1037//0022-006x.66.5.715. [DOI] [PubMed] [Google Scholar]
- Weissman MM, Pilowsky DJ, Wickramaratne PJ, Talati A, Wisniewski SR, Fava M, et al. Remission in maternal depression and child psychopathology: A STAR*D-child report. Journal of the American Medical Association. 2006;295:1389–1398. doi: 10.1001/jama.295.12.1389. [DOI] [PubMed] [Google Scholar]
- Weissman MM, Warner V, Wickramaratne PJ, Moreau D, Olfson M. Offspring of depressed parents: 10 years later. Archives of General Psychiatry. 1997;54:932–940. doi: 10.1001/archpsyc.1997.01830220054009. [DOI] [PubMed] [Google Scholar]
- Windle M, Windle RC. Depressive symptoms and cigarette smoking among middle adolescents: Prospective associations and intrapersonal and interpersonal influences. Journal of Consulting and Clinical Psychology. 2001;69(2):215–226. [PubMed] [Google Scholar]