Abstract
Chronic diseases are among the most costly and, in part, preventable health problems that share common behavioral risk factors. Data related to the prevalence of chronic diseases, such as diabetes, their risk factors, and the description of the capacity of the health and medical care system to address these problems are limited in the US-affiliated Pacific Islands (USAPI). This paper presents the background and methods used in conducting comprehensive assessments of the health care systems in ten sites across the USAPI. The principles used as the basis for conducting these assessments included capacity building and skills training. The methods included identifying the on-site Needs Assessment Team (NAT), developing the conceptual model; archival data collection; key informant interviews; reviewing data and documents to identify the key problems and issues to be prioritized; and reviewing and prioritizing the problems and issues.
Background
Non-communicable diseases including heart disease, stroke, cancer, diabetes, and arthritis, are among the most common, costly, and largely preventable health problems in the United States. Four modifiable health risk behaviors—lack of physical activity, poor nutrition, tobacco use, and excessive alcohol consumption—are responsible for much of the morbidity and early death related to the burden of chronic diseases.1 The World Health Organization (WHO) reports that serious health issues in American Samoa relate to the increase in obesity-related chronic diseases associated with lifestyle, improper nutrition, and lack of physical activity. Significant increases in the prevalence of obesity at increasingly younger ages are associated with hypertension, cardiovascular diseases, cerebrovascular diseases, type 2 diabetes and its complications, and some forms of cancer.2 In the Republic of the Marshall Islands (RMI), exposure to American culture has brought about a rise in levels of adult obesity, non-communicable diseases, teenage pregnancy, suicide, alcoholism and tobacco use.2 Although infectious diseases continue to be prevalent in the Federated States of Micronesia (FSM), the disease burden also includes non-communicable diseases, such as diabetes, nutritional, and metabolic diseases. Contributing factors to these conditions are believed to be a change in diet, lack of exercise, gender and age.2 Like many developing nations, the Republic of Palau has undergone an epidemiological shift from diseases of the developing world, such as malnutrition and infectious diseases, to an increasing burden of diseases of the developed world, like diabetes, heart disease, obesity and kidney failure.2 In the Commonwealth of the Northern Marianna Islands (CNMI), obesity, diabetes, hypertension, and atherosclerotic vascular disease are increasing concerns facing the population.2
Although surveillance data are limited and published data for specific USAPI are difficult to find, some data can be presented on the prevalence of diabetes. The estimated prevalence of diagnosed diabetes among adults was 11% in Guam between 2001–2003; 24.4% in the State of Pohnpei, (FSM) and 29.8% in RMI in 2002; 38.9% in Palau in 2006; and 47.3% in American Samoa in 2004.3 In comparison, the National Center for Health Statistics reported that in 2010, the percent of the population 20 years of age and older in the United States with diagnosed and undiagnosed diabetes was 11.3%. It was also reported that diabetes was the seventh leading cause of death in the United States as well as the leading cause of kidney failure, non-traumatic lower-limb amputations, and new cases of blindness among adults.4
In 2008, the Pacific Chronic Diseases Council (PCDC) was formed with assistance and support from the Division of Diabetes Translation of the Centers for Disease Control and Prevention, Papa Ola Lōkahi Native Hawaiian Health Board, and the National Association of Chronic Diseases Directors. The PCDC members include the Non-Communicable Disease (NCD) Program coordinators and the Diabetes Prevention and Control Program (DPCP) coordinators from the six USAPI that include American Samoa, CNMI, Guam, FSM, RMI, and the Republic of Palau. The purpose of the PCDC is to address the issues related to chronic diseases in the Pacific region by providing an avenue to act collectively with international, professional, governmental, community, and faith-based organizations and other non-governmental organizations (NGO) on issues that affect the successful development, management, implementation, and evaluation of chronic disease programs. The priorities of the PCDC are to provide training opportunities to build the capacity and skills of the PCDC coordinators and their partners, and to conduct a comprehensive assessment of the system of services for chronic diseases and diabetes prevention and control. To fulfill some of these priorities, the National Institutes of Health's National Institute on Minority Health and Health Disparities (NIH-NIMHD) provided funding, with administrative support through the Department of Native Hawaiian Health in the John A. Burns School of Medicine at the University of Hawai‘i at Mānoa, to conduct comprehensive assessments of the system of services in ten sites throughout the USAPI.
Purpose
Throughout the USAPI, data on the prevalence of chronic diseases, including diabetes, its complications, and risk factors, are limited and there is little documented information on the system of services for the prevention and control of the risk factors for diabetes and other chronic diseases. The purpose of these comprehensive assessments was to identify and describe the most current data available related to non-communicable diseases, with a focus on diabetes, and to describe the capacity of the administrative system, data system, clinical services, and support services to address the problems associated with chronic diseases and their risk factors. These assessments were conducted in American Samoa, the CNMI, FSM (Chuuk, Pohnpei, Kosrae, Yap), Guam, RMI (Majuro, Ebeye), and the Republic of Palau. This volume presents the preliminary findings of the most current data and the status of major components of the health and medical care delivery systems in each of the sites. It is anticipated that these findings will inform and encourage health planners, health care providers, epidemiologists, and researchers to conduct further studies and begin to address some of the issues identified in these assessments.
Methods
The methods of the assessment included the following principles:
Capacity Building and Skills Training
During each site visit, the consultant provided technical assistance and skills training for the on-site Needs Assessment Team (NAT) members on topics such as the basic components of the planning cycle (assess need, identify issues, develop goals and objectives, implement, evaluate), principles of conducting a needs assessment as part of planning, principles of interviewing techniques and collecting qualitative data, principles of qualitative data analysis, and how to use the Criteria Weighting Method (see description below) to develop the priority of issues and problems.
The methods employed included development of a conceptual model; establishment of the on-site NAT; archival data collection; key informant interviews; and identification of key issues and problems and their prioritization. These methods are described as follow:
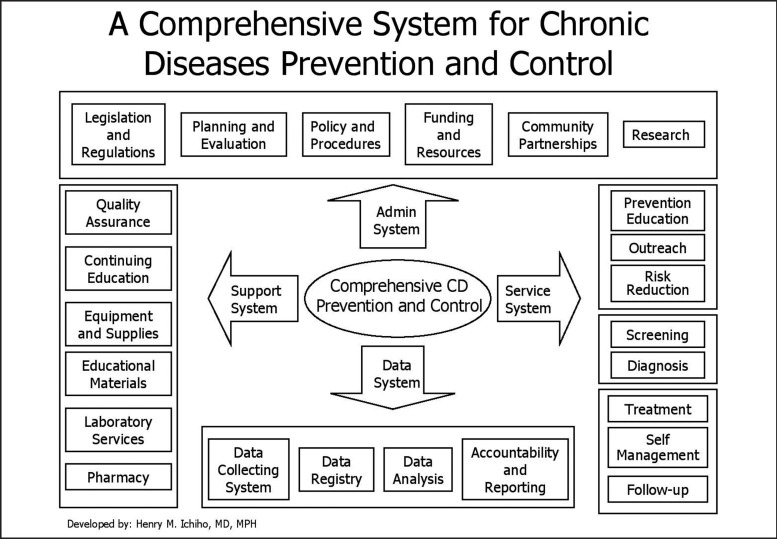
Conceptual Model
To develop the conceptual model for the framework for the assessment, the consultant (Henry Ichiho, MD, MPH) collaborated with the PCDC representatives from the six USAPI jurisdictions to conceptualize a model of the system of services for NCD and diabetes prevention and control that included specific sub-system components for data, administration, clinical services, and support services. Survey questions were developed based on this model and included questions relevant to each of the system components. Key informants were identified and interviewed to obtain the information on the status of each of the system components. In addition to the survey questions, procedures for collecting data and information were developed to standardize data collection across all the sites.
On-site Needs Assessment Team
The consultant worked with individual members of the PCDC to identify a NAT leader and the team members and to obtain approval to conduct the assessment from the respective Minister/Secretary/Director of Health at each site. The team leader selected was the NCD Coordinator, the Diabetes Prevention and Control Program Coordinator, or a Public Health Administrator. The team members for each site were selected by the team leader because of their involvement in working with staff of the diabetes or NCD program. The responsibilities of the NAT were to plan and schedule the on-site assessment, identify and gather documents and current data; identify and communicate with key informants and schedule interviews; assist the consultant to review all the data and information, and identify the problems and issues to be prioritized; recruit members of local administrative and clinical groups to prioritize the issues; and participate in all the activities of the assessment. The team leaders also assisted in the analysis, reporting, and dissemination of results in each of the sites.
Archival Data Collection
On-site NAT members were responsible for identifying and collecting documents and information prior to the site visit. All data and information for this report were extracted and summarized from existing documents, reports, and datasets. No new data were collected or generated. The documents collected were: data from Behavioral Risk Factor Surveillance System surveys; WHO's NCD-STEPS surveys; Youth Risk Behavior Survey; household health surveys; mortality and morbidity reports; Jurisdiction or State NCD Strategic Plans; program summary and evaluation reports; research reports and other pertinent documents. These documents were reviewed and assessed by the consultant and the NAT members. Brief descriptions of the major national and international surveys are included here.
(a) Behavioral Risk Factor Surveillance System (BRFSS)
The BRFSS, established by the Centers for Disease Control and Prevention, is a state-based telephone survey of adults that collects data on health risk behaviors, preventive health practices, and health care access primarily related to chronic disease and injury. The BRFSS questionnaire consists of three components: (1) The Core Questions, (2) Optional Modules, and (3) State-added Questions. BRFSS data are used to identify emerging health problems, track health objectives, develop and evaluate public health policies and programs, and support health-related legislative efforts.5
(b) WHO STEPwise Approach to Surveillance (STEPS)
The STEPS approach is a simple, standardized method for collecting, analyzing and disseminating data related to the risk factors that contribute to the burden of NCDs. The STEPS approach is flexible and has three levels. Within each level, risk factor assessment is divided into core, expanded, and optional modules. The STEPS Instrument covers three different “steps” of risk factor assessment: (1) the Questionnaire contains self-report measures to include socio-economic data, data on tobacco and alcohol use, and measures of nutritional status and physical inactivity; (2) physical measurements, such as height, weight, waist circumference, and blood pressure; and (3) biochemical measurements, such as fasting blood sugar, total cholesterol, HDL-cholesterol, and triglycerides. By using standardized questions and protocols, jurisdictions can use STEPS information to monitor within-jurisdiction trends and to make comparisons across the six USAPI jurisdictions.6 Some of the definitions for selected indicators used in the survey are included in Table 1.
(c) Youth Risk Behavior Surveillance System (YRBSS)
The YRBSS was developed by the Centers for Disease Control and Prevention to monitor health risk behaviors that contribute to the leading causes of death, disability, and social problems among youth. These behaviors include: unintentional injuries, sexual behavior, alcohol and other drug use, tobacco use, unhealthy dietary behaviors, inadequate physical activity. It also monitors the prevalence of obesity and asthma. The Departments of Health and Education survey students in public schools in Grades 9 through 12 every other year. The YRBSS was designed to: determine the prevalence and monitor the trends of health risk behaviors; examine the co-occurrence of health risk behaviors; provide data for national, state, territorial, tribal, local comparisons, and monitor progress toward achieving objectives and program indicators.7 Definitions for BMI-for-age status used in the survey are included in Table 2.
(d) Global Youth Tobacco Survey (GYTS)
The GYTS is a school-based survey that collects data on students 13–15 years using a standardized method for constructing the sampling frame and selecting schools and classes. The intent of this survey is to enhance the capacity of the jurisdictions to design, implement, and evaluate tobacco control and prevention programs. The survey includes data on prevalence of cigarette and other tobacco use and five determinants of tobacco use: access, availability, and price; exposure to second hand smoke; cessation; media and advertising, and school curriculum.8
Key Informant Interviews
Qualitative data were obtained by using the survey questionnaire developed by the consultant to interview health administrators, program managers, directors of clinical laboratory and pharmacy, information managers, hospital records personnel, and public health and hospital personnel. The consultant and at least one member of the NAT conducted the key informant interviews.
Identification of Key Issues and Problems
The NAT members assisted in the analysis of the data and information from the archival documents and datasets as well as interviews with key informants. Based on this information, team members identified issues and problems that described the deficits in the administrative, data, service delivery, and support services infrastructure. These issues and problems were categorized into the administrative and the clinical areas and two lists were produced. The administrative and clinical lists were then presented to the respective Administrative Group and Clinical Group for prioritization.
Prioritization Using an Adapted Criteria Weighting Method
At each of the sites, an Administrative Group and a Clinical Group were convened separately to assess the list of problems and to define the priorities. The Administration Group was comprised of hospital and clinic administrators, chiefs of nursing, public health administrators, program coordinators, and information managers. The Clinical Group was comprised of hospital and clinic physicians and nurses, nurse supervisors, and program coordinators. These groups used an adapted Criteria Weighting Method9 to prioritize the administrative and clinical problems respectively. The adapted Criteria Weighting Method used six criteria: need, implementation feasibility, required resources, political feasibility, control, and cost. The members of each of the priority-setting groups independently assessed the problem statements using each of the criteria and ranked the problems from first choice to last choice. All of the scores from the individual group members were aggregated and averaged to determine the priority ranking for the group. This process resulted in a unique list of administrative and clinical priorities for each of the sites.
Format of the Assessment Report
The assessment reports for the ten sites follow the same format and include the following:
-
Introduction and Background
Abstract
Introduction
Description of the Geography
Population and Characteristics of the Population
-
Data
Mortality Data
Population-Based Surveillance Data
Data on Risk Factors for NCDs
Diabetes Specific and Related Data
-
Description of the Administrative System
Legislation and Regulations
Planning Documents
Policy and Procedure Manuals
Health Insurance
Partnerships and Collaborations
Research
-
Description of the Clinical Services System
Outreach and Prevention
Screening and Diagnosis
Treatment and Management
Specialty Clinics
-
Description of the Support Services System
Quality Assurance and Continuing Education Program
Diabetes Health Education Materials
Pharmacy
Laboratory Services
Description of the Data System
Conclusion — Prioritized Issues and Needs
Figure 1.
Table 1.
Definitions of Indicators, NCD-STEPS Survey
| NCD-STEPS Indicator | Collection Method | Definition |
| Overweight | Measured weight/height | BMI (kg/m2) ≥25 |
| Obese | Measured weight/height | BMI (kg/m2) ≥30 |
| Central obesity | Measured | Waist circumference ≥40 inches — Men; Waist circumference ≥35 inches - Women |
| Diabetes (Venous) | Fasting blood sugar | FBS≥126 mg/dl or taking medication |
| Diabetes (Capillary) | Fasting blood sugar | FBS≥110 mg/dl or taking medication |
| Hypercholesterolemia | Fasting blood sugar | Cholesterol≥200 mg/dl |
| Hypertension | Measured | Blood pressure≥140/90mm/hg or taking medication |
| Current tobacco use (smoking) | Self-report | Any tobacco product used (smoking) in the past 12 months |
| Daily tobacco use (smoking) | Self-report | Any tobacco product used (smoking) every day |
| Current alcohol use | Self-report | Any alcohol consumption within the past 12 months |
| Binge drinking | Self-report | Five or more drinks for males and four or more drinks for females per drinking day on any day during the past week |
Data Source: WHO, NCD-STEPS Manual10
Table 2.
Definitions of Indicators, YRBS Survey
| YRBS Indicator | Collection Method | Definition |
| Overweight (Children) | Self-report on questionnaire | BMI ≥85th percentile but < 95th percentile based on sex- and age-specific reference data |
| Obese (Children) | Self-report on questionnaire | BMI ≥95th percentile based on sex- and age-specific reference data |
Data Source: Centers for Disease Control and Prevention, Adolescent and School Health11
Acknowledgements
Funded by the National Institute on Minority Health and Health Disparities (NIMHD) of the National Institutes of Health (NIH) (Grant 3R24MD001660). The content is solely the responsibility of the author and does not necessarily represent the official views of the NIMHD or the NIH.
Glossary
- ADA
American Diabetes Associati
- AusAID
Australian A
- BMI
Body mass index
- BRFSS
Behavioral Risk Factor Surveillance System
- CDC
Centers for Disease Control and Prevention
- CDE
Certified diabetes educator
- CDEMS
Chronic Disease Electronic Management System
- CHC
Community Health Center
- CNMI
Commonwealth of the Northern Mariana Islands
- CSHCP
Chuuk State Health Care Plan
- CWC
Chuuk Women's Council (Chuuk, FSM)
- DDT
Division of Diabetes Translation
- DOH
Department of Health
- DPCP
Diabetes Prevention and Control Program
- FSM
Federated States of Micronesia
- FSMNGEHIP
Federated States of Micronesia National Government Employees' Health Insurance Plan
- GYTS
Global Youth Tobacco Survey
- HDC
Health Disparities Collaborative
- IDF
International Diabetes Federationyy
- KUMIT
Komaron Ukot Mour Ilo Tomak (RMI)
- LBJ
Lyndon B. Johnson Tropical Medical Center (American Samoa)
- LTBI
Latent tuberculosis infection
- MDR-TB
Multiple drug resistant tuberculosis
- MiCare
State run health plan for the FSM
- MOH
Ministry of Health
- NAT
Needs Assessment Team
- NCD
Non-Communicable Disease(s)
- NGO
Non-Governmental Organization
- NIH-NIMHD
National Institutes of Health - National Institute on Minority Health and Health Disparities
- PCDC
Pacific Chronic Diseases Council
- PECS
Patient Electronic Care System
- RMI
Republic of the Marshall Islands
- STEPS
WHO STEPwise Approach to Surveillance of NCD Risk Factors
- SPC
Secretariat of the Pacific Community
- UAK
Ulkerreuil A Klengar Community Health Support Group (Palau)
- USAPI
United States-associated Pacific Islands
- WIC
Supplemental Nutrition Program for Women, Infants and Children
- WHO
World Health Organization
- YRBS
Youth Risk Behavior Survey
Disclosure Statement
The authors report no conflict of interest.
References
- 1.Centers for Disease Control and Prevention, author. Chronic Disease and Health Promotion Web site. [August 2, 2012]. http://www.cdc.gov/chronicdisease/overview/index.htm.
- 2.World Health Organization, author. Western Pacific Region. Western Pacific Country Health Information Profiles: 2009 Revision. Geneva, Switzerland: World Health Organization; 2009. [Google Scholar]
- 3.Hosey G, Aitaoto N, Satterfield D, Kelly J, Apaisam CJ, Belyeu-Camacho T, deBrum I, Luces PS, Rengiil A, Turituri P. The culture, community, and science of type 2 diabetes prevention in the US Associated Pacific Islands. Preventing Chronic Disease. 2009;6(3):1–10. [PMC free article] [PubMed] [Google Scholar]
- 4.U.S. Department Of Health and Human Services, National Diabetes Information Clearinghouse Web site, author. National Diabetes Statistics. 2011. [August 12, 2012]. http://diabetes.niddk.nih.gov/dm/pubs/statistics/#fast.
- 5.Centers for Disease Control and Prevention, author. About the BRFSS Web site. [September 25, 2012]. http://www.cdc.gov/brfss/about.htm.
- 6.World Health Organization, author. Chronic Diseases and Health Promotion Web site. [September 25, 2012]. http://www.who.int/chp/steps/riskfactor/en/index.html.
- 7.Centers for Disease Prevention and Control, author. Youth Risk Behavioral Surveillance System: System Overview Web site. [September 25, 2012]. http://www.cdc.gov/healthyyouth/yrbs/pdf/system_overview_yrbs.pdf.
- 8.Centers for Disease Control and Prevention, author. Global Youth Tobacco Survey Overview Web site. [September 25, 2012]. http://apps.nccd.cdc.gov/gtssdata/Ancillary/Documentation.aspx?SUID=1&DOCT=1.
- 9.Centers for Disease Control and Prevention, Public Health Practice Program Office, National Association of City and County Health Officials, author. Assessment Protocol for Excellence in Public Health (APEXPH) in Practice. [June 10, 2012]. http://www.cdc.gov/nphpsp/documents/prioritization.pdf. Published March 1, 1991.
- 10.World Health Organization, author. Chronic Diseases and Health Promotion, STEPS Manual, Section 4: Reporting and Disseminating Results Web site. [October 23, 2012]. http://www.who.int/chp/steps/Part4_Section4.pdf.
- 11.Centers for Disease Control and Prevention, Adolescent and School Health, Questionnaire and Item Rationale Web site, author. [October 21, 2012]. http://www.cdc.gov/healthyyouth/yrbs/pdf/questionnaire/2011_hs_questionnaire.pdf.