Abstract
Previous studies have demonstrated that prior infection by various bacterial pathogens induces nonspecific resistance to subsequent infection by other gram-negative and gram-positive bacterial pathogens. In the present study, we evaluated whether underlying inflammation enhanced host resistance to inhalational Bacillus anthracis infection in New Zealand White rabbits (SPF; Bordetella- and Pasteurella-free). Accordingly, rabbits were pretreated with either the inflammagen bacterial LPS (60,000 EU/kg), a component of the outer membrane of gram-negative bacteria, or saline (vehicle). Administration of LPS resulted in brief pyrexia and a significant increase in the proinflammatory cytokine TNFα, thus confirming LPS-induced inflammation. At 24 h after LPS treatment, rabbits were exposed to aerosolized B. anthracis spores (Ames strain; approximately 300 LD50). Blood samples collected at various times after challenge were cultured. Compared with their saline-pretreated counterparts, LPS-pretreated, B. anthracis-challenged rabbits exhibited delays in 2 biomarkers of B. anthracis infection—anthrax-induced pyrexia (25 h versus 66 h after challenge, respectively) and bacteremia (26 h versus 63 h, respectively)—and survived longer (41 h versus 90 h, respectively). Similar to control animals, all LPS-pretreated, B. anthracis-challenged rabbits exhibited pathology consistent with inhalational anthrax. Taken together, these results suggest that prior or underlying stimulation of the innate immune system induces transient host resistance to subsequent B. anthracis infection in SPF New Zealand white rabbits. In particular, our results emphasize the importance of using animals that are free of underlying infections to prevent confounding data in studies for inhalational anthrax characterization and medical countermeasure evaluation.
Abbreviations: EU, endotoxin units
Aerosolized spores of the gram-positive bacterium B. anthracis are an important biothreat.40,47 Without aggressive prophylaxis or intervention, inhalational anthrax results in high mortality rates.4,5 The 1979 anthrax outbreak in Sverdlosk, Russia, and the 2001 anthrax attacks in the United States illustrated that inhalational anthrax can be rapidly fatal.24,40,47
Gaps in our healthcare system were revealed as a direct consequence of the 2001 anthrax attacks in the United States, precipitating renewed interest in identifying effective therapeutics strategies against symptomatic anthrax in nonvaccinated persons.4,5,40,48 Well-characterized animal models are essential for the development of therapeutic strategies directed against inhalational anthrax. In particular, rabbits are sensitive to B. anthracis challenge and, although the disease progresses more rapidly in rabbits, anthrax-induced pathologic changes are similar to those in humans.16,27,29,62 Moreover, rabbits are predictive of the outcome of inhalational anthrax in nonhuman primates.26,61 The sensitivity of rabbits to this highly pathogenic disease makes them a valuable animal model to evaluate product effectiveness in preliminary vaccine and drug trials.62 Recently, we developed a comprehensive natural history study for New Zealand white rabbits exposed to aerosolized Ames strain B. anthracis and demonstrated the potential of these rabbits as a therapeutic model for the testing of pharmaceuticals against inhalational anthrax.68
However, differences in the length of survival of New Zealand white rabbits after lethal challenge with aerosolized B. anthracis spores have been observed.9,28,42,68 This disparity in survival time may be the result, in part, of differences in sources, namely the use of conventionally sourced rabbits or rabbits that have not been certified to be free of Bordetella and Pasteurella spp. as compared with Bordetella-free, Pasteurella-free SPF rabbits. Unlike SPF rabbits, conventional rabbits may be colonized with many common pathogens, including gram-negative bacteria such as Pasteurella and Bordetella.39 Differences in anthrax survival according to animal source (conventional compared with germ-free) has previously been reported in a rat model.59 A recent study13 found that stimulation of the innate immune system with aerosolized bacterial lysate in mice protected against subsequent exposure from a broad range of pathogens, including B. anthracis, Yersinia pestis, and Francisella tularensis, possibly due to the activation of protective pathways. Moreover, other investigators30 reported an innate immune response due to nosocomial infection from gram-negative Serratia marcescens that induced a protective effect in African green monkeys challenged with aerosolized B. anthracis spores. Similar host resistance has been observed in other animal models, wherein prior bacterial infection or pretreatment with the inflammagen bacterial LPS induced nonspecific (innate) resistance to subsequent infections by gram-negative and gram-positive pathogens.13,15,37,44,65 LPS is an integral constituent of the outer cell wall of gram-negative bacteria and a potent inflammagen in humans and mammals.22,52 Taken together, these findings support the premise that prior or underlying activation of the innate immune system in rabbits may be responsible for transient host resistance to B. anthracis infection and thereby prolong their survival.
In the present investigation, we evaluated whether underlying inflammation enhanced host resistance to inhalational B. anthracis infection in Bordetella-free, Pasteurella-free SPF New Zealand white rabbits. At 24 h after pretreatment with a noninjurious dose of the inflammagen LPS, rabbits were exposed to aerosolized B. anthracis spores, and clinical signs, onset of bacteremia, and survival were assessed. Overall, our results demonstrated that prior or underlying stimulation of the innate immune system induced transient resistance to subsequent B. anthracis infection in NZW rabbits, significantly delaying the onset of inhalational anthrax and prolonging survival.
Materials and Methods
Animals.
Certified Bordetella-free, Pasteurella-free SPF male and female New Zealand white rabbits (Oryctolagus cuniculus; weight, 3.0 to 3.6 kg) were acquired from Charles River Laboratories (Pointe-Claire, Quebec, Canada). These rabbits were also free of Pseudomonas aeruginosa. Rabbits were housed in individual cages and acclimated to a 12:12-h light:dark cycle in a temperature- and humidity-controlled, SPF environment. Rabbits were maintained according to facility standard operating procedures, with food and water provided ad libitum.
In the LPS dose-determination study, all rabbits were acclimated to the facility for at least 7 d before subcutaneous injection of a microchip transponder (model IPTT300, BioMedic Data Systems, Seaford, DE) into the animal's flank to monitor body temperature. Similarly, in the B. anthracis infection study, all rabbits were acclimated to the facility for at least 7 d before surgical implantation of a venous access port (Solomon Scientific, San Antonio, TX) to facilitate frequent phlebotomy sampling and a radiotelemetry device (model TA10TA-D70; Data Sciences International, St Paul, MN) to measure body temperature continuously. For surgery, anesthesia was induced with ketamine–xylazine solution (ketamine HCl, 23.5 mg/kg; xylazine HCl, 4.7 mg/kg; Vedco, St Joseph, MO), and general anesthesia was maintained with isoflurane by using a laryngeal mask airway. Use of the laryngeal mask airway did not result in aspiration pneumonia (as later determined through histopathology). Venous access port was a femoral catheter with an exit line tunneled subcutaneously to a dorsal location between the right scapulae and the spine. The radiotelemetry device was implanted in the subcutaneous tissue of the left side of the abdomen. Rabbits were allowed to recover for at least 10 d from either microchip transponder implantation or surgery and were deemed to be clinically healthy (per physical exam and blood culture) before use.
Research was conducted under an IACUC-approved protocol in compliance with the Animal Welfare Act, PHS Policy, and other federal statutes and regulations relating to animals and experiments involving animals.2,3,46 The facility where this research was conducted is accredited by AAALAC and adheres to principles stated in the Guide for the Care and Use of Laboratory Animals.45
LPS.
LPS (Escherichia coli 055:B5; 3 × 106 endotoxin units [EU]/mg; Sigma Chemical Company, St Louis, MO) diluted in sterile, nonpyrogenic saline (0.9% sodium chloride; Baxter, Deerfield, IL) or equivalent volume sterile, nonpyrogenic saline (vehicle) was administered intravenously to rabbits. LPS activity was determined by using a chromogenic, endpoint Limulus Amebocyte Lysate assay (Lonza, Walkersville, MD). Because activity varies between LPS lots, the same LPS lot was used throughout. LPS is expressed in EU, whereby 1 EU is equivalent to 100 pg of United States standard endotoxin.41 Therefore, an LPS dose of 60,000 EU/kg is equivalent to 6 µg/kg of the United States standard endotoxin. Although LPS and endotoxin are used interchangeably, LPS is actually the principal biologically active component of endotoxin.22,63
LPS dose-determination study.
Sixteen rabbits were injected intravenously with saline or various doses of LPS once daily for 1 or 2 d. At 90 min after LPS or saline administration, blood samples were collected from each rabbit, allowed to clot in tubes (Rapid Serum tubes, BD Bioscience, San Jose, CA) for approximately 1 h at room temperature, and then centrifuged. Serum was separated for analysis of LDH activity and increased levels of the proinflammatory cytokine TNFα. Within an hour after LPS exposure, circulating TNFα levels increase transiently.21 Serum samples also were used for additional blood chemistry tests. Body temperature was recorded manually (model DAS7007s Handheld Reader System, BioMedic Data Systems) every 10 min from 1 h before LPS or saline administration (to establish baseline temperature) until 2 h after LPS or saline administration. Pyrexia was defined as a body temperature that exceeded 40 °C for at least 3 sequential time points.1,54,58 All rabbits were euthanized at the study endpoint of 7 d after LPS or saline administration.
LDH assay.
LDH activity, a general biomarker for tissue injury,57 was measured by the colorimetric assay (Bioassay Systems, Hayward, CA) on a microplate reader (SpectraMax 190 Absorbance Microplate Reader, Molecular Devices, Sunnyvale, CA).
TNFα assay.
TNFα levels, a biomarker for inflammatory response, were determined through ELISA. Briefly, polyclonal goat antirabbit TNFα capture antibody (1 µg/mL, BD Biosciences) was incubated overnight in wells of an enhanced protein-binding plate (BD Biosciences). Wells were washed with wash buffer (BD OptEIA Reagent Set B; BD Biosciences); blocking buffer (assay diluent; BD OptEIA Reagent Set B; BD Biosciences) then was incubated in wells at room temperature for 2 h. After washing, standards (various concentrations of recombinant rabbit TNFα; BD Biosciences) and serum samples were incubated in plate wells at room temperature for 4 h. Plates then were washed, biotinylated mouse antirabbit TNFα secondary antibody (0.5 µg/mL; BD Biosciences) was added to each well and incubated at room temperature for 1 h. After washing, streptavidin-labeled horseradish peroxidase (dilution, 1:1000; BD Biosciences) was added to each well and incubated at room temperature for 30 min. Plates were washed and then substrate (substrate reagents A and B; BD OptEIA Reagent Set B, BD Biosciences) was added to wells and allowed to incubate at room temperature for 20 min before reaction was halted by using stop solution (BD OptEIA Reagent Set B; BD Biosciences). Plates were then read at 450 nm (subtracting 570 nm) on a microplate reader (Molecular Devices).
Blood chemistry.
Serum samples were analyzed for changes in aspartate aminotransferase (AST) and alanine aminotransferase (ALT) levels, 2 biomarkers for liver injury,57 using a Vitros 5600 Clinical Laboratory System (Ortho Clinical Diagnostics, Rochester, NY).
Infection studies.
LPS (60,000 EU/kg) or saline was administered intravenously to 18 rabbits 24 h before challenge with B. anthracis spores. At 90 min after LPS or saline administration, blood samples were collected from each rabbit, allowed to clot in tubes (BD Biosciences) for approximately 1 h at room temperature, and then centrifuged. Serum was separated for analysis for increased LDH activity and TNFα levels. Starting at 12 h after challenge and continuing at 12-h intervals thereafter, blood samples were collected for culture (that is, bacteremia analysis) until rabbits succumbed or were euthanized.
Telemetry data analysis.
Body temperature was recorded every 15 min by using radiotelemetry (DataQuest ART3.1 system, Data System International, Overland Park, KS) for the B. anthracis infection studies. To establish the temperature baseline, data were collected at least 72 h before LPS or saline administration. Data collection continued until the rabbits succumbed or were euthanized. Pyrexia was defined as a body temperature exceeding 40 °C for at least 3 sequential time points.1,54,58 During aerosol challenge with B. anthracis spores, no temperature data were recorded.
Spore preparation.
B. anthracis (Ames strain) spores were produced in flask cultures containing Leighton and Doi medium31 in a Biologic Safety level 3 laboratory.51 After centrifugation, the spore pellet was washed in sterile water and purified on gradients of 60% Hypaque 76 (GE Healthcare, Piscataway, NJ). Spores were stored in 1% phenol at 4 °C until use. Phenol was removed before aerosolization, and spores were resuspended in sterile water and heat-shocked at 60 °C for 45 min.
Aerosol exposure.
Immediately before challenge, whole-body plethysmography (head out; Buxco Research Systems, Wilmington, NC) was performed on each rabbit to determine respiratory capacity.68 Unanesthetized rabbits subsequently were challenged in a head-only chamber for approximately 10 min by using an aerosol of B. anthracis spores created by a 3-jet nebulizer (Collison model, BGI, Waltham, MA) and controlled by an automated bioaerosol exposure system.20,68 The concentration of aerosolized B. anthracis in the chamber was determined by constant sampling with an all-glass impinger (Ace Glass, Vineland, NJ) containing sterile water. Spore concentration was determined by plating on tryptic soy agar (Remel, Lenexa, KS). Rabbits were exposed to 300 times the median lethal dose (1 LD50 = 105,000 cfu) of aerosolized B. anthracis spores; this dose greatly exceeds the aerosol LD99 for B. anthracis in rabbits.69 Aerosols mimic the route of infection expected for future bioterrorism attacks5,36,55, and result in diffuse bronchopneumonia.4,18 Aerosolized B. anthracis challenges occurred in a class III biologic safety cabinet situated within an approved, restricted-access Biologic Safety level 3 laboratory suite at the United States Army Medical Research Institute of Infectious Diseases (Fort Detrick, MD).
Bacteremia.
Whole-blood samples were collected in Wampole isolator microbial tubes (Inverness Medical, Princeton, NJ) and immediately cultured on tryptic soy agar. Plates (in duplicate) were incubated for 18 to 24 h at 37 °C and then evaluated for colonies.
Clinical observations.
After saline or LPS administration, rabbits were observed and scored at least twice daily for changes in appearance (for example, coat condition, respiration, and body posture), natural behavior (for example, mobility, alertness, food intake, and vocalization), and provoked behavior (for example, response to handling). Each category was ranked on an ascending numerical order from 0 (normal) to 2 (listless, abdominal or open mouth breathing) for the appearance category; 0 (normal) to 3 (vocalization, decreased mobility and alertness) for the natural behavior category; and 0 (normal) to 3 (unresponsive when stimulated, weak, precomatose) for the provoked behavior category. These categorical scores were summed to obtain the total clinical score. When a clinical score was 4 to 6, the frequency of observations was increased to at least 3 times daily, to ensure careful monitoring of the disease progression and animal welfare. Rabbits meeting the predetermined clinical score of 7 to 8 were deemed moribund and euthanized.
Histopathologic evaluation.
Similar to a previous study,61 all B. anthracis-exposed rabbits underwent complete necropsy in a designated Biologic Safety level 3 necropsy suite, and gross findings were recorded. Representative tissue sections were immersion-fixed in 10% neutral buffered formalin (LabChem, Pittsburgh, PA) for 21 d and processed for histologic analysis.50,61 Lungs were inflated with 10% neutral buffered formalin before fixation. Paraffin-embedded tissue sections were cut at 5 to 6 µm and stained with hematoxylin and eosin (Poly Scientific R and D, Bay Shore, NY).69 Anthrax bacilli were stained in selected tissue by using the Gram–Twort staining method.61 A board-certified veterinary pathologist (NAT) reviewed all slides and was blinded to the treatment groups. Each histopathologic finding was scored individually (0, no change; 1, minimal; 2, moderate; and 3, severe) according to the distribution and extent of tissue injury.
Statistical analysis.
SigmaPlot (version 11.0, Systat Software, Chicago, IL) was used for all analyses; results are expressed as mean ± SEM. Data expressed as percentages underwent arcsine square root transformations before analysis. All correlations were analyzed by using Pearson product–moment correlations. Data for single comparisons were analyzed by using the Student t test with Bonferroni correction applied. Multiple comparisons of homogenous data were analyzed by one-way ANOVA, and group means were compared by using the Student Newman–Keuls post hoc test. Survival curves between B. anthracis-challenged rabbits pretreated with saline or LPS were analyzed by the log-rank test. The criterion for significance for Bonferroni-corrected t tests was a P value of 0.004 or less, whereas the criterion for significance for all other comparisons was a P value of 0.05 or less.
Results
LPS dose determination.
Sixteen Bordetella-free, Pasteurella-free SPF New Zealand white rabbits (male, 8; female, 8) were injected intravenously with either saline or LPS daily for 1 or 2 d. LPS doses evaluated were 6000, 12,000, and 60,000 EU/kg. Blood was collected at 90 min after saline or LPS administration to assess tissue injury and inflammatory response. No significant increase in ALT, AST, or LDH activity was observed between saline-treated and LPS-treated rabbits at any of the dosing regimens investigated (ALT: day 1, P = 0.357; day 2, P = 0.219; AST: day 1, P = 0.129; day 2, P = 0.215; LDH: day 1, P = 0.946; day 2, P = 0.982). Although a treatment-dependent increase in serum TNFα levels after the first daily LPS administration was observed for all LPS-treated compared with saline-treated rabbits, only an LPS dose of 60,000 EU/kg significantly (P = 0.004) increased serum TNFα levels (after saline, 0.057 ± 0.0043 ng/mL TNFα; 6000 EU/kg LPS, 6.65 ± 0.34 ng/mL TNFα; 12,000 EU/kg LPS, 10.66 ± 1.80 ng/mL TNFα; 60,000 EU/kg LPS, 25.87 ± 2.96 ng/mL TNFα). Serum TNFα levels were not elevated in any of the LPS-treated compared with saline-treated rabbits after the second LPS administration (data not shown).
Pyrexia, a pathophysiologic marker of systemic inflammation or infection, occurred approximately 1 h after LPS administration and continued for several hours before resolving. Whereas all rabbits that received LPS at 60,000 EU/kg developed transient pyrexia, the occurrence of pyrexia was sporadic in rabbits administered lower LPS doses. Regardless, all LPS-treated rabbits exhibited short-term, mild clinical responses after LPS administration. These clinical signs included lethargy, rough coats, and other minor changes, such as diarrhea. Within a day of the last LPS administration, rabbits were clinically normal and remained so until euthanasia at 7 d after LPS exposure.
Effect of LPS-induced inflammation on B. anthracis infection.
Saline or LPS (60,000 EU/kg) was administered intravenously to 18 Bordetella-free, Pasteurella-free SPF rabbits (male, 9; female, 9) 24 h before challenge with aerosolized B. anthracis spores. Similar to the procedure in the LPS dose-determination study, blood was collected 90 min after saline or LPS administration to assess tissue injury and inflammatory response. Although serum TNFα levels increased significantly (P ≤ 0.001) in LPS-pretreated compared with saline-pretreated rabbits (that is, 34.52 ± 4.67 compared with 0.054 ± 0.0018 ng/mL, respectively) and thus confirmed an LPS-induced inflammatory response, LDH levels did not differ between LPS- and saline-pretreated rabbits (that is, 69.4 ± 7.7 compared with 62.3 ± 2.1 IU/L, respectively). Transient pyrexia was observed approximately 1 h after LPS administration and continued for several hours before resolving. Rabbits were not pyrexic immediately before exposure to B. anthracis spores.
At 24 h after intravenous administration of saline or LPS, rabbits were challenged with approximately 300 LD50 aerosolized B. anthracis (Ames strain) spores. Specifically, saline-pretreated rabbits were exposed to a presented inhaled dose of 246.5 ± 33.4 LD50 (range, 127.7 to 445.5 LD50), whereas LPS-pretreated rabbits were exposed to a presented inhaled dose of 293.7 ± 19.7 LD50 (range, 207.8 to 380.0 LD50). The presented doses did not differ significantly between the 2 groups (Table 1).
Table 1.
Disease course for New Zealand white rabbits pretreated with saline or LPS and then challenged with aerosolized B. anthracis spores
| Saline | LPS | ||
| LD50 | |||
| Mean | 246.5 ± 33.4 | 293.7 ± 19.7 | |
| Range | 127.7–445.5 | 207.8–380 | |
| Occurrence of anthrax-induced pyrexiaa | |||
| Mean | 24.8 ± 1.5 | 66.3 ± 12.1b | |
| Range | 15.8–29.8 | 34.8–130.5 | |
| Occurrence of bacteremiaa | |||
| Mean | 25.9 ± 2.0 | 62.5 ± 11.8b | |
| Range | 15.0–39.0 | 37.5–123 | |
| Length of survivala | |||
| Mean | 40.5 ± 2.6 | 89.6 ± 13.6b | |
| Range | 31.3–56.3 | 43.8–162.5 |
Rabbits were pretreated with saline or LPS (60,000 EU/kg) and then challenged 24 h later with approximately 300 LD50 aerosolized B. anthracis spores.
Time (h) after B. anthracis challenge.
Value significantly (P < 0.004) different from that of saline-pretreated, B. anthracis-challenged rabbits.
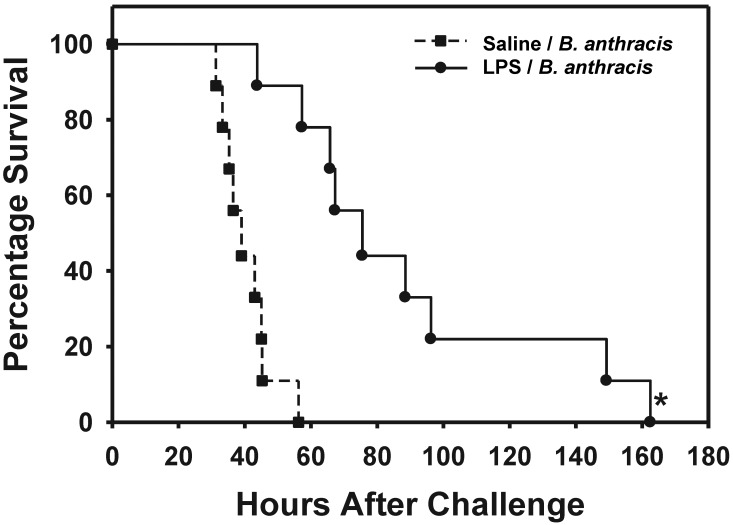
After aerosolized B. anthracis spore exposure, bacteremia—the ‘gold standard’ for systemic infection—either preceded or occurred at relatively the same time as did anthrax-induced pyrexia in both saline- and LPS-pretreated rabbits. However, development of both bacteremia and anthrax-induced pyrexia was significantly (P = 0.001 and P ≤ 0.001, respectively) delayed in LPS-pretreated compared with saline-pretreated rabbits after exposure to B. anthracis. Bacteremia and pyrexia occurred at 25.9 ± 2.0 h (range, 15.0 to 39.0 h) and 24.8 ± 1.5 h (range, 15.8 to 29.8 h) after B. anthracis challenge, respectively, in saline-pretreated rabbits but at 62.5 ± 11.8 h (range, 37.5 to 123.0 h) and 66.3 ± 12.1 h (range, 34.8 to 130.5 h), respectively, in LPS-pretreated rabbits. Survival time after B. anthracis exposure was significantly (P = 0.001) prolonged for LPS-pretreated rabbits (mean, 89.6 ± 13.6 h; range, 43.8 to 162.5 h) compared with saline-pretreated rabbits (mean, 40.5 ± 2.6 h; range, 31.3 to 56.3 h). A slight, but nonsignificant increase (per Bonferroni-corrected t test; P = 0.01) in survival time after bacteremia was observed for LPS-pretreated rabbits (27.1 ± 3.8 h; range, 6.3 to 39.5 h) in comparison with saline-pretreated rabbits (14.6 ± 1.8 h; range, 3.3 to 20.3 h). Therefore, the onset of anthrax and the duration of survival after B. anthracis challenge were significantly increased in LPS-treated compared with saline-pretreated rabbits (Table 1, Figure 1). Consistent with previous findings,68 we noted no correlation between the presented inhaled dose of B. anthracis spores and postchallenge survival time for either saline-pretreated or the LPS-pretreated rabbits. Moreover, there was no significant difference in the survival time after B. anthracis challenge between saline-pretreated and naïve New Zealand white rabbits.68 Regardless of the pretreatment, all B. anthracis-exposed rabbits eventually succumbed to inhalational anthrax (Table 2).
Figure 1.
Percentage survival for New Zealand white rabbits (n = 9 per group) pretreated with either saline (vehicle) or LPS (60,000 EU/kg) and then challenged 24 h later with approximately 300 LD50 of aerosolized B. anthracis spores. *, Value significantly (P ≤ 0.001) different from that in saline-treated, B. anthracis-challenged rabbits.
Table 2.
Semiquantitative histopathologic analysis of New Zealand white rabbits pretreated with saline or LPS and then challenged with aerosolized B. anthracis spores
| Saline | LPS | |
| Lung | 2.6 ± 0.2 | 2.4 ± 0.2 |
| Splenitis | 3.0 ± 0.0 | 3.0 ± 0.0 |
| Lymphadenitis of mediastinal lymph node | 3.0 ± 0.0 | 3.0 ± 0.0 |
| Adenitis of adrenal gland | 1.7 ± 0.3 | 1.4 ± 0.3 |
| Mediastinum | 1.4 ± 0.4 | 1.7 ± 0.3 |
| Renal tubular necrosis | 2.0 ± 0.0 | 2.0 ± 0.0 |
Rabbits were pretreated with saline or LPS (60,000 EU/kg) and then challenged 24 h later with approximately 300 LD50 aerosolized B. anthracis spores. Rabbits either succumbed to inhalational anthrax or were euthanized. Histopathologic finding was graded individually on a severity scale of 0 (none), 1 (minimal), 2 (moderate), and 3 (severe) according to the distribution and extent of tissue injury.
Clinical observations and pathology in B. anthracis-challenged New Zealand white rabbits.
Similar to previous reports,68,69 B. anthracis-challenged rabbits appeared clinically normal until shortly before succumbing to inhalational anthrax. Moribund rabbits were lethargic, weak, and subject to respiratory distress. All moribund rabbits were euthanized. No clear, consistent pattern in the overall clinical observations for B. anthracis-challenged rabbits could be elucidated as a predictor for infection or state of pathogenesis (data not shown).
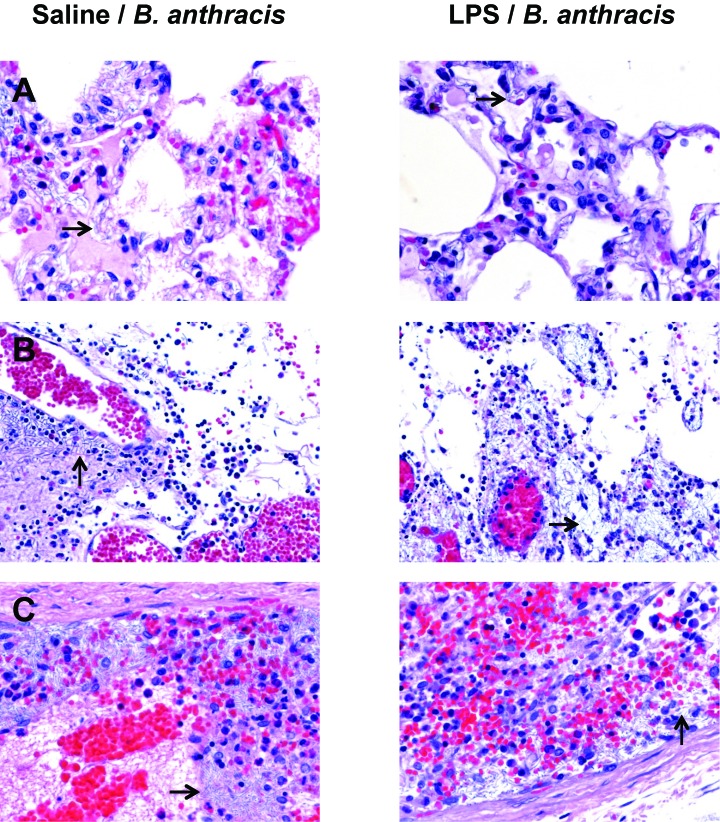
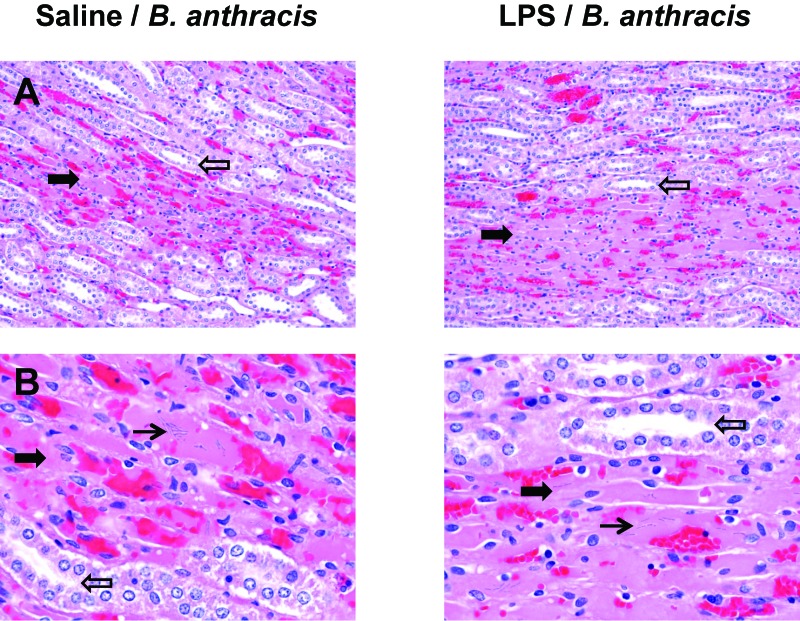
The resultant pathology for both saline-pretreated and LPS-pretreated, B. anthracis-challenged rabbits was consistent with inhalational anthrax in rabbits as previously described.69 Bacilli were identified histologically within blood vessels of multiple organs and tissues in all animals, indicating that severe bacteremia was present at the time of death. Histologic lesions in all B. anthracis-exposed rabbits were generally consistent and included acute necrotizing splenitis, necrotizing lymphadenitis of the mediastinal lymph node, mediastinitis, pneumonia, adenitis of the adrenal gland, renal tubular necrosis, and congestion and edema in multiple tissues. A semiquantitative comparison between saline-pretreated and LPS-pretreated B. anthracis-challenged rabbits revealed no differences between the severity of histologic lesions, based on distribution and extent of injury, for lungs, mediastinum (for example, mediastinitis), acute necrotizing splenitis, lymphadenitis of the mediastinal lymph node, adenitis of the adrenal gland, and renal tubular necrosis (Table 2, Figure 2). In particular, lungs from both saline-pretreated and LPS-pretreated B. anthracis-challenged rabbits exhibited acute interstitial pneumonia with abundant alveolar edema (Figure 2 A). Multifocal disruption of the alveolar interstitium was apparent throughout, diffusely expanded by myriad bacilli, heterophils, necrotic cellular debris, and fibrin. Acute mediastinitis was observed, with multifocal expansion of mediastinal tissues (Figure 2 B) through the presence of hemorrhage, edema, fibrin inflammatory cells (for example, heterophils), necrotic cellular debris, and bacilli. Severe destruction of the spleen (Figure 2 C) was present in both groups of rabbits. Diffuse loss of the white pulp in the spleen, characterized by an overall lack of basophilic lymphocytes, was observed. The spleen exhibited a pronounced presence of bacilli admixed with hemorrhage, fibrin, and necrotic cellular debris. Lastly, renal tubular necrosis (Figure 3 A, B) was evident in both saline-pretreated and LPS-pretreated B. anthracis-challenged rabbits. Necrotic tubules were identified by hypereosinophilia, lack of basophilic circular nuclei, and collapsed tubular lumen. Hemorrhage and B. anthracis bacilli were apparent among the necrotic tubules. Photomicrographs of renal injury from aerosolized B. anthracis-exposed rabbits have not been published previously.69
Figure 2.
Representative photomicrographs of lung, mediastinum, and spleen from New Zealand white rabbits pretreated with saline (vehicle) or LPS (60,000 EU/kg) and then challenged 24 h later with approximately 300 LD50 of aerosolized B. anthracis spores. (A) Lungs exhibited acute interstitial pneumonia with abundant alveolar edema. Multifocal disruption of the alveolar interstitium, hemorrhage and the presence of B. anthracis bacilli (arrow) are apparent. Hematoxylin and eosin stain; magnification, 60×. (B) Mediastinum has been multifocally expanded by hemorrhage, edema, inflammatory cells, necrotic cellular debris and bacilli (arrow). Hematoxylin and eosin stain; magnification, 40×. (C) Spleen exhibited severe disruption with diffuse loss of white pulp, characterized by an overall lack of basophilic lymphocytes, and the presence of myriad bacilli (arrow) admixed with hemorrhage, fibrin, and necrotic cellular debris. Hematoxylin and eosin stain; magnification, 60×.
Figure 3.
Representative photomicrographs of kidney from New Zealand white rabbits pretreated with saline (vehicle) or LPS (60,000 EU/kg) and then challenged 24 h later with approximately 300 LD50 of aerosolized B. anthracis spores. (A) At 20× magnification, the kidney revealed areas of acute necrosis of the renal tubules (wide solid arrow) with adjacent normal tubules (wide open arrow) apparent. (B) Acutely necrotic renal tubules (wide solid arrow) are homogenously hypereosinophilic, lack nuclei, and have collapsed lumens (normal tubules, open arrow). Hemorrhage and the presence of bacilli (arrow) are also apparent among the necrotic tubules. Magnification, 60×. Hematoxylin and eosin stain.
Discussion
The development of medical countermeasures to many biothreat agents, including aerosolized B. anthracis spores, relies heavily on well-characterized animal models to predict disease pathogenesis and treatment efficacy in humans (US Food and Drug Administration's Animal Efficacy Rule, 21 CFR 314.610 and 21 CFR601.91).29,56 Both an animal's initial state of health (that is, use of an unhealthy animal compared with a healthy one) and its source (for example, conventional compared with SPF) may affect the interpretation of results from characterization and medical countermeasure studies.19,23,53 Similar to previous findings,13,30 we demonstrate that LPS-induced activation of the innate immune system—such as would occur during infection—of healthy SPF New Zealand white rabbits results in transient host resistance to B. anthracis infection (Table 1, Figure 1). LPS pretreatment significantly delayed the onset of inhalational anthrax and prolonged survival after B. anthracis exposure but did not alter the ultimate lethal outcome or pathology of the disease in New Zealand white rabbits.
The proinflammatory properties of LPS are due to its interaction with the Toll-like receptor 4 pathways which activates innate immune cells (such as macrophages, monocytes, and neutrophils) and releases proinflammatory mediators including TNFα, interferon γ, interleukin 1, interleukin 6, and various chemokines.6,22 In the present investigation, a limited dose-range study was conducted in New Zealand white rabbits to determine an LPS dose that provoked an inflammatory reaction, as indicated by pyrexia and increased TNF-α levels, but that would be insufficient to cause overt tissue injury. No increase in serum LDH, ALT, and AST activity, markers of tissue injury, occurred 90 min after LPS exposure at any of the LPS doses (ranging from 6000 to 60,000 EU/kg; equivalent to 0.6 to 6 µg/kg United States standard endotoxin) evaluated, indicating that these doses were noninjurious. Furthermore, when a second LPS dose was given a day later, serum LDH, ALT, and AST activities in LPS-treated rabbits did not differ from that observed in control animals. Although it is possible that increased serum LDH, ALT, or AST activity occurred after the first day's blood collection time, any increase was transient and had returned to normal levels by the next day. Only the LPS dose of 60,000 EU/kg resulted in consistent transient pyrexia, significantly increased TNFα levels, and no overt tissue injury. Interestingly, a second daily LPS dose (60,000 EU/kg) did not evoke increased TNFα levels, possibly suggesting a tolerance effect.32,33 Alternatively, this diminished LPS response may be due to increased presence of acute-phase proteins that induce the binding of LPS to LPS-binding protein or high-density lipoproteins, thereby decreasing LPS activity.60,67
Optimal increased host resistance to bacterial infection has been reported in mouse and rat models when either low-dose LPS or another activator of the innate immune system was administered 24 h prior to lethal bacterial infection, with lesser protection observed at shorter and longer (up to 72 h) intervals.7,8,13,25,38,65 Accordingly, in the present study, an LPS dose of 60,000 EU/kg was administered 24 h prior to lethal B. anthracis spore exposure (approximately 300 LD50). Significant delays in both anthrax-induced pyrexia and bacteremia occurred in LPS-pretreated compared with saline-pretreated rabbits, indicating that prior activation of the innate immune system delays the onset of anthrax infection (Table 1, Figure 1). Survival after bacteremia was slightly prolonged in LPS-pretreated rabbits compared with saline-pretreated rabbits. However, the overall increased survival time for LPS-pretreated rabbits after B. anthracis exposure more likely was due to the delayed onset of inhalational anthrax rather than to the prolonging of symptomatic anthrax, given that as the survival time after bacteremia for both LPS- and saline-pretreated rabbits did not differ significantly from the survival time after bacteremia that was observed for naive B. anthracis-exposed rabbits.68 Consistent with previous results,68 both saline- and LPS-pretreated rabbits appeared clinically normal until shortly before they died from inhalational anthrax. The resultant pathology was consistent for rabbits that died due to inhalational anthrax, with no observable histopathologic differences between the 2 pretreated groups (Table 2, Figures 2 and 3).62,68 Because pathologic evaluation occurred at the late stage of the disease, early pathologic changes in the current study are unknown. However, early unique pathology may have existed in LPS-pretreated animals and may not have been apparent when the animal died or was euthanized. Overall, these results suggest that prior activation of the innate immune system causes transient host resistance to lethal B. anthracis infection in rabbits. Although pretreatment with LPS did not prevent B. anthracis-exposed rabbits from ultimately dying from the disease, it significantly delayed the onset of inhalational anthrax and thereby prolonged survival after exposure to aerosolized B. anthracis spores.
The mechanism through which LPS enhances host resistance to subsequent bacterial infection has not been defined fully but likely involves macrophage activation and the induction of inflammatory mediators.7,17,32,44,65 After inhalation, B. anthracis spores are ingested by alveolar macrophages and possibly other phagocytic cells. The spores germinate within the phagolysosomes, and a minority of the germinating spores escape the host phagocyte to establish an extracellular infection that leads to toxemia, septicemia, and death.12,47 Although macrophages serve as a vehicle for spore germination, macrophages have been shown in vitro to have sporicidal activity; in a mouse model, both macrophages and neutrophils (although to a lesser extent perhaps) had an early protective role in B. anthracis-infected hosts.10,11,34,43 Moreover, a recent study12 found that increased levels of interferon-inducible CXC chemokines (namely, CXCL9, CXCL10, and CXCL11, which are produced by monocytes and macrophages after stimulation by proinflammatory cytokines, such as interferon γ) significantly reduced spore germination within the lung, thereby suggesting that these chemokines have an antimicrobial role against B. anthracis spores and bacilli. Therefore, a putative mechanism is that pretreatment with LPS not only activates macrophages and (perhaps) neutrophils to attack B. anthracis spores and bacilli directly but also (direct or indirectly) causes the production of various cytokines (such as interferons), antimicrobial chemokines, and polypetides that reduce spore germination and thereby transiently increase host resistance to subsequent B. anthracis infection by delaying the onset of inhalational anthrax.7,12,,35,43,49,66 Additional studies are required to determine the exact mechanism through which LPS-pretreatment in rabbits beneficially prolongs survival after B. anthracis challenge. Studies also are needed to elucidate how changes in the interval between challenge and LPS treatment (before and after challenge) affect this transient protection.
Animal health plays an important role in the interpretation of results from animal models of disease.19,23,53,59 Our finding that prior or underlying activation of the innate immune system prolongs survival in the rabbit model of inhalational anthrax emphasizes the importance of knowing an animal's health status before study initiation. In this regard, the use of unhealthy rabbits (for example, infected) may be responsible for confounding data in studies characterizing inhalational anthrax and the efficacy of potential therapeutic strategies. Moreover, although the disease outcome is the same, subtle differences in the pathogenesis of inhalational anthrax may occur in animals with a prior or underlying infection that would not occur in a healthy animal. As previously noted, conventionally sourced New Zealand white rabbits, which may be colonized with many common gram-negative bacteria such as Pasteurella and Bordetella, or rabbits that are not certified as Bordetella- and Pasteurella-free appear to have a longer survival time after B. anthracis exposure than do Bordetella-free, Pasteurella-free SPF-sourced rabbits.26,42,68 The mean duration of survival after B. anthracis challenge for LPS-pretreated rabbits was similar to that of B. anthracis-challenged conventionally sourced rabbits and B. anthracis-challenged rabbits that were not certified as Bordetella- and Pasteurella-free, raising the possibility that differences in survival time between these animal sources may be, in part, due to activation of the innate immune system by exogenous pathogens such as Pasteurella and Bordetella.9,26,41,68 Additional studies are needed to determine whether Bordetella and Pasteurella infection cause transient host resistance to inhalational anthrax.
Although bacterial infection is the primary source of systemic LPS exposure, modest exposure may occur when LPS is released from the predominantly gram-negative indigenous flora of the rabbit gastrointestinal lumen and translocates into the circulation; increased translocation may occur due to changes in diet, gastrointestinal distress, and disease.14,52,64 Therefore, increased endogenous LPS levels may lead to transient activation of the innate immune system and affect resistance to B. anthracis infection. This effect of endogenous LPS may account for some of the variability in survival observed within individual inhalational anthrax studies for rabbits and nonhuman primates.9,28,42,51,68
In summary, the present study demonstrates that prior or underlying stimulation of the innate immune system significantly delays the onset of inhalational anthrax and thereby prolongs survival after B. anthracis exposure. Specifically, prior administration of a noninjurious dose of LPS to New Zealand white rabbits transiently increased host resistance to lethal challenge with aerosolized Ames strain B. anthracis spores. Activation of the innate immune system, perhaps by LPS or by a similar Toll-like receptor 4 agonist, potentially may be useful for delaying the onset of anthrax when immediate treatment for inhalational anthrax is unavailable. Overall, these results emphasize the importance of understanding animal health status (for example, free of underlying infection) to prevent confounding data from studies characterizing inhalational anthrax and evaluating potential medical countermeasures.
Acknowledgments
This research was sponsored through an interagency agreement between the National Institute of Allergy and Infectious Diseases (Y1-AI-6129-04), and the United States Army Medical Research Institute of Infectious Diseases (USAMRIID; A 120-B-10.3). The views, opinions, and/or findings contained herein are those of the authors and should not be construed as an official Department of Army position, policy, or decision unless so designated by other documentation. The authors do not have a commercial or other association that would pose a conflict of interest.
We are grateful to the staff of the Center for Aerobiological Sciences (USAMRIID) for providing aerosol challenge expertise and to Sarah Norris of the Research Support Division (USAMRIID) for statistical advice. We also thank Joshua Moore and the Veterinary Medicine (USAMRIID) technicians for expert animal care and veterinary assistance. Finally, we are grateful to Drs Judith Hewitt and Raymond Slay (National Institute of Allergy and Infectious Diseases) for manuscript review.
References
- 1.Anderson IE, Buxton D, Campbell I, Russell G, Davis WC, Hamilton MJ, Haig DM. 2007. Immunohistochemical study of experimental malignant catarrhal fever in rabbits. J Comp Pathol 136:156–166 [DOI] [PubMed] [Google Scholar]
- 2.Animal Welfare Act as Amended. 2008. 7 USC §2131-2159.
- 3.Animal Welfare Regulations. 2009. 9 CFR §2.30–2.38 and 3.50–3.66.
- 4.Bakker-Woudenberg IAJM. 2003. Experimental model of pulmonary infection. J Microbiol Methods 54:295–313 [DOI] [PubMed] [Google Scholar]
- 5.Bouzianas DG. 2007. Potential biological targets of Bacillus anthracis in antiinfective approaches against the threat of bioterrorism. Expert Rev Anti Infect Ther 5:665–684 [DOI] [PubMed] [Google Scholar]
- 6.Bryant CE, Spring DR, Gangloff M, Gay NJ. 2010. The molecular basis of the host response to lipopolysaccharide. Nat Rev Microbiol 8:8–14 [DOI] [PubMed] [Google Scholar]
- 7.Clement CG, Evans SE, Evans CM, Hawke D, Kobayashi R, Reynolds PR, Moghaddam SJ, Scott BL, Melicoff E, Adachi R, Dickey BF, Tuvim MJ. 2008. Stimulation of lung innate immunity protects against lethal pneumococcal pneumonia in mice. Am J Respir Crit Care Med 177:1322–1330 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cluff CW, Baldridge JR, Stover AG, Evans JT, Johnson DA, Lacy MJ, Clawson VG, Yorgensen VM, Johnson CL, Livesay MT, Hershberg RM, Pershing DH. 2005. Synthetic Toll-like receptor agonists stimulate innate resistance to infectious challenge. Infect Immun 73:3044–3052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Comer JE, Ray B, Henning LN, Stark GV, Barnewall RE, Mott JM, Meister GT. 2012. Characterizing a therapeutic model of inhalational anthrax using an increase in body temperature as a trigger for treatment in New Zealand white rabbits. Clin Vaccine Immunol 19:1517–1525 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cote CK, Rea KM, Norris SL, Van Rooijen N, Welkos SL. 2004. The use of a model of in vivo macrophage depletion to study the role of macrophages during infection with Bacillus anthracis spores. Microb Pathog 37:169–175 [DOI] [PubMed] [Google Scholar]
- 11.Cote CK, van Rooijen N, Welkos SL. 2006. Role of macrophages and neutrophils in the early host response to Bacillus anthracis spores in a mouse model of infection. Infect Immun 74:469–480 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Crawford MA, Zhu Y, Green CS, Burdick MD, Sanz P, Alem F, O'Brien AD, Mehrad B, Strieter RM, Hughes MA. 2009. Antimicrobial effects of interferon-inducible CXC chemokines against Bacillus anthracis spores and bacilli. Infect Immun 77:1664–1678 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Evans SE, Scott BL, Clement CG, Larson DT, Kontoyiannis D, Lewis RE, LaSala PR, Pawlik J, Peterson JW, Chopra AK, Klimpel G, Bowden G, Hook M, Xu Y, Tuvim MJ, Dickey BF. 2010. Stimulated innate resistance of lung epithelium protects mice broadly against bacteria and fungi. Am J Respir Cell Mol Biol 42:40–50 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fann MK, O'Rourke D. 2001. Normal bacterial flora of the rabbit gastrointestinal tract: a clinical approach. Semin Avian Exot Pet Med 10:45–47 [Google Scholar]
- 15.Fujiki T, Kutsukake H, Imai K, Tanaka A. 1988. Protection of mice against bacterial infection by oral administration of bacterial lipopolysaccharide. Microbiol Immunol 32:1253–1258 [DOI] [PubMed] [Google Scholar]
- 16.Goossens PL. 2009. Animal models of human anthrax: the quest for the Holy Grail. Mol Aspects Med 30:467–480 [DOI] [PubMed] [Google Scholar]
- 17.Hackett CJ. 2003. Innate immune activation as a broad-spectrum biodefense strategy: prospects and research challenges. J Allergy Clin Immunol 112:686–694 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Halperin SA, Heifetz SA, Kasina A. 1988. Experimental respiratory infection with Bordetella pertusis in mice: comparison of 2 methods. Clin Invest Med 11:297–303 [PubMed] [Google Scholar]
- 19.Hansen AK. 1999. The impact of general laboratory animal health on experimental models of antimicrobial therapy, p 49–60. In: Zak O, Sande M. Handbook of animal models of infection. London (UK): Academic Press. [Google Scholar]
- 20.Hartings JM, Roy CJ. 2004. The automated bioaerosol exposure system: preclinical development and a respiratory dosimetry application with nonhuman primates. J Pharmacol Toxicol Methods 49:39–55 [DOI] [PubMed] [Google Scholar]
- 21.Hewett JA, Jean PA, Kunkel SL, Roth RA. 1993. Relationship between tumor necrosis factor α and neutrophils in endotoxin-induced liver injury. Am J Physiol 265:G1011–G1015 [DOI] [PubMed] [Google Scholar]
- 22.Hewett JA, Roth RA. 1993. Hepatic and extrahepatic pathobiology of bacterial lipopolysaccharides. Pharmacol Rev 45:382–411 [PubMed] [Google Scholar]
- 23.Hickey TE. 1997. Animal care and use in toxicity testing, p 85–100. In: Williams PD, Hottendorf GH. Comprehensive toxicology, vol 2. New York (NY): Elsevier. [Google Scholar]
- 24.Inglesby TV, O'Toole T, Henderson DA, Bartlett JG, Ascher MS, Eitzen E, Friedlander AM, Gerberding J, Hauer J, Hughes J, McDade J, Osterholm MT, Parker G, Perl TM, Russell PK, Tonat K. 2002. Anthrax as a biological weapon, 2002: updated recommendations for management. JAMA 287:2236–2252 [DOI] [PubMed] [Google Scholar]
- 25.Jean D, Rezaiguila-Delclaux S, Delacourt C, Leclercq R, Lafuma C, Brun-Buisson C, Harf A, Delclaux C. 1998. Protective effect of endotoxin instillation on subsequent bacteria-induced lung injury in rats. Am J Respir Crit Care Med 158:1702–1708 [DOI] [PubMed] [Google Scholar]
- 26.Kobiler D, Weiss S, Levy H, Fisher M, Mechaly A, Pass A, Zeev A. 2006. Protective antigen as a correlative marker for anthrax in animal models. Infect Immun 74:5871–5876 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lawrence WS, Hardcastle JM, Brining DL, Weaver LE, Ponce C, Whorton EB, Peterson JW. 2009. The physiologic response of Dutch belted rabbits infected with inhalational anthrax. Comp Med 59:257–265 [PMC free article] [PubMed] [Google Scholar]
- 28.Leffel EK, Bourdage JS, Williamson ED, Duchars M, Fuerst TR, Fusco PC. 2012. Recombinant protective antigen anthrax vaccine improves survival when administered as a postexposure prophylaxis countermeasure with antibiotic in the New Zealand white rabbit model of inhalational anthrax. Clin Vaccine Immunol 19:1158–1164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Leffel EK, Pitt LM. 2012. Characterization of new and advancement of existing animal models of Bacillus anthracis infection, p 81–98. In: Swearengen JR, editor. Biodefense: research methodology and animal models, 2nd ed. Boca Raton (FL): CRC Press. [Google Scholar]
- 30.Leffel EK, Twenhafel NA, Whitehouse CA. 2008. Nosocomial infection of Serratia marcescens may induce a protective effect in monkeys exposed to Bacillus anthracis. J Infect 57:162–164 [DOI] [PubMed] [Google Scholar]
- 31.Leighton TJ, Doi RH. 1971. The stability of messenger ribonucleic acid during sporulation in Bacillus subtilis. J Biol Chem 246:3189–3195 [PubMed] [Google Scholar]
- 32.Lehner MD, Hartung T. 2002. Endotoxin tolerance—mechanisms and beneficial effects in bacterial infection. Rev Physiol Biochem Pharmacol 144:95–141 [DOI] [PubMed] [Google Scholar]
- 33.Lehner MD, Ittner J, Bundschuh DS, van Rooijen N, Wendel A, Hartung T. 2001. Improved innate immunity of endotoxin-tolerant mice increases resistance to Salmonella enteric serovar typhimurium infection despite attenuated cytokine response. Infect Immun 69:463–471 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lisanby MW, Swiecki MK, Dizon BL, Pflughoeft KJ, Koehler TM, Kearney JF. 2008. Cathelicidin administration protects mice from Bacillus anthracis spore challenge. J Immunol 181:4989–5000 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Loos T, Dekeyzer L, Struyf S, Schutyser E, Gijsbers K, Gouwy M, Fraeyman A, Put W, Ronsse I, Grillet B, Opdenakker G, Van Damme J, Proost P. 2006. TLR ligands and cytokines induce CXCR3 ligands in endothelial cells: enhanced CXCL9 in autoimmune arthritis. Lab Invest 86:902–916 [DOI] [PubMed] [Google Scholar]
- 36.Loving CL, Kennett M, Lee GM, Grippe VK, Merkel TJ. 2007. Murine aerosol challenge model of anthrax. Infect Immun 75:2689–2698 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lu M, Varley AW, Ohta S, Hardwick J, Munford RS. 2008. Host inactivation of bacterial lipopolysaccharide prevents prolonged tolerace from gram-negative bacterial infection. Cell Host Microbe 4:293–302 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Mann PB, Wolfe D, Latz E, Golenbrock D, Preston A, Harvill ET. 2005. Comparative Toll-like receptor 4-mediated innate host defense to Bordetella infection. Infect Immun 73:8144–8152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Manning PJ, Ringer DH, Newcomer CE. 1994. The biology of the laboratory rabbit. New York (NY): Academic Press [Google Scholar]
- 40.Martin GJ, Friedlander AM. 2010. Anthrax as an agent of bioterrorism, p 3983–3992. In: Mandell GL, Bennett JE, Dolin R. Mandell, Douglas, and Bennett's principles and practice of infectious disease, vol 2. Philadelphia (PA): Elsevier. [Google Scholar]
- 41.Mayeux PR. 1997. Pathophysiology of lipopolysaccharide. J Toxicol Environ Health 51:415–435 [DOI] [PubMed] [Google Scholar]
- 42.Migone T-S, Subramanian GM, Zhong J, Healey LM, Corey A, Devalaraja M, Lo L, Ullrich S, Zimmerman J, Chen A, Lewis M, Meister G, Gillum K, Sanford D, Mott J, Bolmer SM. 2009. Raxibacumab for the treatment of inhalational anthrax. N Engl J Med 361:135–144 [DOI] [PubMed] [Google Scholar]
- 43.Moayeri M, Crown D, Newman ZL, Okugawa S, Eckhaus M, Cataisson C, Liu S, Sastalla I, Leppla SH. 2010. Inflammasome sensor Nlrp1b-dependent resistance to anthrax is mediated by caspase 1, IL1 signaling, and neutrophil recruitment. PLoS Pathog 6:e1001222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Muthukkumar S, Muthukkaruppan VR. 1993. Mechanism of protective immunity by porin-lipopolysaccharide against murine salmonellosis. Infect Immun 61:3017–3025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Institute for Laboratory Animal Research 2011. Guide for the care and use of laboratory animals, 8th ed. Washington (DC): National Academies Press [Google Scholar]
- 46.Office of Laboratory Animal Welfare. [Internet] 2002. Public health service policy on humane care and use of laboratory animals. Available at: http://grants.nih.gov/grants/olaw/references/phspol.htm
- 47.Passalacqua KD, Bergman NH. 2006. Bacillus anthracis: interactions with the host and establishment of inhalational anthrax. Future Microbiol 1:397–415 [DOI] [PubMed] [Google Scholar]
- 48.Phipps AJC, Premanandan C, Barnewall RE, Lairmore MD. 2004. Rabbits and nonhuman primate models of toxin-targeting human anthrax vaccines. Microbiol Mol Biol Rev 68:617–629 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Pickering AK, Osorio M, Lee GM, Grippe VK, Bray M, Merkel TJ. 2004. Cytokine response to infection with Bacillus anthracis spores. Infect Immun 72:6382–6389 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Prophet EB, Mills B, Arrington JB, Sobin LA. 1992. Armed Forces institute of pathology: laboratory methods in histotechnology. Washington (DC): American Registry of Pathology [Google Scholar]
- 51.Rossi CA, Ulrich M, Norris S, Reed DS, Pitt LM, Leffel EK. 2008. Identification of a surrogate marker for infection in the African green monkey model of inhalation anthrax. Infect Immun 76:5790–5801 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Roth RA, Harkema JR, Pestka JP, Ganey PE. 1997. Is exposure to bacterial endotoxin a determinant of susceptibility from xenobiotic agents? Toxicol Appl Pharmacol 147:300–311 [DOI] [PubMed] [Google Scholar]
- 53.Rouse MS, Wilson WR. 1999. General methodologies for animal models, p 9–12. In: Zak O, Sande M. Handbook of animal models of infection. London (UK): Academic Press. [Google Scholar]
- 54.Sande MA, Sande ER, Woolwine JD, Hackbarth CJ, Small PM. 1987. The influence of fever on the development of experimental Streptococcus pneumoniae meningitis. J Infect Dis 156:849–850 [DOI] [PubMed] [Google Scholar]
- 55.Spencer RC. 2003. Bacillus anthracis. J Clin Pathol 56:182–187 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Steele KE, Alves DA, Chapman JL. 2007. Challenges in biodefense research and the role of the US Army Veterinary Pathologists. US Army Med Dep J Jul-Sep: 28–37. [PubMed] [Google Scholar]
- 57.Suber RL. 1989. Clinical pathology for toxicologists, p 511–514. In: Hayes AW, editor. Principles and methods of toxicology, 2nd ed. New York (NY): Raven Press. [Google Scholar]
- 58.Suckow MA, Brammer DW, Rush HG, Chrisp CE. 2002. Biology and diseases of rabbits. In: Fox JG, Anderson LC, Loew FM, Quimby FW. Laboratory animal medicine, 2nd ed. London (UK): Academic Press. [Google Scholar]
- 59.Taylor MJ, Rooney JR, Blundell GP. 1961. Experimental anthrax in the rat. II. The relative lack of natural resistance in germ-free (Lobund) hosts. Am J Pathol 38:625–638 [PMC free article] [PubMed] [Google Scholar]
- 60.Tobias PS, Ulevitch RJ. 1983. Control of lipopolysaccharide high-density lipoprotein binding by acute-phase proteins. J Immunol 131:1913–1916 [PubMed] [Google Scholar]
- 61.Twenhafel NA, Leffel E, Pitt ML. 2007. Pathology of inhalational anthrax infection in the African green monkey. Vet Pathol 44:716–721 [DOI] [PubMed] [Google Scholar]
- 62.Twenhafel NA. 2010. Pathology of inhalational anthrax animal models. Vet Pathol 47:819–830 [DOI] [PubMed] [Google Scholar]
- 63.Vaara M. 1999. Lipopolysaccharide and the permeability of the bacterial outer membrane, p 31–38. In: Brade H, Opal SM, Vogel SN, Morrison DC. Endotoxin in health and disease. New York (NY): Marcel-Dekker. [Google Scholar]
- 64.Van Leeuwen PAM, Boermeester MA, Houdjik APJ, Ferwerda CC, Cuesta MA, Meyer S, Wesdorp RIC. 1994. Clinical significance of translocation. Gut 35:S28–S34 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Vuopio-Varkila J, Nurminen M, Pyhala L, Makela PH. 1988. Lipopolysaccharide-induced nonspecific resistance to systemic Escherichia coli infection in mice. J Med Microbiol 25:197–203 [DOI] [PubMed] [Google Scholar]
- 66.Walberg K, Baron S, Poast J, Schwartz B, Izotova L, Pestka S, Peterson JW. 2008. Interferon protects mice against inhalational anthrax. J Interferon Cytokine Res 28:597–601 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Worthen GS, Avdi N, Vulkalovich S, Tobias PS. 1992. Neutrophil adherence induced by lipopolysaccharide in vitro. Role of plasma component interaction with lipopolysaccharide. J Clin Invest 90:2526–2535 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Yee SB, Hatkin JM, Dyer DN, Orr SA, Pitt MLM. 2010. Aerosolized Bacillus anthracis infection in New Zealand white rabbits: natural history and intravenous levofloxacin treatment. Comp Med 60:461–468 [PMC free article] [PubMed] [Google Scholar]
- 69.Zaucha GM, Pitt MLM, Estep J, Ivins BE, Friedlander AM. 1998. The pathology of experimental anthrax in rabbits exposed by inhalation and subcutaneous inoculation. Arch Pathol Lab Med 122:982–992 [PubMed] [Google Scholar]