Abstract
Ecopharmacovigilance (EPV) is a developing science and it is currently very unclear what it might mean in practice. We have performed a comparison between pharmacovigilance (PV) and EPV and have identified that there are similarities, but also some important differences that must be considered before any practical implementation of EPV. The biggest difference and greatest challenge concerns signal detection in the environment and the difficulty of identifying cause and effect. We reflect on the dramatic vulture decline in Asia, which was caused by the veterinary use of diclofenac, versus the relative difficulty in identifying the specific causes of intersex fish in European rivers. We explore what EPV might mean in practice and have identified that there are some practical measures that can be taken to assess environmental risks across product life cycle, particularly after launch of a new drug, to ensure that our risk assessments and scientific understanding of pharmaceuticals in the environment remain scientifically and ecologically relevant. These include:
Tracking environmental risks after launch of the product, via literature monitoring for emerging data on exposure and effects
Using Environmental Risk Management Plans (ERMPs) as a centralized resource to assess and manage the risks of a drug throughout its life cycle
Further research, testing or monitoring in the environment when a risk is identified
Keeping a global EPV perspective
Increasing transparency and availability of environmental data for medicinal products.
These measures will help to ensure that any significant environmental issues associated with pharmaceuticals in the environment (PIE) are identified in a timely way, and can be managed appropriately.
Introduction
In recent years concern has been expressed over the potential impact of pharmaceuticals in the environment (PIE) and consequently a comprehensive Environmental Risk Assessment (ERA) is now a regulatory requirement prior to launch of any new drug. However, there is no formal framework or mechanism to review the ERA, or to monitor for potential adverse effects in the environment, once a product has been launched.
Within Europe, the Pharmacovigilance Framework [1] includes a reference to the pollution of waters and soils with pharmaceutical residues and states that “Member states should consider measures to monitor and evaluate the risk of environmental effects, including those which may have an impact on public health”. This suggests that a kind of PV for the environment, or ecopharmacovigilance (EPV), should be explored.
The aim of this article is to explore what EPV might mean in practice and to discuss some of the challenges and potential opportunities that need to be faced when trying to implement EPV procedures. We also describe our approach to developing Environmental Risk Management Plans (ERMPs), which start to address some of the challenges of EPV.
What is Ecopharmacovigilance (EPV)?
Before introducing the EPV concept, some background is necessary on PIE and the ERA of pharmaceuticals.
Pharmaceuticals in the Environment
In recent years, human pharmaceuticals from numerous therapeutic classes have increasingly been detected in the environment, typically at ng/L to low μg/L in surface waters [2–17]. The potential routes of environmental entry have been extensively reviewed. These include (i) patient excretion either as parent compound or metabolites via the sewer system, (ii) direct release into the waste water system from manufacturing, hospitals or disposal via toilets/sinks, and (iii) terrestrial depositions, for example via sludge application to land, leaching from solid waste landfills, or irrigation with treated or untreated wastewaters [4, 13, 16, 18, 19].
It is generally accepted that excretion of pharmaceuticals after human and veterinary therapeutic use dominates the global input of pharmaceuticals into the environment. Manufacturing effluent discharges and the disposal of unused drugs make a relatively small contribution to the overall environmental load [8, 16, 20, 21]. Nevertheless, localized elevated drug concentrations can occur adjacent to discharges from hospitals [22] and manufacturing sites if emissions are not properly treated and controlled [23–25]. Proactive initiatives to manage pharmaceutical manufacturing and formulation wastes have been described elsewhere [26, 27]. Similarly, disposal of unused drugs is a very specific issue that can be managed effectively if the appropriate preventative methods are put in place. This may include guidance for patients, take-back schemes and disposal practices [21]. Pharmaceutical residues in the environment associated with human excretion are an inevitable consequence of patient drug use, and unlike manufacturing-related releases and unused drugs, it is a much more difficult source to control. The level of effective sewage treatment in a particular region may reduce the resulting concentrations, but there will still be some residues remaining, so the question remains as to whether or not such residues present any significant risk, and what level of residues is acceptable. This question is routinely addressed for new drugs by undertaking an ERA as part of the regulatory approval process.
Environmental Risk Assessment of Pharmaceuticals
In both Europe and North America, there are regulatory requirements governing the ERA of human pharmaceuticals [28, 29]. It is widely accepted that the European Union (EU) regulations are currently the most demanding and data intensive. In most cases, a new regulatory submission or line extension has to be accompanied by an ERA, which requires environmental fate and effects tests to be undertaken.
ERA is addressed through the generation of a risk quotient, i.e. the ratio of the predicted environmental concentration (PEC) to the predicted no-effect concentration (PNEC) ratio (PEC:PNEC). The PEC provides an estimate of the maximum concentration anticipated to occur in the environment, resulting from patient use and subsequent excretion into the wastewater system. The PNEC is derived from ecotoxicological tests, normally on algae, daphnids and fish (representing three trophic levels), together with an assessment factor that accounts for interspecies differences in toxicity. Typically, worst-case assumptions are initially made in deriving the PEC (e.g., 100 % excretion by patients, no removal during sewage treatment), and generally if the PEC:PNEC is <1 no further information is required. Conversely, if PEC:PNEC is >1 then additional testing is generally needed to refine the PEC or PNEC. If this fails to refine the risk quotient to <1 then appropriate risk management measures may need to be put in place.
The ERA must normally be in place prior to approval of a new drug in the EU, and if an environmental risk is identified, “specific arrangements to limit it should be envisaged” [29]. However, there is no requirement for an ERA to be updated or reviewed once a new drug has been approved.
Definition of EPV
The term ‘ecopharmacovigilance’ was first coined by Velo [30]. However, a number of other articles have proposed terms to describe this newly emerging field: ecopharmacology [31], environmental pharmacology [32], pharmacoenvironmentology [33], pharmacovigilance [21, 34] and ecopharmacostewardship [35]. Whilst these articles introduce the concept of EPV, and some approaches to EPV, they tend to cover a much broader scope that captures all areas of sustainable pharmacy, such as green drug design, green chemistry in process development, minimization of manufacturing emissions, improved prescribing practices and the management of unused drugs. In addition, many of the EPV approaches that have been advocated to date have been largely preventative in nature and have assumed that the presence of pharmaceuticals in the environment will inevitably result in an adverse impact without any consideration of likelihood of impact or risk. As such many of the approaches advocated under EPV are simply designed to reduce the environmental concentrations of pharmaceuticals. In taking this preventative approach, EPV could be in danger of failing to relate field-based observations to the environmental risk assessments, or to understanding whether pharmaceuticals actually result in adverse environmental impacts, and, if so, how. It also fails to consider the relative impact that pharmaceuticals have on ecosystems versus other environmental stimuli.
PV has been defined by the World Health Organisation (WHO) as “the science and activities relating to the detection, assessment understanding and prevention of adverse effects or any other possible drug related problems” [36, 37]. Thus, a reasonable starting point for EPV is to take this definition and directly apply it to the environment. In doing so, EPV would describe the science and activities associated with the detection, evaluation, understanding and prevention of adverse effects of pharmaceuticals in the environment. This definition of EPV reflects the approach communicated at the International Society of Pharmacovigilance annual meeting in Ghana in November 2010 [38], and that endorsed by Velo and Moretti [39].
Comparison of Pharmacovigilance (PV) with EPV
Both PV and EPV aim to monitor the adverse effects of pharmaceuticals, PV in patients and EPV in the environment but potentially also in humans through indirect non-therapeutic exposure. Exposure to drugs in humans is well defined through clinical trials by knowing the dose given and measuring plasma levels, which can in turn in some instances be correlated to adverse drug reactions (ADRs). Conversely, whilst drugs and their metabolites can be detected in the environment and their concentrations measured or predicted, apart from a limited number of studies [40, 41], actual exposure in wildlife is generally not known. Drugs prescribed to patients are monitored, and ADRs identified, discussed and clarified as necessary through the PV process. In contrast, species in the environment are not routinely monitored (unless there is a specific reason to do so) and there is no equivalent to the doctor-patient interaction that is so important for identifying ADRs in patients.
PV is highly regulated in most countries around the world [29, 37] with pharmaceutical companies subject to inspection and dissuasive disciplinary measures in cases of non-compliance. In contrast, EPV is a new concept and an emerging science that is not regulated.
Last, but by no means least, determining a causal relationship between a drug, or a combination of drugs, and a possible ADR in an individual patient or a population group is not always straightforward but it is nowhere near as difficult as attributing adverse environmental impacts on environmental species to a single cause such as an individual drug, combination of drugs or a drug metabolite. This is compounded further by the presence of other synthetic and natural chemicals in the environment, and/or other environmental factors that may or may not contribute towards an observed adverse environmental impact. Some of the similarities and differences between EPV and PV are highlighted in Table 1.
Table 1.
Summary of some of the similarities and differences between ecopharmacovigilance (EPV) and pharmacovigilance (PV)
| Similarities between EPV and PV | Differences between EPV and PV | ||
|---|---|---|---|
| EPV | PV | EPV | PV |
| Aims to identify any adverse environmental impacts including the indirect impact on humans | Identifies the nature and frequency of ADRs in patients | Not subject to regulation | Highly regulated |
| Adverse environmental impact may be missed as ERA is conducted in highly controlled exposures in the laboratory, to a limited range of species that act as surrogates for all wildlife | ADRs in the wider patient populations may be missed as preclinical safety assessment is conducted within a limited range of species with defined endpoints and clinical trials represent selected patient populations under controlled conditions | Potentially all species in all environmental compartments could be exposed. This includes indirect exposure to humans | Exposure of prescribed drugs is restricted to identifiable individuals and a target population (human or veterinary) |
| EPV is captured in the ERMPs | PV is captured in the RMPs | Dose is unknown but environmental concentrations can be predicted or measured. Actual exposure levels are unknown without sophisticated biological monitoring work | Dose is known and defined by medication regimen. Exposure levels can be measured. |
| EPV issues identified for any drug are documented within the ERMP and action plans are agreed within AstraZeneca | RMPs ensure a robust assessment of the potential risks with a response plan to minimize or mitigate them for patients using AstraZeneca products | No routine monitoring is in place; however, some fish plasma levels are being monitored for scientific studies | Exposed populations are under regular supervision and routine monitoring could be in place |
| ERA procedures can learn from EPV and be refined to increase future levels of environmental protection. | PV updates the drug development programme and safety assessments | Not possible to identify adverse environmental impacts directly through discussion with the species of concern. Human intervention is required to assess impacts on the environment | In most cases it is possible to discuss and clarify issues with the patient directly. |
| If adverse environmental impacts are seen it is difficult to attribute these to one particular cause. | May or may not be easy to attribute ADR to one particular drug or a sub-population of patients | ||
ADR adverse drug reaction, ERA Environmental Risk Assessment, ERMPs AstraZeneca Environmental Risk Management Plans, RMPs AstraZeneca Risk Management Plans
Determining a Relationship between Cause and Effect in the Environment
Unlike many other chemicals that enter the environment, human drugs are designed to have highly specific interactions with their intended biochemical target in their intended target species [42]. It is these unique properties that raised questions over the potential impact of pharmaceuticals in the environment, in terms of their potential interaction with aquatic life, higher predators and humans [43]. Despite the widespread detection of pharmaceuticals in the environment and the potential for effects in wildlife species, there is only one identified case in which an adverse environmental impact in the field has been solely attributed to a pharmaceutical. Diclofenac, a non-steroidal anti-inflammatory drug, is the only well documented example where a pharmaceutical has resulted in an adverse population-level impact on non-target populations in the wild [44]. This was through its veterinary application in South-East Asia to treat inflammation and fever in domestic livestock. Vultures ingested diclofenac when feeding on the carcasses of livestock that had been treated with high doses shortly before their deaths. It is estimated that somewhere between 10 and 40 million vultures have been poisoned, and that three species of Gyps vultures are now critically endangered [45]. Gyps vultures are extremely sensitive to diclofenac and exposure to the drug causes abdominal gout and acute kidney failure. The lethal dose for renal failure is of the order of 0.1–0.2 mg/kg [46, 47]. Acute effects have also been observed in the African white-backed vulture (Gyps africanus) and the Eurasian griffon vulture (Gyps fulvus) [48] as a result of diclofenac exposure. However, the North American species of vulture such as Cathartes aura appear to be less sensitive than Gyps vultures by exposure to diclofenac [49]. Rapid population declines have also been observed in non-Gyps vulture populations in South America and Asia [50], but the cause of these declines has not yet been established. A key factor that facilitated the link between the population decline in vultures with diclofenac exposure was the scale of the population decline and the acute impact the diclofenac had. However, it is extremely unlikely that any other human pharmaceuticals will cause such obvious acute effects on wildlife and, consequently, it may prove extremely challenging to link chronic adverse impacts on wildlife with a specific pharmaceutical or group of pharmaceuticals with the same mechanism of action [45].
A classic example is the case of ethinylestradiol (EE2), a known potent endocrinally active pharmaceutical that has been shown to affect the sexual development of male fish in extremely low concentrations in the laboratory [51–53]. Comprehensive field surveys have also shown that intersex fish are widespread in British rivers [54, 55]. From an environmental risk assessment perspective, EE2 is without doubt the most extensively studied human pharmaceutical on the market. Nevertheless, it is very difficult to attribute the appearance of feminized male fish in the environment to the presence of EE2 alone since the observed effects can result from the exposure of fish to many other stressors in the environment that are also known to have endocrine-disrupting effects. These include other estrogen-like and anti-androgen-like chemicals such as the nonylphenol and octylphenol ethoxylate surfactants and their degradation products [56], bisphenol A [57], phthalates [56, 58], phytoestrogens such as genistein and equol [59] and endogenous estrogen excreted from women [60, 61]. Population level impacts have been reported in the experimental lake studies by Kidd et al. [62] as a result of EE2 exposure albeit at levels significantly above those found in rivers. This illustrates the complexity associated with linking cause and effect where several natural and synthetic chemicals are implicated, and the body of scientific data is continuing to grow and the full picture may not yet be clear.
EPV in Practice
It is clear that there are several differences between PV and EPV and several challenges that need to be overcome if EPV is to be effective in practice, particularly with respect to relating cause and effect. Nevertheless, whilst EPV is very much a developing concept, we have identified some things that can be done to ensure that risk assessments and scientific understanding of pharmaceuticals in the environment remain as up to date as possible.
Environmental Risk Management Plans (ERMPs)
In AstraZeneca we have developed the concept of ERMPs to provide a framework for capturing any environmental risks for AstraZeneca products from early development to launch and subsequently throughout the product life post-launch (Fig. 1). ERMPs include information such as physico-chemistry, pharmacokinetics, human metabolism, preclinical toxicology and environmental data (when available) of the Active Pharmaceutical Ingredient (API). The ERMP enables all available environmental data to be taken into account at key decision points during drug development, and provides early warning of drugs that could pose a potential risk to the environment. In addition, it provides a framework for monitoring environmental risks after a new product is launched, taking into account any new information that may be available. This is analogous to the Risk Management Plan (RMP), which includes a number of measures to be taken for characterizing the safety profile, mitigating and minimizing the risk to the patient of a particular pharmaceutical. Any identified risks can then be managed, with appropriate engagement of regulatory authorities and interested stakeholders. If risks are identified, appropriate follow-up measures might include additional laboratory studies or ultimately monitoring for ecological effects in the environment. However, there are very few precedents to date showing which risk management measures could be considered beyond risk refinement. On the one hand this is reassuring in that very few significant risks have been identified, but it does leave open the question of how risk mitigation would be managed in practice. The only known example of a mitigation measure beyond risk refinement is for an EE2 patch for which special package inserts were required with instructions for proper disposal [63].
Fig. 1.
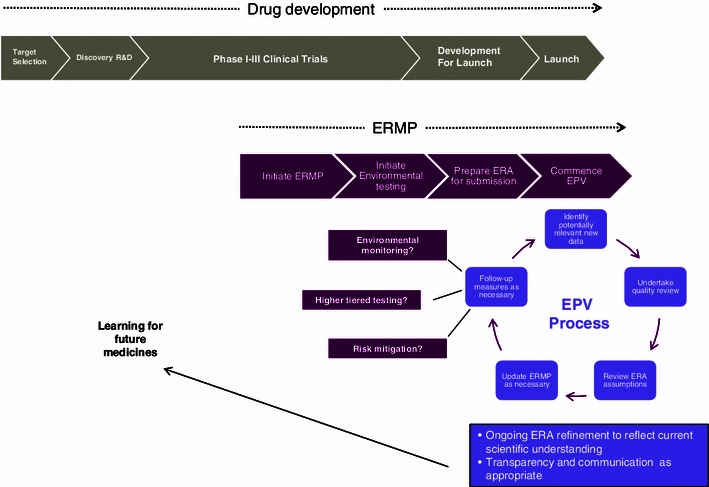
AstraZeneca’s Environmental Risk Management Plan (ERMP) concept: the ERMP is initiated during drug development to provide an early indication of any potential risks and to design an appropriate environmental testing programme for the Active Pharmaceutical Ingredient (API) in support of the Environmental Risk Assessment (ERA). After launch, the ERMP is updated as necessary if any new or emerging risks are identified as part of AstraZeneca’s internal Ecopharmacovigilance (EPV) process
Ongoing Research to Improve Scientific Understanding of Pharmaceuticals in the Environment and Environmental Risk Assessment
ERAs are by definition predictive assessments of potential risks, normally based on experimental laboratory studies. As scientific understanding increases, ERA practice and associated regulatory guidance can be developed accordingly. In many ways, the development of the current EU ERA guideline [29] demonstrated some of the principles of EPV in that it applied the scientific knowledge and understanding available at the time. Consequently, the current ERA guideline reflects that patient use and excretion result in a widespread continuous emission of low levels of pharmaceuticals to the environment, and as such longer term chronic studies with sublethal endpoints were required to indicate the potential for population level effects. It was also recognized that specific classes of drugs, or particular modes of action (e.g. compounds that are designed to interact with endocrine systems), may require additional evaluation.
One area of current interest is whether it may be possible to predict potential effects on environmental species from knowledge of the preclinical and clinical data for a compound, since many of the biological receptors and metabolic pathways present in humans are also present in environmental species [43]. Winter et al. [64] have reviewed some of the concepts and challenges faced in using preclinical data, and knowledge of mode of action, from drug discovery and development to aid in the design of more ‘intelligent’ ERA. Such knowledge can help identify potentially sensitive species or sensitive life-stages that should be considered when designing appropriate testing strategies [43]. Similarly, the physicochemical properties, metabolism, stability and adsorption data for a compound can help to identify relevant environmental compartments where it may be expected to be present, which in turn can help to focus further testing. There would seem little point in conducting tests on species that are unlikely to be exposed, for example.
There are many examples of individual and collaborative research between industry, academia and government acting in a proactive manner to improve the scientific understanding of PIE and ERA, to ensure that ERA guidance is offering adequate levels of environmental protection. The European Commission (EC) has funded a number of specific projects in the area. These include KNAPPE (Knowledge and Need Assessment on Pharmaceutical Products in Environmental Waters) [65], ERAPharm [66], Pharmas [67] and Cytothreat [68]. These projects have assessed and are currently assessing the environmental risks associated with β-blockers, selective serotonin reuptake inhibitors, antibiotics and cytotoxic drugs. In addition, the EC [69] (DG SANCO, DG Environment and the Executive Agency for Health and Consumers; EAHC) is currently reviewing data on PIE and the potential impact on the environment and public health, including a review of the current legislation for human and veterinary drugs. Similarly there have been some important national initiatives around the world that have helped to inform the PIE debate, for example the recent work undertaken by the United Kingdom Water Industry Research (UKWIR) [70], which investigated in detail the occurrence and removal of several micropollutants, including some pharmaceuticals, in UK wastewaters. Another example is the academia-based PIE project MistraPharma [71], which aims to identify human pharmaceuticals that are likely to be of concern to aquatic ecosystems, and to address the risk for promotion of antibiotic resistance in the environment.
In addition, partial and full fish life-cycle studies have been conducted to address concerns that the acute to chronic ratios used in risk assessment were not protective enough for all modes of actions. These include studies on EE2 [51], tamoxifen [72], propranolol [73], atenolol [74, 75], anastrozole and bicalutamide [76], and levonorgestrel and drospirenone [77].
Studies have also been conducted that demonstrate that the antiviral drug oseltamivir (Tamiflu®) is unlikely to have an impact on the environment as a result of widespread consumption due to the global bird flu pandemic [78], and seasonal influenza and pandemic-use conditions [79].
Antibiotics represent a class of drugs that are receiving particular attention as the increasing prevalence of antimicrobial resistance (AMR) in clinically important pathogens is undermining their efficacy. WHO has identified options for action to combat the evolving threat of antimicrobial resistance [80]. Many of the control measures identified are focused on reducing the use of antibiotics and increasing surveillance to track antimicrobial use and resistance; they do not appear to look at natural reservoirs of resistance and the impact that other chemical co-selectors may have on the increased burden and transmission of AMR. At a recent AMR workshop hosted by the Canadian Society of Microbiology it was agreed that an increasing body of data exists that demonstrates that the genes encoding for resistance in clinically relevant bacteria appear to be recruited from environmental bacteria [81–83]. Therefore more research is required to determine whether environmental input of human and veterinary antibiotics, antibiotic-resistant bacteria, biocides and metals (e.g. copper and zinc) from various activities promotes an increase in the abundance of antibiotic-resistant bacteria in clinically important pathogens.
Finally, the Society of Environmental Toxicology and Chemistry (SETAC) has recently published the outcomes of a collaborative workshop that identified the top 20 questions related to PIE [84]. The workshop was attended by experts from academia, governments and industry from around the world and provides an important summary of current knowledge gaps and future research needs. Some of the key recommendations for further research work were to (i) conduct a comparative assessment between pharmaceuticals and other environmental stressors to determine their relative impact on human and environmental health, (ii) determine whether environmental exposure to antibiotic residues results in adverse human health outcomes through the spread of antimicrobial resistance to clinically important pathogens, and (iii) link mode of action-based biomarker responses to ecologically important adverse outcome pathways.
These examples highlight just some of the proactive and collaborative approaches to product stewardship and research on PIE. They also demonstrate that all interested stakeholders from regulatory agencies, academia, non-governmental organizations and industry are actively engaged in the debate. Such initiatives demonstrate many of the principles of EPV and are essential for improving our understanding of the science of PIE. The outcomes ultimately may lead to improvements in ERA practices and can help to inform the revisions of future ERA regulation.
Literature Monitoring and ERA/ERMP Refinement
Within AstraZeneca, alongside our research activities we routinely monitor the literature for any newly published information relating to our products. Depending on the significance of any findings, such data may then be used to refine the ERA assumptions, and update the ERMPs as appropriate. In practice this generally requires identifying and assessing any relevant published ecotoxicological information that could impact the PNEC and any information on fate and exposure that might impact on the PEC. This includes any data on the occurrence of the APIs in the environment and deciding how such findings should be interpreted, for example whether measured concentrations relate to manufacturing or hospital discharges or whether they are indicative of more widespread concentrations associated with normal patient use and excretion into domestic wastewater. To be used in ERA directly, any published information, including non-standard data, needs to be sufficiently robust, for example following the criteria laid out by Klimisch et al. [85], Kϋster et al. [86] and Ågerstrand et al. [87]. If relevant information is identified, and if there is an established link between the endpoint and an adverse population effect [88], this can then be used to refine the ERA assumptions as appropriate, and options for further risk refinement, risk management or further research can then be considered in the ERMP. It is also important to recognise that publications of biomarker endpoints can also be useful to direct future research activities [89], but it is equally important that such studies include sufficient supporting information so that the data may be interpreted appropriately.
Refining ERAs when the Ratio of the Predicted Environmental Concentration to the Predicted No-Effect Concentration is >1
If the PEC:PNEC is >1, further refinement of the risk assessment is generally appropriate. This might require additional targeted testing to refine the PEC or the PNEC. Another option might be to undertake targeted monitoring of concentrations in the environment in order to confirm whether the PEC calculations are reasonable. The choice of follow-up measure adopted is likely to be decided on a case-by-case basis, reflecting the nature of the risks identified and the data available for the specific compound in question.
Propranolol is a good example of an API for which a significant amount of follow-up work was triggered based on initial ERA findings. The original work from Huggett et al. [90, 91] suggested that the concentrations in the environment may lead to harmful effects in fish. This then led to several research projects, including the major EC-funded project ERAPharm, which focused not only on propranolol, but on other β-blockers, such as atenolol, in order to improve understanding of the risks associated with this group of compounds. The work of ERAPharm and other research have helped to provide new data to refine the original risk assessment [75]. These focused studies showed that propranolol biodegraded in the environment (indeed it was readily mineralized in some tests). It is also readily photodegraded [92, 93], and unlikely to bioaccumulate [94, 95]. There is also now much more ecotoxicity data available, including chronic fish studies [95], such that the weight of evidence suggests that propranolol is not as toxic to fish as previously thought. Perhaps most importantly, it is also now clear that not all β-blockers have the same ecotoxicity profile, since the lowest ‘No Observed Effect Concentration’ (NOEC) for atenolol [75], for example, is over two orders of magnitude higher (less toxic) than the lowest NOEC for propranolol [26]. Overall these data provide reassuring answers to the questions that the original assessments posed. Figure 2 shows that, from all the available surface water-monitoring data of propranolol in the environment, in most cases the measured data are lower than the PNEC, with the exception of about 10 % of cases. These data represent a broad range of sampling regimens (e.g., spot and composite samples) and different types of measurements (e.g., peak vs. mean concentrations), so care is needed when interpreting the results. However, on face value the data provide an indication of where the potential risk may be highest and where further investigation might be needed. There are many potential reasons why the risks may be higher in some areas, for example if there is inadequate wastewater treatment, and/or particularly high population density or low dilution capacity in the receiving environment. Whatever the reason, such an analysis, when cross-referenced to specific locations, enables researchers to target further investigations in those local geographical areas where the potential for risk is higher, thereby making best use of available resources.
Fig. 2.
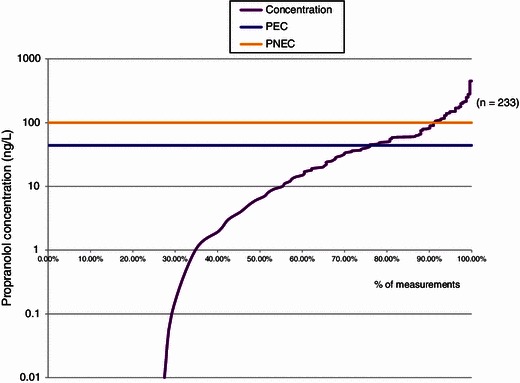
Published Measured Environmental Concentrations of propranolol in surface waters. PEC predicted environmental concentration, PNEC predicted no-effect concentration
For drugs that are relatively data rich, species sensitivity distributions have been generated with all the environmental effects data to provide more confidence in the effects and risk assessment. Two examples of such an approach are the work of Caldwell et al. [96] for EE2, and the deterministic and probabilistic risk assessment of naproxen by Straub and Stewart [97]. Further refinement in the PEC values for EE2 have been made based on the results from the PhATE (Pharmaceutical Assessment and Transport Evaluation) and GREAT-ER (Geography Referenced Regional Exposure Assessment Tool for European Rivers) models to identify the 90th-percentile low-flow PECs in surface water for EE2 in the USA and Europe, respectively [98].
Keeping a Global EPV Perspective
Current ERA practices largely reflect EU and US pharmaceutical use patterns and the potential risks associated with drugs in those regions. Just as PV addresses regional differences, so too should ERAs be designed to ensure protection in any region where the drug will be used. Whilst many areas of the European Medicines Agency (EMA) ERA guideline have global relevance, there may be some inherent assumptions that are not applicable in other regions. For example, the EMA guideline does not consider irrigation as a potential route to the terrestrial environment, whilst this is normal practice in some parts of the world, particularly in water-stressed areas. Similarly, disease prevalence, cultural practices and climate are different in different parts of the world, so the risk profile associated with a pharmaceutical agent may also be different. The challenge is to identify what region-specific exposure scenarios may need to be considered, recognizing that this may not always be straightforward, especially when considering uses such as for example the veterinary use of diclofenac in cattle. A major reason for the unanticipated impact of diclofenac on vulture populations was the sensitivity of certain raptors to diclofenac and a failure of the risk assessment to recognise this exposure route. Secondary poisoning of raptors has previously been recognised and mitigated against. For example, bald and golden eagles, other wildlife and domestic dogs have been intoxicated or killed after ingestion of pentobarbital residues present in tissues of euthanized carcasses that have been disposed of inadequately [99]. In order to control these risks, disposal procedures were tightened (e.g., incineration of euthanized carcasses or immediate deep burial) and penalties for the violation of appropriate disposal were developed. Thus, it is certainly relevant, and arguably the essence of EPV, to ask the question whether the vulture decline could have been detected earlier if this exposure route had been identified before employing widespread use in cattle. As pointed out by Winter et al. [64], if this exposure route had been considered, then this might have triggered targeted effects testing on carrion-feeding birds. This underlines the importance of consideration of the patterns of compound usage, local cultural and agricultural practices, and ecology of the species assessed, in order to explain the patterns of contamination observed.
Transparency with Data
One of the ways to encourage effective EPV practices is to ensure that relevant environmental information is shared between government, academia, industry and other interested stakeholders. For several years environmental data have been made publically available in the Swedish Prescribing guide [100], which includes environmental risk information of the API, based on the PEC/PNEC ratio, as well as information about degradation and bioaccumulation, and results from environmental studies. Environmental data for AstraZeneca products are now also available on their corporate responsibility webpages [101]. The information available on AstraZeneca.com is slightly different to that on Fass.se in that it considers an EU-wide risk assessment, rather than a Swedish-based one; however, both systems are based on the total API volume used in all products, from all companies, containing the same active ingredient. It is hoped that this transparency will contribute to the scientific knowledge about environmental properties of API. It is notable that the EMA has recently made significant changes to its policy on data transparency [102]. It is not yet clear how this will work in practice but it is likely that much of the ERA information that is provided as part of the regulatory submission will be more publically accessible in future.
Identifying Adverse Environmental Impacts
One of the key challenges for EPV is that any observations of ecological trends or adverse effect in the environment will almost certainly not (at least initially) be identified as being associated with any one particular cause. It took several years to identify the cause of the vulture decline due to diclofenac poisoning. Similarly, research into the causes and consequences of intersex in fish is now well into its second decade, with no single cause having been identified. Whether there is a long-term population-level impact is also still uncertain and is dependent on the severity of feminized males [103, 104]. Another key challenge for EPV is that in the environment there are many different species that may be potentially exposed; however, it is simply not possible to monitor all of them. In contrast, with PV, it is usually possible to monitor all patients who are taking a particular drug.
Biological monitoring studies of species, species assemblages and ecosystems are being undertaken all the time by a range of researchers in many parts of the world. These may identify adverse or unexpected effects of unknown cause and such observations may (or may not) subsequently be included in reports or scientific publications. However, even if the observations are reported they are, in effect, randomly distributed throughout the literature and there is currently no worldwide process, other than serendipity, whereby connections might be made and restorative action initiated.
In the EU, this type of monitoring activity already forms the central core of the Water Framework Directive (WFD), and requires that every watercourse within the EU27 has to be monitored periodically to determine its ecological status. Those that do not comply with the conditions for “good ecological” status must be subjected to further investigation to determine the reason for their non-compliance. Once the reasons have been established, plans then need to be drawn up and implemented to remedy the deficiency.
In terms of pharmaceuticals, it would be expected that any adverse impact in the aquatic environment would occur where the environmental residue concentration was highest, for example in the vicinity of outfalls from large wastewater treatment plants. Consequently, within the EU any such adverse impacts could emerge from the ecological monitoring being undertaken for the WFD, although attribution of cause and effect is still likely to be extremely difficult unless there is a very substance-specific effect. In addition, potential adverse environmental impacts in species living in the terrestrial or atmospheric environment would be unlikely to be identified from the activities within the WFD. It should also be noted that ecological monitoring is undertaken at a local level with no formal mechanism for sharing data on adverse impacts either between or even within member states.
Discussion
The above sections highlight some of the challenges associated with EPV and some of the practical measures that can be undertaken to ensure that the ERA understanding of a drug remains up to date and globally relevant throughout the life of a new drug.
Most of the pro-active measures proposed here often form part of the research activities that are already undertaken by pharmaceutical companies, academics and governments, sometimes collaboratively, and are not part of any regulatory requirement. However, it is also clear in the EU Medicines Directive that if a risk is identified in the ERA follow-up work is required to refine the ERA or identify appropriate “specific arrangements to limit it”. Thus, in principle the mechanism exists in the EU to manage risks effectively for new medicinal products and line extensions, providing those risks are identified before approval.
One additional challenge for EPV is that many older established drugs pre-date current regulatory requirements for environmental risk assessment. Of approximately 4,000 APIs on the market today only about 10 % have sufficient data to enable a PEC:PNEC value to be calculated [84]. For these drugs there is typically considerably more information on their occurrence in the environment than there is on their effects. Thus, the significance of trace levels of these drugs in the environment is often poorly understood. The challenge is to identify which of these APIs should be prioritized for further evaluation.
In an attempt to address this challenge, Roos et al. [105] have used nine prioritization schemes to prioritize and rank 582 human drugs based on environmental hazard and risk. Due to the availability of data, not all these drugs could be assessed. The authors favoured risk-based approaches over hazard-based systems, as environmental risk reflects both exposure and impact, and recommended that hazard-based approaches should only be applied for human drugs where insufficient exposure data exist. Using the traditional PEC:PNEC prioritization approach on 196 human drugs, for which robust data were available, they identified seven with a PEC:PNEC >1, indicating that, where sufficient data exist for analysis, the majority of pharmaceuticals pose no significant risk to the environment.
Summary and Conclusions
In this article we have accepted the definition of EPV based upon the WHO definition of PV:
Ecopharmacovigilance is the science and activities associated with the detection, evaluation, understanding and prevention of adverse effects of pharmaceuticals in the environment.
We have presented some ideas on what EPV might mean in practice, together with some challenges and opportunities for implementing EPV procedures. We suggest that the main focus of EPV should be after launch of a drug, which will help to identify any possible risks throughout the life of the product. It should be emphasized that EPV is a developing science, still very much in its infancy, and there is therefore room for further debate and research before any formalized approach to EPV is established.
We have identified that there are many similarities between EPV and PV, but also some important differences that have implications for any practical implementation of EPV. In particular, to determine a causal relationship between a drug and an ADR is not straightforward in terms of a patient, but nowhere near as difficult as attributing adverse impacts in environmental species to a single drug.
However, we have identified some approaches that can be taken, including;
Tracking environmental risks after launch of the product, via literature monitoring for emerging data, and by use of Environmental Risk Management Plans
Further research, testing or monitoring in the environment when a risk is identified
Keeping a global EPV perspective
Increasing transparency and availability of environmental data for medicinal products.
These measures will help to ensure that any issues associated with PIE are identified in a timely way, and can be managed appropriately. In addition, research in this area will continue, and the SETAC 20 questions publication [84] has provided a comprehensive summary of the current state of science of PIE and has identified clear areas where future research is needed.
Acknowledgments
Sarah Barrett, Nigel Budgen, Claire Coleman, Paul Robinson and Alan Sharpe are acknowledged for their valuable input into the establishing of ecopharmacovigilance principles in AstraZeneca. In addition support from the AstraZeneca Safety, Health and Environment Strategy is acknowledged.
Conflict of interest
The authors have no conflicts of interest that are directly relevant to the content of this paper.
References
- 1.European Commission. Regulation (EU) No 1235/2010 of the European parliament and of the Council. Volume 1. Pharmaceutical legislation medicinal products for human use. 2010. Available from URL: http://ec.europa.eu/health/documents/eudralex/vol-1/. Accessed 4 Apr 2013.
- 2.Alder AC. Consumption and occurrence. In: Ternes TA, Joss A, editors. Human pharmaceuticals, hormones and fragrances: the challenge of micropollutants in urban water management. London: IWA Publishing; 2006. [Google Scholar]
- 3.Daughton CG, Ternes TA. Pharmaceuticals and personal care products in the environment: agents of subtle change? Environ Health Perspect. 1999;107(Suppl.6):907–38. [DOI] [PMC free article] [PubMed]
- 4.Kϋmmerer K. Drugs in the environment: emission of drugs, diagnostic aids and disinfectants into wastewater by hospitals in relation to other sources: a review. Chemosphere. 2001;45(6–7):957–969. doi: 10.1016/S0045-6535(01)00144-8. [DOI] [PubMed] [Google Scholar]
- 5.Vanderford BJ, Snyder SA. Analysis of pharmaceuticals in water by isotope dilution liquid chromatography/tandem mass spectrometry. Environ Sci Technol. 2006;40(23):7312–7320. doi: 10.1021/es0613198. [DOI] [PubMed] [Google Scholar]
- 6.Batt AL, Kostich MS, Lazorchak JM. Analysis of ecologically relevant pharmaceuticals in wastewater and surface water using selective solid-phase extraction and UPLC-MS/MS. Anal Chem. 2008;80(13):5021–5030. doi: 10.1021/ac800066n. [DOI] [PubMed] [Google Scholar]
- 7.Kasprzyk-Hordern B, Baker DR. Estimation of community-wide drugs use via stereoselective profiling of sewage. Sci Total Environ. 2012;423:142–150. doi: 10.1016/j.scitotenv.2012.02.019. [DOI] [PubMed] [Google Scholar]
- 8.Kϋmmerer K. The presence of pharmaceuticals in the environment due to human use—present knowledge and future challenges. J Environ Manage. 2009;90(8):2354–2366. doi: 10.1016/j.jenvman.2009.01.023. [DOI] [PubMed] [Google Scholar]
- 9.Cunningham VL, Binks SP, Olson MJ. Human health risk assessment from the presence of human pharmaceuticals in the aquatic environment. Regul Toxicol Pharmacol. 2009;53(1):39–45. doi: 10.1016/j.yrtph.2008.10.006. [DOI] [PubMed] [Google Scholar]
- 10.Heberer T. Occurrence, fate, and removal of pharmaceutical residues in the aquatic environment: a review of recent research data. Toxicol Lett. 2002;131(1–2):5–17. doi: 10.1016/S0378-4274(02)00041-3. [DOI] [PubMed] [Google Scholar]
- 11.Fent K, Weston AA, Caminada D. Ecotoxicology of human pharmaceuticals. Aquat Toxicol. 2006;76(2):122–159. doi: 10.1016/j.aquatox.2005.09.009. [DOI] [PubMed] [Google Scholar]
- 12.Kim SD, Cho J, Kim IS, Vanderford BJ, Snyder SA. Occurrence and removal of pharmaceuticals and endocrine disruptors in South Korean surface, drinking, and waste waters. Water Res. 2007;41(5):1013–21. [DOI] [PubMed]
- 13.Daughton CG, Ruhoy IS. Environmental footprint of pharmaceuticals: the significance of factors beyond direct excretion to sewers. Environ Toxicol Chem. 2009;28(12):2495–2521. doi: 10.1897/08-382.1. [DOI] [PubMed] [Google Scholar]
- 14.Snyder SA. Pharmaceuticals, personal care products and endcrine disruptors in water: implications for the water industry. Environ Eng Sci. 2003;20:449. doi: 10.1089/109287503768335931. [DOI] [Google Scholar]
- 15.Koplin DW. Pharmaceuticals, hormones and other organic wastewater contaminants in US streams, 199–2000: a national reconnaissance. Environ Science Technol. 2002;36:1202–1211. doi: 10.1021/es011055j. [DOI] [PubMed] [Google Scholar]
- 16.Kϋmmerer K. Pharmaceuticals in the environment: a brief summary. In: Kϋmmerer K, editor. Pharmaceuticals in the environment. London: Springer; 2008. pp. 3–21. [Google Scholar]
- 17.Monteiro SC, Boxall AB. Occurrence and fate of human pharmaceuticals in the environment. Rev Environ Contam Toxicol. 2010;202:53–154. doi: 10.1007/978-1-4419-1157-5_2. [DOI] [PubMed] [Google Scholar]
- 18.Bound JP, Voulvoulis N. Predicted and measured concentrations for selected pharmaceuticals in UK rivers: implications for risk assessment. Water Res. 2006;40(15):2885–92. [DOI] [PubMed]
- 19.Barnes KK, Christenson SC, Kolpin DW, Focazio MJ, Furlong ET, Zaugg SD, et al. Pharmaceuticals and other organic waste water contaminants within a leachate plume downgradient of a municipal landfill. Ground Water Monit Remediat. 2004;24(2):119–126. doi: 10.1111/j.1745-6592.2004.tb00720.x. [DOI] [Google Scholar]
- 20.Halling-Sørensen B, Nors Nielsen S, Lanzky PF, Ingerslev F, Holten Lutzhoft HC, Jorgensen SE. Occurrence, fate and effects of pharmaceutical substances in the environment: a review. Chemosphere. 1998;36(2):357–93. [DOI] [PubMed]
- 21.Daughton CG, Ruhoy IS. Green pharmacy and pharmEcovigilance: prescribing and the planet. Expert Rev Clin Pharmacol. 2011;4(2):211–232. doi: 10.1586/ecp.11.6. [DOI] [PubMed] [Google Scholar]
- 22.Thomas KV, Dye C, Schlabach M, Langford KH. Source to sink tracking of selected human pharmaceuticals from two Oslo city hospitals and a wastewater treatment works. J Environ Monit. 2007;9(12):1410–8. [DOI] [PubMed]
- 23.Zhang Y, Yang M, Liu M, Dong L, Renli R. Antibiotic pollution from Chinese drug manufacturing: antibiotic resistance. Toxicol Lett. 2012;211(Suppl.:S16).
- 24.Larsson DGJ, de Pedro C, Paxeus N. Effluent from drug manufactures contains extremely high levels of pharmaceuticals. J Hazard Mater. 2007;148(3):751–5. [DOI] [PubMed]
- 25.Li D, Yang M, Hu J, Ren L, Zhang Y, Li K. Determination and fate of oxytetracycline and related compounds in oxytetracycline production wastewater and the receiving river. Environ Toxicol Chem. 2008;27(1):80–86. doi: 10.1897/07-080.1. [DOI] [PubMed] [Google Scholar]
- 26.Murray-Smith RJ, Coombe VT, Grönlund MH, Waern F, Baird JA. Managing emissions of active pharmaceutical ingredients from manufacturing facilities: an environmental quality standard approach. Integr Environ Assess Manage. 2012;8(2):320–330. doi: 10.1002/ieam.1268. [DOI] [PubMed] [Google Scholar]
- 27.Snape JR, Lewis C, Murray-Smith R. Pollution: drug firm monitors waste water. Nature. 2011;477:33. [DOI] [PubMed]
- 28.US FDA. Guidance for industry: environmental assessment of human drug and biologics application. Silver Spring; US FDA, 1998.
- 29.Commission European. Directive 2001/83/EC of the European Parliament and of the Council of 6 November 2001 on the Community code relating to medicinal products for human use. Off J Eur Commun. 2004;311:67. [Google Scholar]
- 30.Velo GP. Why ecopharmacovigilance. Drug Saf. 2007;30(10):919. [Google Scholar]
- 31.Kϋmmerer K, Velo G. Ecopharmacology: a new topic of importance in pharmacovigilance. Drug Saf. 2006;29(5):371–373. doi: 10.2165/00002018-200629050-00001. [DOI] [PubMed] [Google Scholar]
- 32.Rahman SZ, Khan RA. Environmental pharmacology: a new discipline. Indian J Pharmacol. 2006;38:229–230. doi: 10.4103/0253-7613.27017. [DOI] [Google Scholar]
- 33.Rahman SZ, Khan RA, Gupta V, Uddin M. Pharmacoenvironmentology: a component of pharmacovigilance. Environ Health. 2007;6:20. [DOI] [PMC free article] [PubMed]
- 34.Daughton CG, Ruhoy IS. The afterlife of drugs and the role of pharmEcovigilance. Drug Saf. 2008;31(12):1069–1082. doi: 10.2165/0002018-200831120-00004. [DOI] [PubMed] [Google Scholar]
- 35.Taylor D. Ecopharmacostewardship: a pharmaceutical industry perspective. In: Kϋmmerer K, Hempel M, editors. Green and sustainable pharmacy. Berlin/Heidelberg: Springer; 2010. pp. 105–126. [Google Scholar]
- 36.World Health Organisation . The importance of pharmacovigilance: safety monitoring of medicinal products. Geneva: World Health Organisation; 2002. [Google Scholar]
- 37.Wise L, Parkinson J, Raine J, Breckenridge A. New approaches to drug safety: a pharmacovigilance tool kit. Nat Rev Drug Discov. 2009;8:779–782. doi: 10.1038/nrd3002. [DOI] [PubMed] [Google Scholar]
- 38.Murray-Smith R. Ecopharmacovigilance: a drug company perspective. 10th Annual Meeting of the International Society of Pharmacovigilance, Accra, Ghana. 4 November 2010. Available from URL: http://isop2010.isoponline.org/uploads/prog/Programme_-3rd_-_7th_November-.pdf. Accessed 4 Apr 2013.
- 39.Velo G, Moretti U. Ecopharmacovigilance for better health. Drug Saf. 2010;33(11):963–968. doi: 10.2165/11539380-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 40.Cuklev F, Kristiansson E, Fick J, Asker N, Förlin L, Larsson DGJ. Diclofenac in fish: blood plasma levels similar to human therapeutic levels affect global hepatic gene expression. Environ Toxicol Chem. 2011;30(9):2126–2134. doi: 10.1002/etc.599. [DOI] [PubMed] [Google Scholar]
- 41.Fick J, Lindberg RH, Parkkonen J, Arvidsson B, Tysklind M, Larsson DGJ. Therapeutic levels of levonorgestrel detected in blood plasma of fish: results from screening rainbow trout exposed to treated sewage effluents. Environ Sci Technol. 2010;44(7):2661–2666. doi: 10.1021/es903440m. [DOI] [PubMed] [Google Scholar]
- 42.Ankley GT, Black MC, Garric J, Hutchinson TH, Iguchi T. A framework for assessing the hazard of pharmaceutical materials to aquatic species. In: William RT, editor. Human pharmaceuticals: assessing the impacts on aquatic ecosystems. Florida: SETAC Press; 2005. [Google Scholar]
- 43.Gunnarsson L, Jauhiainen A, Kristiansson E, Nerman O, Larsson DGJ. Evolutionary conservation of human drug targets in organisms used for environmental risk assessments. Environ Sci Technol. 2008;42(15):5807–5813. doi: 10.1021/es8005173. [DOI] [PubMed] [Google Scholar]
- 44.Oaks JL, Gilbert M, Virani MZ, Watson RT, Meteyer CU, Rideout BA, et al. Diclofenac residues as the cause of vulture population decline in Pakistan. Nature. 2004;427(6975):630–633. doi: 10.1038/nature02317. [DOI] [PubMed] [Google Scholar]
- 45.Sumpter J. Pharmaceuticals in the environment: moving from a problem to a solution. In: Kϋmmerer K, Hempel M, editors. Green and sustainable pharmacy. Berlin: Springer; 2010. p. 11–22.
- 46.Green RE, Newton I, Shultz S, Cunningham AA, Gilbert M, Pain DJ, et al. Diclofenac poisoning as a cause of vulture population declines across the Indian subcontinent. J Appl Ecol. 2004;41(5):793–800. doi: 10.1111/j.0021-8901.2004.00954.x. [DOI] [Google Scholar]
- 47.Green RE, Taggart MA, Senacha KR, Raghavan B, Pain DJ, Jhala Y, et al. Rate of decline of the Oriental White-backed vulture population in India estimated from a survey of diclofenac residues in carcasses of ungulates. PLoS ONE. 2007;2(8):e686. doi: 10.1371/journal.pone.0000686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Swan GE, Cuthbert R, Quevedo M, Green RE, Pain DJ, Bartels P, et al. Toxicity of diclofenac to Gyps vultures. Biol Lett. 2006;2(2):279–282. doi: 10.1098/rsbl.2005.0425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Rattner BA, Whitehead MA, Gasper G, Meteyer CU, Link WA, Taggart MA, et al. Apparent tolerance of turkey vultures (Cathartes aura) to the non-steroidal anti-inflammatory drug diclofenac. Environ Toxicol Chem. 2008;27(11):2341–2345. doi: 10.1897/08-123.1. [DOI] [PubMed] [Google Scholar]
- 50.Cuthbert R, Parry-Jones J, Green RE, Pain DJ. NSAIDs and scavenging birds: potential impacts beyond Asia’s critically endangered vultures. Biol Lett. 2007;3(1):90–93. doi: 10.1098/rsbl.2006.0554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Länge R, Hutchinson TH, Croudace CP, Siegmund F, Schweinfurth H, Hampe P, et al. Effects of the synthetic estrogen 17beta-ethinylestradiol on the life-cycle of the fathead minnow (Pimephales promelas) Environ Toxicol Chem. 2001;20(6):1216–1227. doi: 10.1897/1551-5028(2001)020<1216:eotsee>2.0.co;2. [DOI] [PubMed] [Google Scholar]
- 52.Nash JP, Kime DE, Van der Ven LT, Wester PW, Brion F, Maack G, et al. Long-term exposure to environmental concentrations of the pharmaceutical ethynylestradiol causes reproductive failure in fish. Environ Health Perspect. 2004;112(17):1725–33. [DOI] [PMC free article] [PubMed]
- 53.Caldwell DJ, Mastrocco F, Anderson PD, Länge R, Sumpter JP. Predicted-no-effect concentrations for the steroid estrogens estrone, 17beta-estradiol, estriol, and 17beta-ethinylestradiol. Environ Toxicol Chem. 2012;31(6):1396–1406. doi: 10.1002/etc.1825. [DOI] [PubMed] [Google Scholar]
- 54.Jobling S, Nolan M, Tyler CR, Brighty G, Sumpter JP. Widespread sexual disruption in wild fish. Environ Sci Technol. 1998;32(17):2498–2506. doi: 10.1021/es9710870. [DOI] [Google Scholar]
- 55.Jobling S, Tyler CR. Introduction: the ecological relevance of chemically induced endocrine disruption in wildlife. Environ Health Perspect. 2006;114(Suppl. 1):7–8. doi: 10.1289/ehp.8046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Soares A, Guieysse B, Jefferson B, Cartmell E, Lester JN. Nonylphenol in the environment: a critical review on occurrence, fate, toxicity and treatment in wastewaters. Environ Int. 2008;34(7):1033–1049. doi: 10.1016/j.envint.2008.01.004. [DOI] [PubMed] [Google Scholar]
- 57.Crain AD, Eriksen M, Iguchi T, Jobling S, Laufer H, LeBlanc GA, et al. An ecological assessment of bisphenol-A: evidence from comparative biology. Reprod Toxicol. 2007;24:225–239. doi: 10.1016/j.reprotox.2007.05.008. [DOI] [PubMed] [Google Scholar]
- 58.Carnevali O, Tosti L, Speciale C, Peng C, Zhu Y, Maradonna F. DEHP impairs zebrafish reproduction by affecting critical factors in oogenesis. PLoS ONE. 2010;5(4):e10201. doi: 10.1371/journal.pone.0010201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Kiparissis Y, Balch GC, Metcalfe TL, Metcalfe CD. Effects of the isoflavones genistein and equol on the gonadal development of Japanese medaka (Oryzias latipes) Environ Health Perspect. 2003;111(9):1158–1163. doi: 10.1289/ehp.5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Desbrow C, Routledge EJ, Brighty GC, Sumpter JP, Waldock M. Identification of estrogenic chemicals in STW effluent. 1. Chemical fractionation and in vitro biological screening. Environ Sci Technol. 1998;32(11):1549–1558. doi: 10.1021/es9707973. [DOI] [Google Scholar]
- 61.Thorpe KL, Cummings RI, Hutchinson TH, Scholze M, Brighty G, Sumpter JP, et al. Relative potencies and combination effects of steroidal estrogens in fish. Environ Sci Technol. 2003;37(6):1142–1149. doi: 10.1021/es0201348. [DOI] [PubMed] [Google Scholar]
- 62.Kidd KA, Blanchfield PJ, Mills KH, Palace VP, Evans RE, Lazorchak JM, et al. Collapse of a fish population after exposure to a synthetic estrogen. Proc Natl Acad Scis. 2007;104(21):8897–8901. doi: 10.1073/pnas.0609568104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Janssen Pharmaceutica. ERAR (European Public Assessment Report) for EVRA (Ref EMEA/H/C/410, attached). 2012. Available from URL: http://www.emea.europa.eu/docs/en_GB/document_library/EPAR_-_Product_Information/human/000410/WC500031512.pdf. Accessed Oct 2012.
- 64.Winter MJ, Owen SF, Murray-Smith R, Panter GH, Hetheridge MJ, Kinter LB. Using data from drug discovery and development to aid the aquatic environmental risk assessment of human pharmaceuticals: concepts, considerations, and challenges. Integr Environ Assess Manag. 2010;6(1):38–51. doi: 10.1897/IEAM_2009-044.1. [DOI] [PubMed] [Google Scholar]
- 65.KNAPPE. Pharmaceutical Products in Environmental Waters (KNAPPE). 2012. Available from URL: http://www.ecologic.eu/2293. Accessed Oct 2012.
- 66.Duis K, Coors A. Environmental risk assessment of pharmaceuticals (ERAPharm). 2008. Available from URL: http://www.erapharm.org/. Accessed Jan 2008.
- 67.Sumpter JP, Roig B. Ecological and human health risk assessments of antibiotics and anti-cancer drugs found in the environment. 2012. Available from URL: http://www.pharmas-eu.org/. Accessed May 2012.
- 68.Filipic M. Fate and effects of cytostatic pharmaceuticals in the environment and identification of biomarkers for an improved risk assessment on environmental exposure (CytoThreat). 2012. Available from URL: http://www.cytothreat.eu/. Accessed May 2012.
- 69.European Commission. Call for tender no. EAHC/2011/Health/12 concerning study on the risks of the environmental effects of medicinal products. 2011. Available from URL: http://ec.europa.eu/eahc/health/tenders_H12_2011.html. Accessed 4 Apr 2013.
- 70.Gardner M, Comber S, Scrimshaw MD, Cartmell E, Lester J, Ellor B. The significance of hazardous chemicals in wastewater treatment works effluents. Sci Total Environ. 2012;437(0):363–72. [DOI] [PubMed]
- 71.Rudén C. Identification and reduction of risks caused by pharmaceuticals (MISTRAPharma). 2012. Available from URL: http://www.mistrapharma.se/. Accessed May 2012.
- 72.Williams TD, Caunter JE, Lillicrap AD, Hutchinson TH, Gillings EG, Duffell S. Evaluation of the reproductive effects of tamoxifen citrate in partial and full life-cycle studies using fathead minnows (Pimephales Promelas) Environ Toxicol Chem. 2007;26(4):695–707. doi: 10.1897/05-646R1.1. [DOI] [PubMed] [Google Scholar]
- 73.Giltrow E, Eccles PD, Winter MJ, McCormack PJ, Rand-Weaver M, Hutchinson TH, et al. Chronic effects assessment and plasma concentrations of the β-blocker propranolol in fathead minnows (Pimephales promelas) Aquatic Toxicol. 2009;95(3):195–202. doi: 10.1016/j.aquatox.2009.09.002. [DOI] [PubMed] [Google Scholar]
- 74.Winter MJ, Lillicrap AD, Caunter JE, Schaffner C, Alder AC, Ramil M, et al. Defining the chronic impacts of atenolol on embryo-larval development and reproduction in the fathead minnow (Pimephales promelas) Aquatic Toxicol. 2008;86(3):361–369. doi: 10.1016/j.aquatox.2007.11.017. [DOI] [PubMed] [Google Scholar]
- 75.Küster A, Alder AC, Escher BI, Duis K, Fenner K, Garric J, et al. Environmental risk assessment of human pharmaceuticals in the European Union: a case study with the B-blocker atenolol. Integr Environ Assess Manag. 2010;6(S1):514–23. [DOI] [PubMed]
- 76.Panter GH, Glennon YC, Robinson J, Hargreaves A, Murray-Smith R. Effects of the anti-androgen, bicalutamide, in a reduced life-cycle study with the fathead minnow (Pimephales promelas) Aquatic Toxicol. 2012;114–115:31–38. doi: 10.1016/j.aquatox.2012.02.002. [DOI] [PubMed] [Google Scholar]
- 77.Zeilinger J, Steger-Hartmann T, Maser E, Goller S, Vonk R, Länge R. Effects of synthetic gestagens on fish reproduction. Environ Toxicol Chem. 2009;28(12):2663–2670. doi: 10.1897/08-485.1. [DOI] [PubMed] [Google Scholar]
- 78.Hutchinson TH, Beesley A, Frickers PE, Readman JW, Shaw JP, Straub J. Extending the environmental risk assessment for oseltamivir (Tamiflu®) under pandemic use conditions to the coastal marine compartment. Environ Int. 2009;35(6):931–936. doi: 10.1016/j.envint.2009.04.001. [DOI] [PubMed] [Google Scholar]
- 79.Straub J. An environmental risk assessment for oseltamivir (Tamiflu) for sewage works and surface waters under seasonal-influenza- and pandemic-use conditions. Ecotoxicol Environ Saf. 2009;72(6):1625–34. [DOI] [PubMed]
- 80.World Health Organization . The evolving threat of antimicrobial resistance: options for action. Geneva: World Health Organization; 2012. [Google Scholar]
- 81.Szczepanowski R, Linke B, Krahn I, Gartemann K, Gützkow T, Eichler W, et al. Detection of 140 clinically relevant antibiotic-resistance genes in the plasmid metagenome of wastewater treatment plant bacteria showing reduced susceptibility to selected antibiotics. Microbiology. 2009;155(7):2306–2319. doi: 10.1099/mic.0.028233-0. [DOI] [PubMed] [Google Scholar]
- 82.Jury K, Khan SJ, Vancov T, Stuetz RM, Ashbolt NJ. Are sewage treatment planst promoting antibiotic resistance. Crit Rev Environ Sci Technol. 2011;41:243–270. doi: 10.1080/10643380902772589. [DOI] [Google Scholar]
- 83.Börjesson S, Matussek A, Melin S, Löfgren S, Lindgren PE. Methicillin-resistant Staphylococcus aureus (MRSA) in municipal wastewater: an uncharted threat? J Appl Microbiol. 2010;108(4):1244–1251. doi: 10.1111/j.1365-2672.2009.04515.x. [DOI] [PubMed] [Google Scholar]
- 84.Boxall ABA, Rudd MA, Brooks BW, Caldwell DJ, Choi K, Hickmann S, et al. Pharmaceuticals and personal care products in the environment: what are the big questions? Environ Health Perspect. 2012;120(9):1221–1229. doi: 10.1289/ehp.1104477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Klimisch H, Andreae M, Tillmann U. A systematic approach for evaluating the quality of experimental toxicological and ecotoxicological data. Regul Toxicol Pharmacol. 1997;25(1):1–5. doi: 10.1006/rtph.1996.1076. [DOI] [PubMed] [Google Scholar]
- 86.Kϋster A, Bachmann J, Brandt U, Ebert I, Hickmann S, Klein-Goedicke J, et al. Regulatory demands on data quality for the environmental risk assessment of pharmaceuticals. Regul Toxicol Pharmacol. 2009;55(3):276–80. [DOI] [PubMed]
- 87.Ågerstrand M, Kϋster A, Bachmann J, Breitholtz M, Ebert I, Rechenberg B, et al. Reporting and evaluation criteria as means towards a transparent use of ecotoxicity data for environmental risk assessment of pharmaceuticals. Environ Pollut. 2011;159(10):2487–2492. doi: 10.1016/j.envpol.2011.06.023. [DOI] [PubMed] [Google Scholar]
- 88.Ankley GT, Bennett RS, Erickson RJ, Hoff DJ, Hornung MW, Johnson RD, et al. Adverse outcome pathways: a conceptual framework to support ecotoxicology research and risk assessment. Environ Toxicol Chem. 2010;29(3):730–741. doi: 10.1002/etc.34. [DOI] [PubMed] [Google Scholar]
- 89.Hutchinson TH, Ankley GT, Segner H, Tyler CR. Screening and testing for endocrine disruption in fish: biomarkers as “signposts”, not “traffic Lights”, in risk assessment. Environ Health Perspect. 2006;114(Suppl. 1):106–114. doi: 10.1289/ehp.8062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Huggett DB, Brooks BW, Peterson B, Foran CM, Schlenk D. Toxicity of select beta adrenergic receptor-blocking pharmaceuticals (B-Blockers) on aquatic organisms. Arch Environ Contam Toxicol. 2002;43(2):229–235. doi: 10.1007/s00244-002-1182-7. [DOI] [PubMed] [Google Scholar]
- 91.Huggett DB, Khan IA, Foran CM, Schlenk D. Determination of beta-adrenergic receptor blocking pharmaceuticals in United States wastewater effluent. Environ Pollut. 2003;121(2):199–205. doi: 10.1016/S0269-7491(02)00226-9. [DOI] [PubMed] [Google Scholar]
- 92.Liu Q, Williams HE. Kinetics and degradation products for direct photolysis of B-blockers in water. Environ Sci Technol. 2007;41(3):803–810. doi: 10.1021/es0616130. [DOI] [PubMed] [Google Scholar]
- 93.Liu Q, Williams TD, Cumming RI, Holm G, Hetheridge MJ, Murray-Smith R. Comparative aquatic toxicity of propranolol and its photodegraded mixtures: algae and rotifer screening. Environ Toxicol Chem. 2009;28(12):2622–2631. doi: 10.1897/09-071.1. [DOI] [PubMed] [Google Scholar]
- 94.Owen SF, Huggett DB, Hutchinson TH, Hetheridge MJ, Kinter LB, Ericson JF, et al. Uptake of propranolol, a cardiovascular pharmaceutical, from water into fish plasma and its effects on growth and organ biometry. Aquatic Toxicol. 2009;93(4):217–224. doi: 10.1016/j.aquatox.2009.05.009. [DOI] [PubMed] [Google Scholar]
- 95.Giltrow E, Eccles PD, Winter MJ, McCormack PJ, Rand-Weaver M, Hutchinson TH, et al. Chronic effects assessment and plasma concentrations of the beta-blocker propranolol in fathead minnows (Pimephales promelas) Aquatic Toxicol. 2009;95(3):195–202. doi: 10.1016/j.aquatox.2009.09.002. [DOI] [PubMed] [Google Scholar]
- 96.Caldwell DJ, Mastrocco F, Hutchinson TH, Länge R, Heijerick D, Janssen C, et al. Derivation of an aquatic predicted no-effect concentration for the synthetic hormone, 17 alpha-ethinyl estradiol. Environ Sci Technol. 2008;42(19):7046–7054. doi: 10.1021/es800633q. [DOI] [PubMed] [Google Scholar]
- 97.Straub JO, Stewart KM. Deterministic and probabilistic acute-based environmental risk assessment for naproxen for Western Europe. Environ Toxicol Chem. 2007;26(4):795–806. doi: 10.1897/06-212R.1. [DOI] [PubMed] [Google Scholar]
- 98.Hannah R, D’Aco VJ, Anderson PD, Buzby ME, Caldwell DJ, Cunningham VL, et al. Exposure assessment of 17B-ethinylestradiol in surface waters of the United States and Europe. Environ Toxicol Chem. 2009;28(12):2725–2732. doi: 10.1897/08-622.1. [DOI] [PubMed] [Google Scholar]
- 99.United States Fish and Wildlife Services. Secondary pentobarbital poisoning of wildlife. 2012. Available from URL: http://cpharm.vetmed.vt.edu/usfws/usfwsfpentobarbfactsheet.pdf. Accessed Oct 2012.
- 100.LIF. Swedish prescribing guide. 2012. Available from URL: http://www.fass.se/LIF/home/index.jsp. Accessed Jun 2012.
- 101.AstraZeneca. Environmental risk assessment data. 2012. Available from URL: http://www.astrazeneca.com/Responsibility/The-environment/Pharmaceuticals-in-the-environment/era-data-2012. Accessed June 2012.
- 102.Heads of Medicines Agency (HMA). HMA/EMA guidance document on the identification of commercially confidential information and personal data within the structure of the Marketing Authorisation (MA) application: release of information after the granting of a marketing authorisation. European Medicines Agency, 2012. Available from URL: http://www.ema.europa.eu/ema/index.jsp?curl=pages/news_and_events/news/2012/03/news_detail_001478.jsp&mid=WC0b01ac058004d5c1. Accessed 4 Apr 2013.
- 103.Brown AR, Riddle AM, Winfield IJ, Fletcher JM, James JB. Predicting the effects of endocrine disrupting chemicals on healthy and disease impacted populations of perch (Perca fluviatilis) Ecol Model. 2005;189(3):377–395. doi: 10.1016/j.ecolmodel.2005.03.009. [DOI] [Google Scholar]
- 104.Harris CA, Hamilton PB, Runnalls TJ, Vinciotti V, Henshaw A, Hodgson D, et al. The consequences of feminization in breeding groups of wild fish. Environ Health Perspect. 2010;119(3):306–311. doi: 10.1289/ehp.1002555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Roos V, Gunnarsson L, Fick J, Larsson DGJ, Rudén C. Prioritising pharmaceuticals for environmental risk assessment: towards adequate and feasible first-tier selection. Sci Total Environ. 2012;421–422:102–110. doi: 10.1016/j.scitotenv.2012.01.039. [DOI] [PubMed] [Google Scholar]


